To the Editor
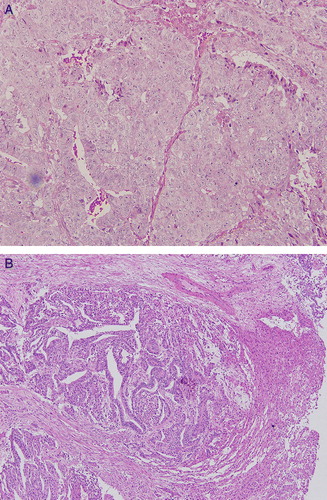
A 3-year-old boy was brought to our hospital for evaluation of enlarged penis and pubic hair. He had no previous medical history and was not receiving any medication. Physical examination showed the genital maturity of penis was Tanner stage III, pubic hair Tanner stage II, but normal testis size. There was abdominal distention and the liver edge was palpable 3 cm below the right costal margin. Laboratory examination revealed normal blood cell counts, liver function tests and lactate dehydrogenase. Results of serology testing were negative for viral hepatitis B and C. The level of serum alpha-fetoprotein (AFP) was 35 534 ng/ml, beta-human chorionic gonadotropin (β-HCG) was 137 mU/ml, and testosterone was 11.1 µg/dl. Computed tomography depicted a multilobular mass measuring 5.5×5.0×3.3 cm in the left lobe of the liver (). Chest CT demonstrated multiple nodules in bilateral lung, which the largest one was 3 cm in diameter. No other tumors were found in further studies. Laparotomy with wedge excision of live mass was performed and the finding revealed the tumor consisted of two different components. Firstly, areas with anastomosing tubules or glands resembling those of a yolk sac tumor were found, with round to oval nuclei with moderate to abundant fine granule cytoplasm. Secondly, cells with primitive-appearing nuclei formed solid aggregates and lined irregular gland-like spaces were seen (). These tumor cells showed focal immunoreactivity for CD 30, AFP, and placental alkaline phosphatase but not for β-HCG, EMA, hepatocyte, cytokeratin 7 and 20. There were no hepatocellular carcinoma or hepatoblastoma features. Based on the clinical features, histological findings and immunohistiochemical stains, a primary germ cell tumor (GCT) of the liver with mixed components of embryonal carcinoma and yolk sac tumor was diagnosed. Chemotherapy was subsequently initiated using VBPE protocol, which included vinblastin, bleomycin, cisplatin, and etoposide every 3 weeks. After three cycles of chemotherapy, the lung lesions all disappeared and the size of liver tumor decreased. Subsequently, the liver mass was totally resected. The pathological result demonstrated massive necrosis without residual tumor. Thereafter, the boy was treated with another two courses of the regimen. He was disease-free during 8 years of follow-up.
Figure 2. A. Cells with primitive-appearing nuclei forming solid aggregates and lining irregular gland-like space. B. Anastomosing tubules or glands surrounded by fibrous stroma; round to oval nuclei with moderate to abundant fine granules cytoplasma.
Extragonadal GCTs account for only 1 to 5% of all GCTs Citation[1], Citation[2]. They arise as a result of malignant transformation of residual germinal components that abnormally migrate during embryogenesis. They are mainly located along the midline of the body, including pineal gland, mediatinum, retroperitoneal and sacrococcygeal regions. Extragonadal GCTs rarely develop in the visceral organs. Within the liver, they are extremely rare Citation[3–5]. These tumors frequently consist of different pathological components such as yolk sac tumors, choriocarcinoma and teratoma, and most patients die as a result of disease despite the use of aggressive therapeutic strategies. Fortunately, our patient had good response to chemotherapy. Since knowledge of this rare type of liver tumor is limited, further characterization of the biologic and pathological features of the tumor is needed to better understand its clinical behavior.
References
- Bokemeyer C, Nichol CR, Droz JP, Schmoll HJ, Horwich A, Gerl A, et al. Extragonadal germ cell tumors of the mediastinum and retroperitoneum: results from an international analysis. J Clin Oncol 2002; 20: 1864–73
- Scholz M, Zehender M, Thalmann GN, Borner M, Thoni H, Studer UE. Extragonadal retroperitoneal germ cell tumor: Evidence of origin in the testis. Ann Oncol 2002; 13: 121–4
- Toumi N, Chaumette-Plankaert MT, Cherqui D, de Revel T, Duvillard P, Theodore C. Primary yolk sac tumor of the liver. J Clin Oncol 2004; 22: 1756–8
- Theegarten D, Reinacher A, Graeven U, Philippou S. Mixed malignant germ cell tumour of the liver. Virchows Arch 1998; 433: 93–6
- Wong NA, D'Costa H, Barry RE, Alderson D, Moorghen M. Primary yolk sac tumour of the liver in adulthood. J Clin Pathol 1998; 51: 939–40