To the Editor
Pituitary Adenoma Neuronal CHoristoma (PANCH syndrome) is a rare pathological entity of pituitary with unknown clinical impact.
Case history
Pituitary adenomas are common benign brain tumours that are easily diagnosed on biopsy specimens by typical morphological features. However, rarely, they may have divergent differentiation, necessitating the use of immunohistochemistry (IHC) for better characterization.
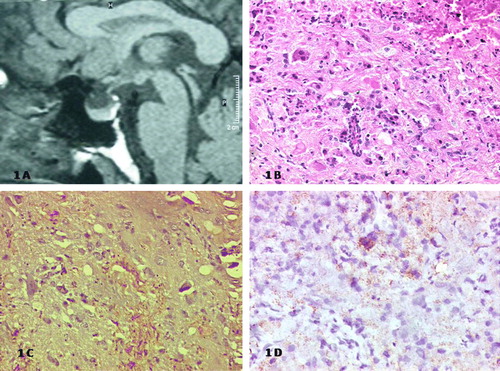
A 43-year-old lady presented with progressive weight gain, enlargement of extremities and hirsutism of 2 years duration. MRI scan showed focal enlargement of the pituitary gland suggestive of a macroadenoma (). There was no mass effect on the optic pathway and her endocrine profile was normal (T3-2.5 nmol/l, T4-129.1 nmol/l, TSH-0.24 mIU/ml, Prolactin-4.48 ng/ml, GH-2.15 ng/ml, and Cortisol-5.45 ug/dl). She underwent trans-sphenoidal excision of the lesion via a sublabial, rhinoseptal approach with uneventful post-operative recovery. Conventional light microscopy suggested pituitary adenoma with extensive neuronal metaplasia (Figure 2). On IHC, the tumor had cytokeratin (CK), glial fibrillary acidic protein (GFAP), and synaptophysin positivity highlighting the adenoma component, gliofibrillary background, and metaplastic neuronal cells respectively (Figure 3a,b). The overall picture was suggestive of ‘Pituitary Adenoma Neuronal CHoristoma’ syndrome. As there was no residual disease on imaging, and the lesion essentially non-secretory, she was kept on surveillance imaging. She had significant symptom relief following surgery and continues to remain asymptomatic on follow-up.
Figure 1. A) Sagittal T1 weighted non-contrast MRI showing hypointense lesion in the pituitary; B) Conventional light microscopy (H & E) of the lesion showing pituitary epithelial cells admixed with bipolar ganglion cells in a glial background (×10); C) Photomicrograph showing synaptophysin positivity D) and background GFAP staining suggestive of glio-neuronal differentiation (×10)
Discussion
The differential diagnoses of pituitary adenoma include a variety of intracranial neoplasms that arise in the sellar-suprasellar region such as pilocytic astrocytoma, craniopharyngioma, ganglioglioma, neurocytoma and germ cell tumours Citation[1]. These tumours arise from diverse cellular lineages and have different management principles and prognosis. PANCH is a rare tumour in this region of uncertain cellular origin Citation[2]. Histogenesis of glial and neuronal metaplasia in pituitary adenomas has been debated Citation[3] suggesting that they arise from embryonal pituitary cell rests or have common hypothalamic origin. It is also hypothesized that sparsely granulated growth hormone (GH) producing adenoma cells can differentiate to the neuronal lineage Citation[4]. Morphologically, the tumour is composed of chromophobe pituitary adenoma with varying ganglionic/neuronal component with or without neuropil.
PANCH has been described only as isolated reports or small case series (), with vast majority being hormone secreting pituitary tumours with consequent increase in serum hormone levels Citation[6], Citation[7], Citation[10]. GH and adrenocorticotropic hormone secreting tumours have a tendency towards glial differentiation Citation[3], Citation[5], Citation[9]. They usually present with intracellular inclusion bodies like Crooke's hyaline change. Only few non-secretory PANCH syndrome cases have been reported including this one.
Table I. Literature review of glioneuronal differentiation of pituitary tumour (PANCH).
As in other pituitary tumours, surgery is the cornerstone of management of these tumours. Completely excised tumours, with no evidence of residual tumour on post-operative imaging, should be kept on close observation. In patients with gross residual disease, or progression on surveillance imaging, not amenable to further safe resection, definitive radiotherapy should be offered to improve outcome.
In summary, non-secretory pituitary adenoma presenting with glioneuronal differentiation (PANCH) is an extremely rare entity with an unknown clinical course.
References
- Halbauer J, Mészáros I, Dóczi T, Kajtár P, Pajor L, Kovács K, et al. Rare sellar region tumors. Pathol Oncol Res 2003; 9: 134–7
- Saeger W, Lüdecke DK, Losa M. Combined neuronal and endocrine tumors of the sellar region. Pathologe 1997; 18: 419–24
- Horvath E, Kovacs K, Scheithauer BW, Lloyd RV, Smyth HS. Pituitary adenoma with neuronal choristoma (PANCH): Composite lesion or lineage infidelity?. Ultrastruct Pathol 1994; 18: 565–74
- Baysefer A, Gezen F, Kayali H, Erdo(an E, Timurkaynak E, Celasun B. Intrasellar gangliocytoma resembling pituitary adenoma. Minim Invasive Neurosurg 1997; 40: 107–9
- Puchner MJ, Lüdecke DK, Saeger W, Riedel M, Asa SL. Gangliocytomas of the sellar region–a review. Exp Clin Endocrinol Diabetes 1995; 103: 129–49
- Sharma MC, Karak AK, Mahapatra AK, Sarkar C. Pituitary adenoma with neuronal choristoma: A report of two rare cases. Clin Neurol Neurosurg 1999; 101: 128–32
- Kurosaki M, Saeger W, Lüdecke DK. Intrasellar gangliocytomas associated with acromegaly Brain Tumor Pathol 2002; 19: 63–7
- Kontogeorgos G, Mourouti G, Kyrodimou E, Liapi-Avgeri G, Parasi E. Ganglion cell containing pituitary adenomas: Signs of neuronal differentiation in adenoma cells. Acta Neuropathol 2006; 112: 21–8
- Nasr C, Mason A, Mayberg M, Staugaitis SM, Asa SL. Acromegaly and somatotroph hyperplasia with adenomatous transformation due to pituitary metastasis of a growth hormone-releasing hormone-secreting pulmonary endocrine carcinoma. J Clin Endocrinol Metab 2006; 91: 4776–80
- Serri O, Berthelet F, Bélair M, Vallette S, Asa SL. An unusual association of a sellar gangliocytoma with a prolactinoma. Pituitary 2008; 11: 85–7
