To the Editor
The current recommendations for the treatment of acute promyelocytic leukemia (APL) include all-trans-retinoic acid (ATRA) and anthracycline-based chemotherapy Citation[1]. This combination therapy results in long-lasting remission in up to 70% of newly diagnosed patients with APL Citation[2]. ATRA is usually well tolerated but it has some side effects, the most severe of which is retinoic acid (RA) syndrome. Here we described a patient with APL who developed atypical presentation of RA syndrome which was confused with septic arthritis initially.
Case report
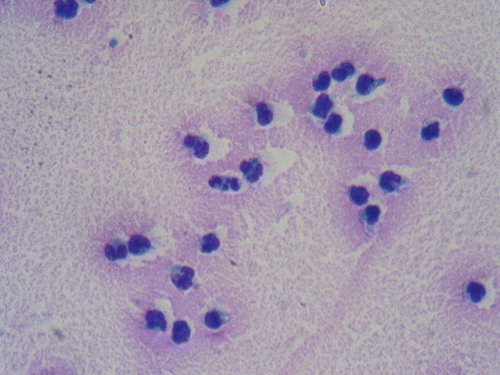
A 72-year-old woman presented with generalized malaise, cutaneous ecchymoses and weakness. The initial laboratory evaluation revealed pancytopenia with a leukocyte count of 0.7×109/l, a hemoglobin level of 8.3 g/dl and a platelet level of 23×109/l. Bone marrow was nearly totally replaced by hypergranulated blasts with auer rods. Flow cytometry analysis of bone marrow showed that blasts were positive for CD 13 and CD33 and negative for HLA DR expression. Diagnosis of APL was confirmed by demonstration of t(15;17) with chromosomal analysis and PML/ RARα rearrangement by reverse transcriptase polymerase chain reaction (RT-PCR). She received remission induction therapy with idarubicin 12 mg/m2/day on days 2, 4, 6 for 3 days and ATRA 45 mg/m2/day from day 1 onwards. On the 9th day of ATRA, she developed fever, pain and swelling of the right knee joint. On physical examination right knee joint was extremely painful, tender, warm and swollen. Effusion was detected by ballottement on patella. Septic arthritis was suspected from the symptoms and the physical examination. Morphologic examination of synovial fluid showed infiltration of mature myeloid cells and occasional promyelocytes (). Gram stains, bacterial and fungal cultures of synovial fluid were negative. On the 11th day of the ATRA white blood cell count (WBC) increased to 14×109/l despite chemotherapy. Two days later dyspnea and pleural effusion occured. With the suspicion of RA syndrome, ATRA was stopped and dexamethasone at a dose of 10 mg twice daily intravenously was initiated. After cessation of ATRA and initiation of dexamethasone, all the clinical symptoms resolved. Then ATRA was reintroduced and given for 45 days. ATRA syndrome did not recur. At the end of the induction therapy complete remisssion was achieved.
Discussion
The most serious complication of ATRA is RA syndrome which is characterized by fever, weight gain, respiratory distress, lung infiltrates, pleural or pericardial effusion, hypotension and renal failure in the absence of any other cause Citation[3–5]. Its incidence is 15–26% Citation[4], Citation[5]. Clinical signs usually develop after 2 to 21 days of treatment. The exact mechanism responsible for RA syndrome is still poorly understood. Changes in cytokine secretion including interleukin (IL) 1β, IL-6, IL-8 and TNF-α and adhesive qualities of APL cells that result in leukemic cell- endothelial cell adhesion followed by extravasation has been suggested to play a role for development of RA syndrome.
Because diagnosis of RA syndrome is purely clinical, it may be difficult to distinguish from other complications of disease. Here we reported an atypical presentation of RA syndrome that was confused with septic arthritis initially. Effusion was aspirated by arthrocentesis to rule out infectious arthritis in our severely neutropenic patient. Negative gram stains and cultures of synovial fluid, heavily infiltration of synovial fluid with mature myeloid cells and occasional promyelocytes, development of dyspnea and pleural effusion in addition to fever, synovial fluid and increase in WBC with immature myeloid cells despite the chemotherapy made us to consider RA syndrome. Improvement of dyspnea and pleural effusion together with all manifestations of joint and fever after withdrawal of ATRA and induction of dexamethasone confirmed the diagnosis of RA syndrome. Interstitial infiltration of myeloid cells with pleural or pericardial effusion is a common finding of RA syndrome but infiltration of synovium with synovial effusion is uncommon. Early recognition and prompt institution of treatment is important especially for patients with atpical presentation of RA syndrome as seen in our patient.
References
- Sanz MA, Martin G, Gonzalez M, Leon A, Rayon C, Rivas C, et al. Risk-adapted treatment of acute promyelocytic leukemia with all-trans-retinoic acid and anthracycline monochemotherapy: A multicenter study by the PETHEMA group. Blood 2004; 103: 1237–43
- Sanz MA, Lo Coco F, Martin G, Avvisati G, Rayon C, Barbui T, et al. Definition of relapse risk and role of nonanthracycline drugs for consolidation in patients with acute promyelocytic leukemia: A joint study of the PETHEMA and GIMEMA cooperative groups. Blood 2000; 96: 1247–53
- Avvisati G, Tallman MS. All-trans retinoic acid in acute promyelocyctic leukemia. Best Pract Res Clin Haematol 2003; 16: 419–32
- De Botton S, Dombret H, Sanz M, Miguel JS, Caillot D, Zittoun R, et al. Incidence, clinical features and outcome of all trans-retinoic acid syndrome in 413 cases of newly diagnosed acute promyelocytic leukemia. The European APL Group. Blood 1998; 92: 2712–8
- Tallman MS, Andersen JW, Schiffer CA, Appelbaum FR, Feusner JH, Ogden A, et al. Clinical description of 44 patients with acute promyelocytic leukemia who developed the retinoic acid syndrome. Blood 2000; 95: 90–5