To the Editor,
The treatment of children with cancer by radiotherapy differs from that of adults. One important difference is that most of the children are cured and become long-term survivors. The overall survival of children with cancer (all forms) in Sweden in 2003 was approximately 80% Citation[1]. A successive increase in survival has been achieved by progress in surgery, chemotherapy and radiotherapy, and perhaps most importantly, the implementation of intensified multimodal treatment including supportive care, together resulting in better treatment outcome.
Late side effects of radiotherapy are often more severe after treatment of a growing child and differ in nature from those in adults, mainly growth retardation. Cancer survivors will have to cope with these late effects for the rest of their lives. It is therefore of utmost importance to optimise the treatment in each individual case, regarding both tumour response and adverse side effects.
Fortunately, the incidence of cancer requiring radiotherapy in children is low. However, this makes it more difficult to maintain a high level of competence amongst the staff working with these patients. Approximately 120 children in Sweden receive radiotherapy each year Citation[2]. Paediatric radiotherapy is presently available at the University Hospitals in Gothenburg, Linköping, Lund, Stockholm, Umeå and Uppsala. Between 10 and 30 children are treated annually at these centres.
A Swedish working group, consisting of physicians and medical physicists, collaborating on matters concerning treatment of children with radiotherapy, was formed seven years ago. The members of this group are also active in other working groups dealing with issues regarding childhood cancer. The “Swedish Workgroup for Paediatric Radiotherapy” is fairly small, including only one or two physicians (together with a few medical physicists) from each university hospital. The group meets twice a year to discuss issues regarding treatment protocols, quality assurance, further education, clinical research and long-term follow-up. Individual patient cases are also reviewed at these meetings.
The use of telemedicine techniques including video conferencing was considered as a means of establishing more formal and regular contact while, at the same time, bridging the long physical distances between the university hospitals involved. Similar systems for radiotherapy collaboration have already been introduced in Europe Citation[3–8], Asia Citation[9], Citation[10] and across the Atlantic Citation[11]. In France, a similar network for on-line conferences regarding paediatric radiotherapy was recently started between several centres Citation[12]. In other areas of health care telemedicine projects have reported great success with similar constellations, for example in cardiology Citation[13], radiology Citation[14], oncology Citation[15] and the retinoblastoma collaboration between a hospital in Jordan and two hospitals in USA Citation[16].
The aim of the project was to keep and/or raise the competence level within the group of specialists as well as distributing this competence more widely in the participating centres as they see more cases and to act as discussion partners and support in difficult decisions.
In this paper we report the implementation of a telemedicine conferencing system including collaboration on radiation treatment plans for paediatric radiotherapy. The different phases from idea, expectations, requirements and evaluation to clinical practice are covered.
Project initiation phase
The project was initiated from within the group since the need for more frequent and regular contact to discuss individual cases became apparent. It usually took place on an informal basis via phone calls. This form of communication was, however, found to be inadequate.
We started the project with a thorough investigation of the clinical and technical expectations and requirements.
Clinical expectations and requirements
Specialists in paediatric radiotherapy were interviewed in order to determine their level of interest in and expectations of the project. A needs analysis model was used for the interviews Citation[17], Citation[18]. This is a model used to collect data for estimating the needs of a working group. It is useful when a new policy or change is being implemented, as well as after it has been taken into operation. It often uses interviews or questionnaires as a mean to collect data. We considered it important to obtain the views of the specialists on the proposed telemedicine project, as well as to encourage them to participate. The interviews were structured with open answers. At the time of the interviews nine specialists in paediatric radiation oncology were active in their department (one centre with three specialists, one centre with two specialists and four centres with one specialist). One of the specialists declined to be interviewed. All interviews were taped and then compiled and analysed by the same person who made the interviews.
The questions were designed to obtain information on the background of the specialists, their clinical setting and their needs and wishes regarding a conference system. The questions also dealt with the possible gains in education and experience. They were also asked if they thought that problems encountered in the clinic concerning radiotherapy in children could be solved by the introduction of a video conference system. The questions were divided into four areas; “background”, “needs”, “learning” and “technique”. The interviews were read through several times, and the answers could then be grouped into content areas. Within each content area subgroups were found. This process is described by Graneheim and Lundgren Citation[19] as finding the manifest content of the text. The unit of analysis is the whole interview, from this meaning units are found, these are answers relevant for the question asked. These meaning units are coded (or categorized) to find the manifest content. The results of the interviews were used to define the clinical expectations and requirements. They also gave some indication of the kind of technical solution required.
The background of the interviewed specialists told us that; the paediatric radiotherapy experience in the group varied from one year to 20 years. They expected the number of paediatric cases to vary from ten per year to 25 per year in their respective centre. They meant that between half to two thirds of their cases would be worth presenting at a national conference. Three women and five men were interviewed. They all claimed to have time to participate.
The question, “What needs can be satisfied with a system like this?” resulted in answers that were grouped into the following six categories, by analysis of content: experience/competence, learning, discussion of individual patient cases, support/new ideas, development of common guidelines, and quality control. Most important was the possibility to increase the experience and raising the competence both individually and as a group. Six of eight participants highlighted this specifically. Equally important was the discussion of individual patient cases (5/8) and support and new ideas (5/8). The development of new protocols or common guidelines also came up as important (4/8). Quality control of treatments and difficulties in interpretation of study protocols were also mentioned. There would then be an advantage of getting the others’ view.
On the technical side the possibility to view treatment plans and diagnostic images (7/8) topped the list, together with good audio and image quality (6/8). Inviting others to participate, like paediatric oncologists, also came up as being important, however, not until the primary group felt comfortable with the conferencing.
The group was on the whole very positive to the project, but also mentioned the importance of patient confidentiality and the fact that the workload for the individual specialist shouldn't increase.
Technical requirements and solution
The technical requirements were investigated regarding demands on both software and hardware. As some of the hospitals already had reliable, well-established video conferencing equipment we were required to find equipment that was readily available and reasonably priced for those who did not.
The network
All hospitals in Sweden are connected via a secure intra-hospital IP network which forms the basic framework for the conferencing system. Sjunet (www.carelink.se) is a national broadband communication network separated from the Internet, and its use for the transmission of identified patient information has been declared safe and legal. It is a protected VLAN (virtual LAN). The Swedish county councils, local authorities, several private caregivers and several suppliers (e.g. the national pharmacy) are connected to Sjunet (). The network is managed by Carelink, an organisation in which the above mentioned organisations are members. The members can choose the bandwidth they wish to subscribe to depending on their needs, from 4 Mbps up to 1000 Mbps full duplex. Apart from video conferences and IP telephony, many other applications are run via Sjunet, such as the transfer of electronic prescriptions to local pharmacies, x-ray images or ultrasound images from a smaller hospital to university hospitals for diagnostic purposes, and data for long-distance EKG supervision.
Local facilities
A connection to Sjunet and a connection through the local firewall, somewhere physically close to the radiotherapy department, are needed in each hospital. Four of the six university hospitals already used a variety of video conferencing systems at the start of the project. The other two invested in personal conferencing systems.
Common to all systems is the ability to communicate sound and live images. Two examples of the web conferencing systems in use are those supplied by Tandberg (http://www.tandberg.com) and Polycom (http://www.polycom.com), installed in a conference room with separate screens for video conferencing and applications. Another system in use is a personal conference system using vPoint HD supplied by VCON (http://www.vcon.com), which is installed on a desktop together with a web camera and a headset or microphone. These different systems all function together, and can use the conference bridge in Sjunet.
Common facilities
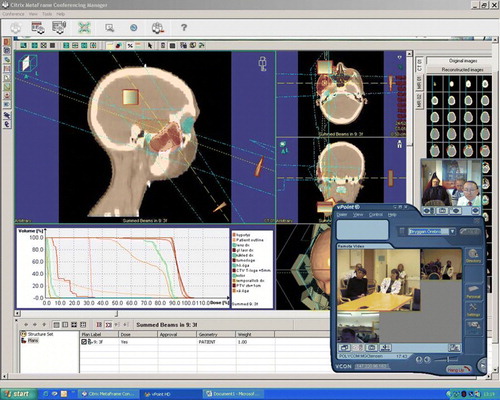
For application-sharing purposes, a dedicated server (a Windows 2003 server with dual 3.2 GHz Intel Xeon CPUs, 4 GB RAM) has been installed. The application-sharing software used is Citrix MetaFrame Presentation XP Server 3.0 and Citrix MetaFrame Conferencing Manager 3.0. The main application software installed on the server, i.e. the DICOM RT-viewer, is Oncentra MasterPlan version 1.5 SP1 (Nucletron Scandinavia AB, Sweden). Other software packages installed are Microsoft Office and Adobe Acrobat Reader.
The conference bridge in Sjunet is hired for the time slot needed for conferences (approx. 1 hour, every two weeks). The bridge can handle calls from conference systems as well as calls from an ordinary telephone, should it be necessary. The standards used are H.323 for IP video conference communication and H.320 for ISDN video conference communication.
RT viewing
Oncentra MasterPlan was chosen as RT-viewer due to its ability to import and show treatment plans from TPSs supplied by other vendors. Of the six hospitals involved, three use MasterPlan and three uses Varian Eclipse (Varian Medical Systems, Inc. USA) in clinical routine.
Plans are exported in DICOM-RT format Citation[20] from the treatment centre to the server, and subsequently viewed in the “Plan Analysis” (PA) module of the TPS. The PA module allows complete treatment plans to be viewed, i.e. images, structures, beams, beam shapes, dose distributions and dose volume histograms for photons with no need for specific treatment machine configuration data. If patient data are exported for target discussions only, and there is no plan, the target module of the software can be used instead of the PA module.
All parameters in the plan can be viewed in the PA module. Tools used in the PA module are dose volume histograms, “tiled” plan and dose distribution comparisons, live dose calculations (which allow the user to move the pointer in the volume of interest and have the dose displayed next to the pointer), dose intervals (hot spots and cold spots) and viewing of images from different imaging modalities (CT, MR and PET).
Routines
A number of routines are followed prior to and during the conferences to make them efficient.
E-mail reminders are sent to all participants approximately one week in advance.
The treatment planning staff at the local centre prepares and exports patient cases.
The local physician sends a short description of the case to the others in the group.
The patient case is imported into the TPS on the server.
All participants connect to the virtual “conference room” and a computer in the local conference room connects to the Citrix server.
Target volumes, treatment plans and diagnostic images, if available, are viewed and discussed ().
After the conference all patient data are erased from the server.
Project evaluation after one year
Clinical video conferences started in November 2005 with conferences held every other week.
The interviews were repeated, with the same respondents and interviewer, one year after the start of the conferences. The purpose was to determine the participants’ experience of the conferences, both the clinical value and the technical status. The questions were focused on the experience the group had made during the first year. They were analysed in the same way as the initial interviews.
The group felt that the conferences did have a significant impact on experience/competence (7/8). The discussion of individual patient cases was rated equally important (7/8). Again support and new ideas were mentioned (3/8) as a rise in quality (1/8).
From a technical point of view most wishes had been fulfilled. There was total agreement in the benefit of viewing treatment plans and diagnostic images (8/8). However the audio quality has, during periods, been poor (6/8).
Future wishes expressed by the participants at the time of the second interview were:
More cases should be submitted and discussed.
More information on the cases should be submitted prior to the conference.
It should also be possible to view the plans prior to the conference.
It should be possible to view proton treatment plans.
All centres should be encouraged to participate in every conference.
Experience and future aspects
We have so far had 45 conferences, discussing on average 2.9 cases per conference, with a range of zero to six cases (SD = 1.58). On average, four of the six hospitals have been connected at each conference, with a range of three to six participating hospitals. During 2008 Copenhagen has been added to the group and participates frequently. Approximately 30–60 minutes were spent on each conference. The coordinator spends an additional 1–2 hours in connection to each conference importing, preparing and then deleting the cases submitted. The participants of the Swedish Workgroup for Paediatric Radiotherapy are, in general, positive to the results obtained with the web conference system. They stress the advantages of seeing more patient cases than they would normally do, and the possibility of discussing patient cases and obtaining advice from the other members of the group in especially “difficult” cases. In general, the conferences are regarded as a concept that works well. The meeting frequency, bi-weekly, also seems to be appropriate at the moment. It is of course possible to call extra conferences if needed, but so far this option has not been exploited. One hospital has not yet submitted any patients to any of the conferences. It is our goal that all new cases of proposed paediatric radiotherapy in Sweden be seen and discussed. There was an increase in the number of submitted patient cases, as well as participating hospitals, during 2007. The method used, to interview the specialists and from their answers draw conclusions on needs and wishes can of course be debated. The results can be biased from the specialists’ side; they knew about the plans, and were in part themselves initiators of the project. The result can also be biased from the interviewer's side, who is also the coordinator of the project, and thereby wanting “compliance”.
The difficulties encountered have mainly been on the technical side. Some centres have had problems getting through hospital fire walls and obtaining help from local IT departments. Another major problem has been the audio quality of the conferences. There may be two reasons for this problem: 1) the broadband of a particular region may not have sufficient bandwidth to support the traffic, which is becoming more and more intense, and/or 2) the PC-based systems may not correct the quality of the sound in the same way as the dedicated video conferencing systems. This is, however, changing since the participating hospitals are now investing in dedicated systems and conference rooms .
Initially, wishes were expressed for both portal images and morphological images, but so far there have been no requests for either of these. However, both types of images can be imported into the RT viewer if required. During the first few conferences we could not show dose distributions from Varian Eclipse treatment plans, but this was solved by Nucletron.
In the future, showing two (or more) treatment plans for the same patient next to each other could be very useful for comparing plans with different modalities, e.g. IMRT vs. 3D-CRT or photons vs. protons. This is technically already possible with the present RT viewer. The current proton planning software used is not DICOM-RT compatible and instead of using the PA module, we have to use screen dumps in PDF documents for viewing proton plans. Proton treatment in Sweden is today administered at The Svedberg Laboratory in Uppsala. Energy, field size and patient positioning are limiting the use of the facility. There are far-reaching plans of a national gantry based proton facility in Sweden. One of its cornerstones is and will be “distributed competence” for which the here described project can be seen as a pilot test of its feasibility Citation[21].
We foresee other possibilities with the conference system, such as:
inviting paediatric medical and radiation oncologists in training or other colleagues to participate in the conferences,
using the conferences for quality control/feedback in ongoing studies, including collaboration with European study centres,
using the system (or similar systems) to develop competence within a specific field and/or patient group, e.g. treatment with protons/light ions.
Such a system can also be used for improving and conforming the segmentation of target volumes. We have performed a dummy run for target delineation according to a new European protocol for the treatment of Hodgkin's lymphoma in children. It was performed to see how well the protocol was understood and what differences occurred.
We use each other's knowledge, experience and suggestions regarding treatment but the decisions regarding the treatment of individual patients lie in the hands of the local treating physician. The fact that patient data are exported to the dedicated server also makes this clear. There is no intrusion in clinical databases, nor are changes made to data concerning patient treatment in any of the participating hospitals’ clinical databases. No data are saved in the dedicated system, nor do we keep record of changes arising from discussions during the conferences. The responsibility and any decision to change treatment are made solely at the local centre.
In the future, other groups can maintain and improve competence in many fields at centres treating patients from small patient groups with the aid of telemedicine. This will be of great value for those patients who can be treated at a centre near their home, but with a procedure based of the common knowledge and experience of all the participating centres.
Acknowledgements
We would like to thank the Swedish Workgroup for Paediatric Radiotherapy for their cooperation, willingness to be interviewed and their support of the project, Mats Johansson, Magnus Jälmbrant and Thomas Molén in Umeå for their technical knowledge and support, and Per Ekström at Nucletron Scandinavia AB, for his belief in the project and for help with the software. The project was supported by The Swedish Children's Cancer Foundation, Lund University Hospital Research Funds, and Västerbottens Läns Landsting Research Funds.
References
- Cancer i siffror. Socialstyrelsen och Cancerfonden. 2005.
- Bjork-Eriksson T, Ask A, Glimelius B. The potential of proton beam therapy in paediatric cancer. Acta Oncol 2005; 44: 871–5
- Norum J, Bruland ØS, Spanne O, Bergmo T, Green T, Olsen DR, et al. Telemedicine in radiotherapy: A study exploring remote treatment planning, supervision and economics. J Telemed Telecare 2005; 11: 245–50
- Olsen DR, Bruland ØS, Davis BJ. Telemedicine in radiotherapy treatment planning: requirements and applications. Radiother Oncol 2000; 54: 255–9
- Björeland A, Blomquist M, Sätherberg A, Bergström P, Karlsson M, Franzén L. Joint Center – samarbetsprojekt för optimal strålbehandling i närmiljö. Läkartidningen 2004;101:472–5. (In Swedish)
- Kristensen I, Johansson M, Lind J, Nilsson P, Karlsson M. Barnradioterapi på distans. Läkartidningen 2006;103:1188–90. (In Swedish)
- Gomez A, Fernandez Sanchez C, Mouriño Gallego JC, Gonzalez Castaño FJ, Rodriguez-Silva D, Pena Garcia J, et al. Remote radiotherapy planning: The eIMRT project. Stud Health Technol Inform 2006; 120: 330–5
- Eich HT, Müller RP, Schneeweiss A, Hansemann K, Semrau R, Willich N, et al. Initiation of a teleradiotherapeutic network for patients in German lymphoma studies. Int J Radiat Oncol Biol Phys 2004; 58: 805–8
- Huh SJ, Shirato H, Hashimoto S, Shimizu S, Kim DY, Ahn YC, et al. An integrated service digital network (ISDN)-based international telecommunication between Samsung Medical Center and Hokkaido University using telecommunication helped radiotherapy planning and information system (THERAPIS). Radiother Oncol 2000; 56: 121–3
- Datta NR, Rajasekar D. Improvement of radiotherapy facilities in developing countries: A three-tier system with a teleradiotherapy network. Lancet Oncol 2004; 5: 695–8
- McAleer JJ, O'Loan D, Hollywood DP. Broadcast quality teleconferencing for oncology. Oncologist 2001; 6: 459–62
- Carrie C. personal communication 2007.
- Boriani G, Diemberger I, Martignani C, Biffi M, Valzania C, Bertini M, et al. Telecardiology and remote monitoring of implanted electrical devices: The potential for fresh clinical care perspectives. J Gen Intern Med 2008; 23(Suppl 1)73–7
- Boland GW. Teleradiology coming of age: Winners and losers. AJR Am J Roentgenol 2008; 190: 1161–2
- Stalfors J, Edström S, Björk-Eriksson T, Mercke C, Nyman J, Westin T. Accuracy of tele-oncology compared with face-to-face consultation in head and neck cancer conferences. J Telemed Telecare 2001; 7: 338–43
- Qaddoumi I, Nawaiseh I, Mehyar M, Razzouk B, Haik BG, Kharma S, et al Team management, twinning, and telemedicine in retinoblastoma: A 3-tier approach implemented in the first eye salvage program in Jordan. Pediatr Blood Cancer 2008; (submitted).
- Polit DF, Black CT. Nursing Research-Principals and Methods. 7th ed. Lippincott Williams and Wilkins; 2004.
- McKillip J. Need analysis-Tool for the human services and education. Sage Publications Inc.; 1987.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004; 24: 105–12
- Digital Imaging and Communication in Medicine (DICOM). Nema Standard Publication 1999.
- Karlsson M, Björk-Eriksson T, Mattson O, Mattson S, Montelius A, Nilsson P, et al. “Distributed proton radiation therapy”-a new concept for advanced competence support. Acta Oncol 2006; 45: 1094–101