Abstract
Background
In Denmark, fine needle aspiration is the standardized tool for obtaining tissue samples from lymph nodes (LN) of the neck. However, because of a low specificity toward lymphomas, LNs suspicious for this disease are often surgically removed and examined. International studies have implied that a core needle biopsy (CNB) is sufficient for detecting lymphomas, thereby potentially avoiding surgery. However, all studies have been conducted retrospectively and the goal of this prospective study was to find the true sensitivity of CNB.
Material and Methods
Fifty-seven patients were enrolled in the study, one was excluded due to lack of CNB material. LNs suspected for lymphoma were surgically removed from the neck, whereafter a CNB was obtained from the removed LN. The CNB and the remaining part of the LN were sent to the Department of Pathology for further processing and the samples were blinded and examined by two pathologists separately. A consensus diagnosis was reached in cases with divergent diagnostic proposals. Sensitivity of the CNB method in comparison to whole tissue sections for lymphoma diagnosis was calculated.
Results
The CNB method gave the correct diagnosis in 66% of lymphoma cases, was inconclusive in 14% and gave an incorrect lymphoma subtype in 18%. In 2% the CNB wrongly resulted in a benign diagnosis. CNB was correct in all the non-lymphoma cases; thereby retaining a specificity of 100%.
Conclusion
This prospective study found a sensitivity of 66% for diagnosing lymphoma with a CNB. As the CNB in this study was obtained under optimal conditions, unlike in clinical practice, we conclude that CNB cannot be recommended as a standard tool for diagnosing lymphomas.
Background
Lymphoma is in the top ten of the most commonly diagnosed cancers in Denmark. With an incidence of approximately 1400 cases per year, it is responsible for 3.4% of all cancers in Denmark, and the age-standardized incidence rate has been increasing over the last six decades [Citation1]. Lymphomas are traditionally divided into Hodgkin lymphoma, which accounts for approximately 10% of the cases, and non-Hodgkin lymphoma, including the remaining 90% [Citation2]. Standard treatment for Hodgkin lymphoma includes chemo- and radiotherapy and the 5-year survival rate is higher than 85% [Citation1]. Non-Hodgkin lymphomas entail more than 30 different subtypes [Citation2,Citation3]. Various treatment combinations are available and most often include chemo-immunotherapy. Survival rates are very much dependent on the lymphoma subtype, but the overall 5-year survival is approximately 70% [Citation1].
To diagnose lymphoma in patients, a tissue sample is required. In 40% of the cases, a biopsy is obtained from a suitable lymph node (LN) accessible at the patient’s neck, and consequently, 12-15% of all malignancies diagnosed in the head and neck are lymphomas [Citation4]. In Denmark, patients presenting with enlarged LNs are traditionally processed through an accelerated diagnostic process; the cancer pathway [Citation5]. Patients are referred to a diagnostic center for Ear-Nose-Throat (ENT) diseases to obtain the following: Complete medical history, an ENT-examination (including fiber-optic endoscopy and ultrasonic examination of the neck structures), a preliminary tissue sampling from a suspicious LN (using fine-needle aspiration), and supplemental imaging of the neck (CT, MRI, or PET-CT).
Tissue samples from the neck for general diagnostics are usually obtained by a Fine Needle Aspiration (FNA), an effective and safe method to acquire cell samples. The FNA most often enables us to distinguish between lymphomas or squamous cell carcinomas (SCC) and adenocarcinoma metastasis. The FNA-technique has a relatively high specificity and sensitivity for SCC but is less sensitive with other kinds of neoplasias, e.g. breast cancer, where it only detects 75% of the malignancies [Citation6] and only 69% of the thyroid cancers [Citation7]. An alternative modality for obtaining tissue samples is a core needle biopsy (CNB), where sensitivity rates are much higher, with 98% for breast cancers and 87% for thyroid cancers [Citation6,Citation7]. Choosing FNA over CNB avoids the potential risk of local spreading of an unexpected SCC. Furthermore, an assumed low sensitivity for lymphoma subtyping with CNB limits the use of this procedure. However, these traditions might be outdated as the scientific basis for local spreading is controversial [Citation8–11], and lymphomas might not have the same properties for local spreading as SCC does.
In case the FNA demonstrates conclusive pathologic findings, i.e. metastasis from a lung squamous cell carcinoma (SCC), the patient will diverge to that specific cancer pathway. If the results are inconclusive, the pathway is continued until a precise diagnosis can be established. Usually, the FNA is repeated once, after which an alternative modality is selected, either being CNB or surgical extirpation. Nevertheless, this will inevitably prolong the pathway (doctors’ delay). Since FNAs have a low sensitivity for lymphomas, preferable a whole lymph node has to be surgically removed to obtain sufficient tissue for diagnostics and grading, including flow cytometry and molecular analyses [Citation12,Citation13]. This procedure entails hospitalization, general anesthesia, and further discomfort for the patients, as well as the risk for postoperative sequelae and complications like scarring, bleeding, infection, and nerve damage of the head and neck.
Haematological management of lymphomas differs significantly among subtypes; therefore, a precise diagnosis is of major importance. Technological progress has made new molecular methods and immunohistochemical markers available. The amount of the sample required for diagnostics has thus decreased, thereby theoretically enabling full subtyping of lymphomas from CNBs. However, the sensitivity and specificity of CNB in the exact diagnosis of lymphomas remain disputed. Pedersen et al. found a high sensitivity (93.6%) for diagnosing malignant lymphoma in cervical lymph nodes, including full subtyping by transcutaneous in vivo CNB using a G14 needle [Citation14]. A recent German report comparing CNB and surgical excision biopsy (SEB) found that CNB could not establish a definite diagnosis in 8.3% of the cases, compared to 2.8% for SEB [Citation15]. Several retrospective studies examining the efficacy of in vivo CNB for diagnosing lymphoma have been conducted [Citation14–17], but the conclusions are elusive. To our knowledge, no studies which have compared CNB and SEB from the same lymph node exist.
The present study compares the quality of CNB against the current traditional histological examination from SEB. The aim is to determine CNB’s applicability in the diagnostic workup of lymphomas. We hypothesize that a diagnosis and full subtyping of lymphoma can be obtained equally with CNB compared to SEB. If this is correct, the surgical removal of a lymph node can be omitted. As CNB is an outpatient procedure, general anesthesia is not needed and fixation time for the biopsy is shorter compared to a SEB, this would result in a shorter diagnostic pathway in benefit for both the patients and the health care system.
Materials and methods
The study was prospectively conducted. We enrolled 57 patients in the period from 21.05.2015 to 31.03.2017. All patients were suspected of lymphoma on the neck and referred to the Department of Otorhinolaryngology and Maxillofacial Surgery, Zealand University Hospital.
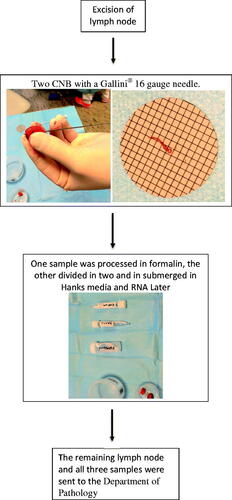
The initial FNAs found evidence of malignancy but were inconclusive; hence the patients were scheduled for surgical extirpation of LN in general anesthesia. Only patients judged by preoperative ultrasound, to have LN larger than 2 cm at the longest possible axis, were included in the study. The surgeons were all experienced in removing neck lymph nodes. During surgery, when the LN was removed, two CNBs were immediately obtained extra corporally with a Gallini® 16 gauge needle. The samples were obtained from the longest possible axis of the node, ensuring a sufficient tissue volume. One sample was preserved in formalin, while the other was divided in two – one for preservation in Hanks’ media for flow cytometric examination, and the other in RNA-Later for molecular analysis (). The remaining tissue of the lymph node (SEB-res) was preserved fresh and sent with the two CNBs to the Department of Pathology. The SEB-res specimen was fixed in formalin and processed grossed the next day, following standard laboratory protocols. The CNB was fixed in formalin. For both specimens, routine hematoxylin and Giemsa stains were prepared as well as flow cytometric analyses. The samples were blinded according to CNB or SEB-res for both pathologists. A consensus diagnosis was found in the collaboration between the two pathologists in the case of divergent diagnosis.
Ethics
Since we followed the standard protocol for lymphoma examination with the extirpation of an enlarged lymph node, after the extirpation examined the node with CNB, there was no delay in the patients’ diagnostics and no risk of side effects from CNB. In the case of insufficient tissue for both CNBs (<2 cm in the longest axis), the lymph node was not included in the study, and the lymph node was examined as usual.
We acquired oral and written informed consent from all participants. The Danish National Committee on Health Research Ethics and the Danish Data Protection Agency (VEK no. SJ-440) approved the protocol for the clinical trial.
Statistical analysis
We performed a power calculation to calculate the required sample size. Based on the hypothesis that there is a significant difference (p < .05) between the exact lymphoma diagnoses between CNB and SEB specimens with a power of 80% where SEB was considered the gold standard procedure (level 1) and CNB is inferior (level 0.9), a total of 56 patients were needed. The null hypothesis would be refuted if the agreement between the two methods would be less than 90%.
The sensitivity and specificity of the CNB compared to the gold standard for diagnosing lymphoma were calculated using descriptive statistics using Microsoft Excel® software.
Results
A total of 57 lymph nodes (from 57 patients) were removed. One was excluded because of insufficient material for the CNB analysis. The remaining 56 lymph nodes were examined using both modalities (). The patients had a mean age of 62 years (range 20–88, median 68). There were 34 males and 22 females, ratio 1.5:1.
Table 1. Overview of histological diagnosis, flow cytometry results and molecular analysis from surgical excision biopsy (SEB-res) and core needle biopsy (CNB) in 56 patients suspected for malignant lymphoma.
The final histopathological diagnoses encompassed 44 cases of lymphoma, six nonmalignant hyperplasias, four sarcoidosis, and two non-lymphoma malignancies of which one was a metastasis from a seminoma and one was a myeloid sarcoma (). In 41 cases (73%), the CNB and SEB-res diagnoses were in agreement (). There was full agreement in cases with reactive histology, sarcoidosis, T-cell lymphomas, and non-lymphoma malignancies. In cases with classical Hodgkin lymphoma, only two of six cases were conclusive or suggestive of the final diagnosis. In the B-cell lymphoma group, 25 of the 36 cases resulted in the same diagnoses (69%), and 11 cases diverged (). In four cases, the CNB was inconclusive or gave a false diagnosis. In one case, the CNB revealed changes suspicious for B-cell lymphoma, but were not conclusive.
Table 2. Overview of histological diagnosis from core needle biopsies (CNB) of neck lymph nodes in 56 patients suspected for malignant lymphomas.
In one sample, the CNB revealed CLL and transformation to DLBCL, and the first diagnosis of the SEB was CLL and transformation to cHL. However, the consensus diagnosis was CLL and transformation to DLBCL also in the SEB. This reflects the challenges in subtype lymphoma diagnostics.
In summary, the CNB was correct in 29 (66%) of the 44 cases of lymphoma ().
Table 3. Overview of incorrect histological diagnosis in CNB with a final lymphoma diagnosis (n = 44).
Flow cytometry results were overall in excellent agreement with the two methods. However, in three cases, no leucocytes were present, possible due to sampling artifacts. Molecular studies, including FISH analyses and clonality analyses of the T-cell receptor or the immunoglobulin gene rearrangement, were mostly performed on SEB specimens ().
Discussion
To our knowledge, this is the first prospective study examining the efficacy of CNB compared to SEB in patients with enlarged lymph nodes of the head and neck, suspicious of lymphoma. In Denmark, the “gold standard” in lymphoma diagnostic workup is SEB. Internationally though, there has been an increasing interest in the use of CNB for diagnosing and subtyping lymphoma. Studies that have tried to determine the advantages and pitfalls of CNB have all been retrospective, and the studies have not correlated CNB from whole LN’s in the same patient as in our prospective and blinded study. Furthermore, in our setup, the conditions for performing CNB were optimal since the LN was removed from the patient before the CNB procedure. With this setup, we can predict the true sensitivity of the CNB within this selected population.
We found a sensitivity for lymphoma, including subtyping by CNB of 66%, which is in line with some prior retrospective studies [Citation17], whereas others have found a higher sensitivity of around 90-95% [Citation14,Citation16]. The specificity of CNB was 100% for detecting benign lesions, as no false-positive malignancies were detected.
In the 15 cases where the CNB resulted in an incorrect diagnosis, eight of the misdiagnoses were of no major clinical impact on the diagnostic situation of the patients, as they would have led to a re-CNB or SEB (inconclusive and possible lymphoma). The diagnostic workup would have been prolonged, but these cases did not represent highly aggressive lymphomas that required immediate therapeutic action.
Six incidents were semi-severe, as the CNB revealed an up- or down-graded diagnosis compared to the final diagnoses (up- and down-classification), this would be a problem with regards to therapeutic decision making. An example is case 25 in , the CNB revealed HL and the final diagnosis was GZL. The patient would have received less aggressive therapy than what would be optimal as a result of the CNB’s down-graded diagnoses. Another example is case 26 in , the CNB revealed DLBCL and the final diagnosis was FL grade 3A. The patient, in this case, would have received more aggressive therapy as a result of the CNB’s up-graded diagnoses, exposing the patient to unnecessary side effects. Both situations would prevent the patients from receiving optimal treatment.
Finally, in one case the CNB revealed no sign of malignancy as opposed to the final diagnosis of DLBCL, a highly aggressive form of Non-Hodgkin lymphoma that requires speedy and correct therapeutic interventions. In this scenario, a repeat CNB or SEB would probably be performed at a later stage, since the patients presented with symptoms highly suspicious of malignant disease and in this case, the prolonged diagnostic workup would lead to increased morbidity and possible mortality. Interestingly, there was one case where the CNB was correct while the SEB was mistaken. This was concluded after the two pathologists compared the two samples and added the result of the flow cytometry.
The CNB was correct in 33% (2/6) of cases of Hodgkin Lymphoma (HL) (three “inconclusive” and one attentive diagnosis). This is a well-known and typical situation with HL due to the paucity of malignant cells in HL, often encompassing only a few percent of the lymphoma tissue. HL can partially involve the LN and differential diagnosis against certain T-cell lymphomas, e.g. angioimmunoblastic T-cell lymphoma and T-cell, nodular lymphocyte predominant Hodgkin lynphoma and histiocyte rich B-cell lymphoma is notoriously difficult in small tissue samples [Citation18,Citation19]. In addition, EBV positive lymphoproliferations and infectious monoculeosis can pose significantly differential diagnostic challenges.
We had a total of nine patients with follicular lymphoma (FL). The CNB revealed the correct lymphoma grade in two and different grades in five. There would not be a clinically relevant consequence in three of these, as the treatment of grades 1–3A principally is the same for stage III-IV, in both asymptomatic and symptomatic patients. In the last two cases, the difference in diagnosis (FL 3 vs. FL 3B) would result in the patient possibly not receiving the optimal therapy, as FL grade 3B is treated as a DLBCL. In situations dealing with FL grades 1–3A, one could argue that treatment of FL follows the same guidelines and this would suffice in daily clinical practice, however, FL can be heterogeneous and grade 3B or transformation to DLBCL can be found elsewhere in the remaining LN [Citation20]. To this end, in clinical practice, a suspicion of high-grade lymphoma or transformation by PET-CT evaluation would result in the removal of a whole LN or a re-biopsy. We have included the three cases of different grades (grades 1 to 3 A) as correct. If these cases were to be defined as the diverging diagnosis, it would result in a sensitivity of CNB for diagnosing lymphoma of 59% (26/44 cases). In addition, suspicion of transformation to a large cell lymphoma from a low-grade lymphoma can be suspected from PET-CT imaging and clinical presentation. Partial involvement of a transformed lymphoma can be seen and a CNB might not be the correct approach in this scenario.
We found a CNB sensitivity of 73% for diagnosing all causes of cervical lymph node hyperplasia. This is considerably lower than others have reported [Citation14,Citation16]. These studies were retrospective, did not compare CNB to SEB and had a much lower percentage of lymphoma patients compared to ours (44/56). All are biases that could skew the sensitivity toward a higher percentage.
This is a prospective study, where the obtainment of the CNB was performed as a “best-case scenario,” as the examiner could see that the sample was correctly obtained. This is not realistic to achieve in a routine clinical setting, where, even with the use of ultrasound guidance, the risk of sample error is present. Furthermore, SEB compared to CNB’s, ensures more histological material, which can be used for additional molecular investigations or saved in, e.g. biobanks for research use.
Strengths and limitations
The study was prospective and CNB’s were taken from the same LN’s as the SEB. The two pathologists were blinded to each other’s results and only compared if the diagnosis was not in agreement. The results concerning diagnosis were regardless of the specialist experience, and both the pathologists were trained haematopathologists. It is, however possible, that a pathologist solely focusing on lymphoma diagnostics in CNB, as is the case in diagnostic centers in some countries, could achieve a higher sensitivity.
From each LN we obtained two CNB’s, one was used for histopathological diagnosis. The second biopsy was divided for flow cytometric analysis and molecular analyses. The latter was in most cases not performed, as all molecular studies were conducted on the SEB material. It is possible that more CNB material and material from different enlarged lymph nodes would increase the diagnostic accuracy of CNB samples.
Conclusion
The sensitivity is 66% for diagnosing lymphoma with a CNB in a prospective partially blinded setting, comparing the diagnosis with a SEB from the same lymph node. The specificity of benign disease was found to be 100%. The sensitivity in non-lymphoma cases of CNB was 100%.
The use of CNB for diagnosing lymphoma did not reach sufficient sensitivity and specificity for diagnosing lymphoma and specific lymphoma subtypes. We recommend that the use of core needle biopsies is restricted to patients with high comorbidities not eligible for general anesthesia or when no peripheral LN’s are available, e.g. in cases with retroperitoneal location. To this end, the best setup for diagnosing, sub-classification and grading of lymphomas are done by excision of whole LN’s, resulting in the best precondition for therapeutic decision making for the individual patient.
Supplemental Material
Download MS Word (33.4 KB)Acknowledgements
The authors thank the operating theatre nurses and colleagues at the Department of Otorhinolaryngology and Maxillofacial Surgery, Zealand University Hospital, Denmark. Likewise The authors thank the laboratory technicians at the Pathology Department, Zealand University Hospital, Denmark for kind assistance. A special thanks to doctors Ramon G. Jensen, Magnus Balslev Avnstorp and Nicolaj Duus for assistance with the sampling.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- NORDCAN [Internet]. Cancer statistics for the nordic countries. Available from: http://www-dep.iarc.fr/NORDCAN/DK/frame.asp
- Danish Lymphoma Group [Internet]. Danish Lymphoma Group’s annual report, Malignant Lymphoma and CLL, annual report 2017. Available from: http://www.lymphoma.dk/wp-content/uploads/2019/05/4689_lyfocll-rsrapport-2017-endeligversion.pdf
- Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–2390.
- Cooper JS, Porter K, Mallin K, et al. National Cancer Database report on cancer of the head and neck: 10‐Year update. Head Neck. 2009;31(6):748–758.
- Sundhedsstyrelsen [Internet]. Danish health authority, cancer pathways. Available from: https://www.sst.dk/da/viden/kraeft/kraeftpakker
- Hukkinen K, Kivisaari L, Heikkila PS, et al. Unsuccessful preoperative biopsies, fine needle aspiration cytology or core needle biopsy, lead to increased costs in the diagnostic workup in breast cancer. Acta Oncol. 2008;47(6):1037–1045.
- Sung JY, Na DG, Kim KS, et al. Diagnostic accuracy of fine-needle aspiration versus core-needle biopsy for the diagnosis of thyroid malignancy in a clinical cohort. Eur Radiol. 2012;22(7):1564–1572.
- Diaz LK, Wiley EL, Venta LA. Are malignant cells displaced by large-gauge needle core biopsy of the breast? AJR Am J Roentgenol. 1999;173(5):1303–1313.
- Liebens F, Carly B, Cusumano P, et al. Breast cancer seeding associated with core needle biopsies: a systematic review. Maturitas. 2009;62(2):113–123.
- Ngamruengphong S, Swanson KM, Shah ND, et al. Preoperative endoscopic ultrasound-guided fine needle aspiration does not impair survival of patients with resected pancreatic cancer. Gut. 2015;64(7):1105–1110.
- Minaga K, Takenaka M, Katanuma A, et al. Needle Tract Seeding: an overlooked rare complication of endoscopic ultrasound-guided fine-needle aspiration. Oncology. 2017;93(1):107–112.
- The Danish Head and Neck Cancer Study Group [Internet]. DAHANCA guidelines. Available from: https://www.dahanca.dk/CA_Adm_Web_Page?WebPageMenu=1&CA_Web_TabNummer=0
- Danish Lymphoma Group [Internet]. Guidelines for diagnostics and treatment of lymphoma and CLL. Available from: http://www.lymphoma.dk/retningslinjer
- Pedersen OM, Aarstad HJ, Lokeland T, et al. Diagnostic yield of biopsies of cervical lymph nodes using a large (14-gauge) core biopsy needle. APMIS. 2013;121(12):1119–1130.
- Johl A, Lengfelder E, Hiddemann W, et al.; The German Low-grade Lymphoma Study Group (GLSG). Core needle biopsies and surgical excision biopsies in the diagnosis of lymphoma-experience at the Lymph Node Registry Kiel. Ann Hematol. 2016;95(8):1281–1286.
- Allin D, David S, Jacob A, et al. Use of core biopsy in diagnosing cervical lymphadenopathy: a viable alternative to surgical excisional biopsy of lymph nodes? Ann R Coll Surg Engl. 2017;99(3):242–244.
- Kwon M, Yim C, Baek HJ, et al. Ultrasonography-guided core needle biopsy of cervical lymph nodes for diagnosing head and neck lymphoma compared with open surgical biopsy: Exploration for factors that shape diagnostic yield. Am J Otolaryngol. 2018;39(6):679–684.
- Harris NL. Hodgkin's disease: classification and differential diagnosis. Mod Pathol. 1999;12(2):159–175.
- Fend F. Classical Hodgkin lymphoma and its differential diagnoses. Diagn Histopathol. 2015;21(10):400–407.
- Horn H, Schmelter C, Leich E, et al. Follicular lymphoma grade 3B is a distinct neoplasm according to cytogenetic and immunohistochemical profiles. Haematologica. 2011;96(9):1327–1334.