To the Editor
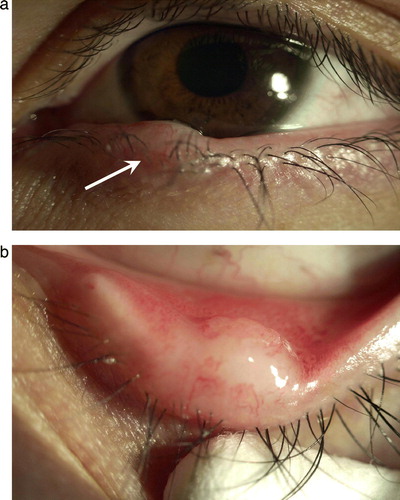
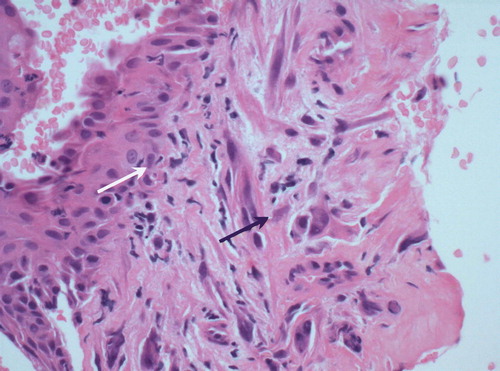
A 29-year-old Hispanic male with an unremarkable past medical history, was diagnosed with a mediastinal germ cell tumor (GCT) of mixed histology including choriocarcinoma, embryonal carcinoma and teratomatous components. At the time of diagnosis the human chorionic gonadotropin (HCG) was 287 IU/l [normal range ≤2], alpha-fetoprotein (AFP) 421 µgr/l [normal range ≤5] and LDH 215 IU/l [normal range ≤190]. No testicular primary or other metastasic sites were observed. The patient received treatment with a combination of bleomycin, etoposide and cisplatin [BEP] for four cycles achieving a normalization of the tumoral markers but only a mild reduction of the tumor volume. Shortly afterwards due to radiological progression, an R0 resection of the mediastinal mass was performed. Pathologic examination revealed a mixed histology with mature teratoma, gastrointestinal adenocarcinoma and sarcoma components together with extensive areas of fibrosis and necrosis. Two months later, the patient relapsed presenting with multiple pulmonary nodules and one suspicious liver lesion. A hepatic biopsy confirmed the diagnosis of teratoma with malignant transformation in keeping with sarcoma. The patient was then treated with a combination of vinblastine, ifosfamide and cisplatin (VeIP) with no response after two cycles. During treatment course he presented with a painless small nodule on his left inferior eyelid measuring around 8 mm (a and b). A biopsy of this nodule () revealed areas of normal conjunctiva (white arrow) along with sarcomatoid components (black arrow) in keeping with metastatic sarcoma. Further systemic treatment options were discussed with the patient who rejected any active approach. To date, four months after diagnosis of this metastasis, the patient remains clinically stable with no symptoms.
Though GCTs account for only 1–2% of all human malignancies they are the most common tumors diagnosed in men ages 15 to 34 years Citation[1]. Only 10% of GCTs present as extragonadal malignancies arising in the mediastinum, retroperitoneum and central nervous system in order of frequency. The biology of GCTs is unique having the capacity to display totipotential differentiation ranging from embryonal carcinoma to extraembryonic cell types (i.e. yolk sac tumor or choriocarcinoma) or to somatic cell types (i.e. teratoma) Citation[2]. Teratomas are tumors that display somatic elements with diverse differentiation stages (i.e. mature and immature teratomas). On rare occasions the teratomatous component in a GCT may undergo malignant transformation leading to histology indistinguishable from a somatic malignancy. Examples of histologic transformed cell types include rhabdomyosarcoma, primitive neuroectodermal tumor [PNET], enteric adenocarcinoma and leukemia. This phenomenon, known as teratoma with malignant transformation (TMT), may occur in GCTs from any primary site but it is seen more often in mediastinal tumors. No clinical characteristics are unique to this condition and in most of the cases the diagnosis is made incidentally at the time of surgery. It has been reported that malignant transformation in to adenocarcinoma tends to occur after long latent intervals compared with other histologies [i.e. sarcoma, PNET or leukemia]. In overall the prognosis of patients with TMT is poor with a recurrence rate of up to 86% and an overall survival rate of only 58–65% Citation[3], Citation[4]. Patients with mediastinal tumors, neural or rhabdomyosarcomatous differentiation and distant metastases usually have the worst prognosis Citation[5]. The management of this condition in the metastatic setting still remains controversial. Traditionally TMTs have been considered as chemo resistant malignancies, however recent data suggest that systemic chemotherapy may be effective when the treatment choice is based on the transformed histology in a minority of patients Citation[2]. The spreading pattern of these tumors usually involves lungs, liver and bones. Eyelids metastases have been rarely described in association with germ cell tumors. Eye metastases have been described extensively in other tumor types (i.e. breast, lung and gastrointestinal carcinomas) Citation[6]. However, there have been only a few reports describing eye metastases from GCTs being most of the cases intraocular metastases with a choriocarcinoma histology Citation[7–9]. To our knowledge this is the second case in the literature of a TMT that presents as an eyelid metastasis Citation[10].
References
- Bosl GJ, Motzer RJ. Testicular germ-cell cancer. N Engl J Med 1997; 337: 242–53
- Donadio AC, Motzer RJ, Bajorin DF, Kantoff PW, Sheinfeld J, Houldsworth J, et al. Chemotherapy for teratoma with malignant transformation. J Clin Oncol 2003; 21: 4285–91
- Ahmed T, Bosl GJ, Hajdu SI. Teratoma with malignant transformation in germ cell tumors in men. Cancer 1985; 56: 860–3
- Little JS, Jr, Foster RS, Ulbright TM, Donohue JP. Unusual neoplasms detected in testis cancer patients undergoing post-chemotherapy retroperitoneal lymphadenectomy. J Urol 1994; 152: 1144–9
- Comiter CV, Kibel AS, Richie JP, Nucci MR, Renshaw AA. Prognostic features of teratomas with malignant transformation: A clinicopathological study of 21 cases. J Urol 1998; 159: 859–63
- Ferry AP, Font RL. Carcinoma metastatic to the eye and orbit. I. A clinicopathologic study of 227 cases. Arch Ophthalmol 1974; 92: 276–86
- Lahav M, Berkowitz S, Albert DM. Primary mediastinal choriocarcinoma in a male metastatic to the choroid. Albrecht Von Graefes Arch Klin Exp Ophthalmol 1978; 206: 191–7
- Barondes MJ, Hamilton AM, Hungerford J, Rustin GJ. Treatment of choroidal metastasis from choriocarcinoma. Case report. Arch Ophthalmol 1989; 107: 796–8
- Zech JC, Subiger L, Chiquet C, Bouvier R, Trepsat C. Testicular choriocarcinoma metastatic to the choroid. Retina 1999; 19: 164–5
- Ham JA, Carr NJ. Testicular cancer presenting as a red swollen lid. Br J Ophthalmol 1988; 72: 868–70