Abstract
Objective: To assess postsurgical clinical and economic outcomes of patients who received local infiltration containing liposomal bupivacaine versus traditional bupivacaine for pain management following total hip arthroplasty (THA).
Methods: This retrospective study included two groups of consecutive patients undergoing THA. The experimental group received local infiltration with a combination of liposomal bupivacaine, bupivacaine HCl 0.25% with epinephrine 1:200,000, and ketorolac for postsurgical analgesia. The historical control group received the previous standard of care: local infiltration with a combination of bupivacaine HCl 0.25% with epinephrine 1:200,000 and ketorolac. Key outcomes included distance walked, length of stay (LOS), opioid medication use, numeric pain scores, hospital charges, hospital costs, all-cause 30 day readmission rate, and adverse events (AEs). Both unadjusted and adjusted (i.e. age, sex, insurance type, living situation, body mass index, procedure side, and comorbidity) outcomes were compared between the two groups.
Results: The experimental group (n = 64) demonstrated statistically significant improvement versus the historical control group (n = 66) in mean distance walked on discharge day (249.2 vs. 180.0 feet; unadjusted p = .025, adjusted p = .070), mean LOS (2.0 vs. 2.7 days; p < .001, p = .002), proportion of patients who used opioid rescue medication on postoperative day (POD) 1 (29.7% vs. 56.1%; p = .002, p = .003) and POD 2 (7.8% vs. 30.3%; p = .001, p = .003), mean cumulative area under the curve for pain score on POD 0 (127.6 vs. 292.5; p < .001, both), POD 1 (92.9 vs. 185.0; p < .001, both), and POD 2 (93.8 vs. 213.8; p = .006, both). Among a subgroup of patients with available financial information, mean hospital charges were lower in the experimental group ($43,794 [n = 24] vs. $48,010 [n = 66]; p < .001, both). Rates of all-cause 30 day readmission and AEs were not significantly different between groups. No falls occurred.
Conclusions: Infiltration at the surgical site with liposomal bupivacaine was associated with improved postsurgical outcomes when compared with traditional bupivacaine in patients undergoing THA.
Introduction
Total hip arthroplasty (THA) is one of the most common orthopedic surgical procedures in the United States. The most recent data from the Centers for Disease Control and Prevention indicate that, in 2010 alone, more than 332,000 patients underwent THACitation1. The prevalence of hip osteoarthritis and associated risk factors such as obesity and advancing age are expected to increase, resulting in greater numbers of patients who will need to undergo THACitation2. By 2030, the annual US demand for primary hip arthroplasty is expected to increase to 572,000 proceduresCitation3.
As the number of THA procedures increases in the coming decades, it is likely that the burden of inadequate postsurgical pain management associated with these procedures will also escalate. Even though postsurgical pain and its clinical consequences are recognized as important problems in orthopedic surgeryCitation4–6, there is currently no gold standard for effective management of postsurgical pain after THACitation7. In the short term, inadequate treatment of acute postsurgical pain may directly or indirectly contribute to higher healthcare costs by delaying mobilization, prolonging hospital length of stay (LOS), and necessitating readmissionCitation5,Citation8–10. In the long term, inadequately controlled postsurgical pain may reduce the patient’s quality of life and increase the risk of developing chronic painCitation8. Furthermore, quality of pain management is now tied to hospital reimbursementCitation11 through the Hospital Inpatient Value-Based Purchasing (VBP) program. The VBP program is a quality improvement initiative by the Centers for Medicare & Medicaid Services (CMS)Citation12 mandating that amounts of value-based incentive payments to hospitals be determined by the total performance score achieved by the hospital on a set of quality indicatorsCitation12. One of the key quality indicators in the program is based on the Hospital Consumer Assessment of Healthcare Providers and Systems survey, which is an assessment of patients’ perceptions regarding several components of their hospital stay, including pain managementCitation12,Citation13.
Clinicians should consider the use of opioid-sparing multimodal analgesic regimens for postsurgical pain management whenever possible in order to optimize analgesia while minimizing risk of opioid-related adverse eventsCitation8. Surgical site infiltration with a local anesthetic provides safe postsurgical analgesia in THACitation5,Citation14,Citation15, with efficacy similar to peripheral nerve blockCitation16. However, the utility of traditional local anesthetic formulations has been limited by their short duration of actionCitation15,Citation17.
Liposomal bupivacaine (bupivacaine liposome injectable suspension; Exparel1) is a prolonged-release formulation of bupivacaine indicated for single-dose administration into the surgical site to produce postsurgical analgesiaCitation18. Clinical studies of liposomal bupivacaine conducted across a variety of surgical models have demonstrated its effectiveness in providing up to 72 hours of postsurgical analgesiaCitation19,Citation20 with a safety profile similar to bupivacaine HClCitation21. The use of liposomal bupivacaine may also obviate the need for elastomeric pumps, knee immobilizers, and patient-controlled analgesia (PCA), thus reducing hospital costs incurred for supplies, equipment, and possibly, for professional servicesCitation22.
In this study, we compared postsurgical outcomes following THA, including distance walked, LOS, opioid consumption, pain intensity, hospital charges, hospital costs, all-cause 30 day readmission rates, and adverse events (AEs) in patients who received local infiltration with liposomal bupivacaine versus traditional bupivacaine, the previous standard of care for postsurgical pain management at our institution.
Patients and methods
Study design
This was a retrospective study of patients who underwent THA at Unity Point–Proctor Hospital in Peoria, IL, USA, from June 2011 through July 2015. Two treatment groups were studied. The historical control group consisted of consecutive patients who underwent THA from June 2011 through July 2013, and received local infiltration at the surgical site with a combination of bupivacaine HCl 0.25% with epinephrine 1:200,000 and ketorolac, the institutional standard of care at the time. The experimental group consisted of consecutive patients who underwent THA from August 2013 through July 2015, and received local infiltration at the surgical site with a combination of liposomal bupivacaine, bupivacaine HCl 0.25% with epinephrine 1:200,000, and ketorolac for postsurgical pain relief.
Ethics
The study protocol was approved by the Peoria Institutional Review Board at the University of Illinois College of Medicine at Peoria in Peoria, IL. A total of three reviewers extracted patient data in a manner that was compliant with the Health Insurance Portability and Accountability Act. To further protect patient confidentiality, the data, which included information on demographics, health status, and clinical outcomes, was de-identified prior to analysis and thereafter accessible only to researchers and clinicians involved in the study.
Inclusive criteria
All patients who underwent primary THA at Unity Point–Proctor Hospital in Peoria, IL during the study period were eligible for inclusion in the study.
Treatments
The senior author (B.T.M.) performed all surgeries using a standard cementless, posterolateral approach for THA. One hour before surgery, all patients received celecoxib 200 mg (one tablet), dextromethorphan polistirex 10 mL (one dose), and acetaminophen 325 mg/hydrocodone 10 mg (two tablets). Spinal anesthesia was used. If spinal anesthesia was unsuccessful or the patient had a previous spinal fusion or refused spinal anesthesia, general anesthesia was used. In the historical control group, the soft tissues within the surgical field were infiltrated with a combination of bupivacaine HCl 0.25% with epinephrine 1:200,000 (30 mL) and ketorolac (30 mg, 15 mg, or 0 mg based on allergies, age, renal function status, and previous patient tolerance). In the experimental group, the soft tissues surrounding the hip were infiltrated with a combination of liposomal bupivacaine (266 mg/20 mL), ketorolac (30 mg, 15 mg, or 0 mg depending on age and renal function status), and bupivacaine HCl 0.25% (30 mL) with epinephrine 1:200,000. One milliliter was injected in the anterior capsule in three sites from distal to proximal. Approximately 5 mL was injected into the gluteus medius and minimus above the greater trochanter. The remainder was injected into the iliotibial band and subcutaneous tissue. It should be noted that admixing liposomal bupivacaine with a nonsteroidal anti-inflammatory drug (NSAID; e.g. ketorolac) is an off-label use of liposomal bupivacaineCitation18. However, an initial compatibility assessment did not identify any substantial safety concerns when admixing liposomal bupivacaine with ketorolacCitation23. Patients in both groups were prescribed intravenous (IV) ketorolac 15–30 mg every 6 hours (if <70 years of age and without renal insufficiency) and acetaminophen 325 mg/hydrocodone 10 mg (1–2 tablets every 4–6 hours); IV fentanyl 50 mcg every 1 hour was available via PCA as needed for breakthrough pain. Deep vein thrombosis prophylaxis consisting of compression stockings and foot pumps was provided to all patients during their hospital stay. Rivaroxaban 10 mg daily was prescribed for a total of 30 days in patients who had not been receiving anticoagulants preoperatively; warfarin or dabigatran etexilate were continued in patients who had used them preoperatively. All patients underwent physical therapy as soon as possible after surgery (including gait training with a walker) with a goal of initiation of physical therapy on the afternoon of the day of surgery. Physical therapy continued while the patient was transitioned to oral opioids, and was continued in the outpatient setting or a skilled nursing environment until the patient met criteria for the level of independence required by the treating physical therapist. Progress in physical therapy was also monitored by the senior author (B.T.M.). Patients were called within 2 days after surgery for follow-up, and were seen in the office at 2 weeks, 6 weeks, and 3 months after surgery; additional follow-up visits were scheduled as necessary.
Baseline data included demographics, insurance type, living situation (i.e. family support or alone), medical history, primary diagnosis, current treatments, comorbidities, alcohol use, smoking, and body mass index. At discharge, assessments included distance walked, frequency of physical therapy, LOS, total daily dose of opioid medication use, pain intensity, falls, and other AEs.
Financial information was available for a subgroup of study patients, including hospital charges incurred during the hospitalization in the following six categories: 1) room and board, 2) pharmacy, 3) medical/surgical supplies, 4) diagnostic/laboratory tests/operating room (OR), 5) physical therapy (PT)/occupational therapy (OT)/speech therapy (ST), and 6) other. Values were adjusted to 2015 US dollars using the Hospital Service Consumer Price IndexCitation24. Hospital total charges were converted to total costs using the estimated cost-to-charge ratio (CCR) for the hospital where this study was conducted (provider number 140209), which was publicly available from the CMSCitation25. In order to remove the effect of CCR variations during the study period, CCR was set to 0.228, which is an average of the available 2010–2013 values.
Efficacy measures
Ambulation and LOS were the primary outcome measures. Ambulation was assessed during physical therapy evaluations at least once daily, including total distance walked on a given day (measured in feet) and degree of assistance required (level of assistance, number of people providing assistance, and use of assistive devices). Documentation of postsurgical opioid medication use included the name and daily dose of the opioid medication taken per day of hospitalization. Other secondary outcome measures included pain intensity, hospital charges, hospital costs, all-cause 30 day readmission rate, and AEs. Pain intensity was assessed using an 11 point numeric rating scale (NRS; 0 = no pain, 10 = worst possible pain) and was recorded at baseline, at the end of spinal anesthesia, and at first administration of opioid pain medication after end of surgery; pain intensity during activity was also recorded during physical therapy.
Statistical analysis
Based on results from a previous studyCitation26, a power analysis determined that a sample size of 110 patients (55 per treatment group) was required to achieve 80% power to detect a between-group difference in the primary outcome measures (distance walked 193.0 ± 202.9 feet [adductor canal infiltration with bupivacaine HCl and knee infiltration with liposomal bupivacaine] vs. 210.8 ± 143.7 feet [adductor canal infiltration and knee infiltration with liposomal bupivacaine] and 46.3 ± 72.6 feet [continuous femoral nerve block with ropivacaine HCl]; LOS 3.0 ± 1.7 days vs. 2.2 ± 1.2 days and 3.2 ± 0.7 days, respectively]) at a significance level of 0.05. All statistical tests were performed against a two-sided alternative hypothesis with a significance level of 5% (α = .05). For efficacy outcomes, hospital charges, hospital costs, p values adjusted by age, sex, insurance type, living situation, body mass index, procedure side, and comorbidity were also determined. Descriptive statistics, including mean and standard deviation (SD) were calculated for continuous variables; frequencies or percentages were calculated for nominal variables. In the univariate analysis for demographics and comorbidities, a Student’s t test was used to compare age and body mass index between groups, and chi-square test was employed for other nominal variables.
Regarding the primary outcome measures, analysis of variance (ANOVA) on log-transformed data (if skewed distribution) was used for between-group comparisons of distance walked and LOS. With regard to the secondary outcome measures, opioid consumption was assessed using a log-rank test when comparing time to first opioid use between groups, while ANOVA on log-transformed data was used to compare mean opioid consumption (converted to oral morphine equivalents) through 72 hours after surgery between groups. ANOVA was used to compare the cumulative pain scores (area under the curve [AUC] from 0 to 12 hours and from 12 to 24 hours) based on daily mean NRS scores in both groups. Multivariable regression analysis using the generalized linear model with log link and gamma distribution was used to compare hospital charges and hospital costs. A logistic regression model was used to estimate the odds ratio of all-cause 30 day readmission in both groups. The multivariable regression models controlled for age, sex, insurance type, living situation, body mass index, procedure side, and comorbidity for all outcomes. Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) or later.
Results
Patients
A total of 130 patients were included, 64 in the liposomal bupivacaine experimental group and 66 in the traditional bupivacaine control group. The groups were well matched, with no significant between-group differences in demographics (). Medical comorbidities present at the time of surgery are summarized in . The control group had a significantly lower proportion of patients with thyroid disease (p = .033) and higher proportion with hypercholesterolemia compared with the liposomal bupivacaine group (p = .047).
Table 1. Patient demographics.
Table 2. Comorbidities.
Efficacy
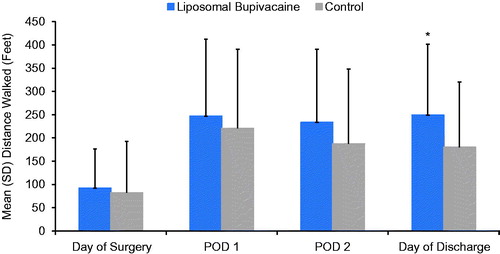
The mean (SD) distance walked on the day of discharge was significantly greater in the liposomal bupivacaine group (249.2 [151.9] feet) compared with the control group (180.0 [140.5] feet; unadjusted p = .025, adjusted p = .070) []). There was no significant difference in the mean distances walked on the day of surgery, postoperative day (POD) 1, or POD 2.
Figure 1. Mean distance walked after surgery. *Unadjusted p = .025, adjusted p = .070. Day of surgery: liposomal bupivacaine, n = 62; control, n = 66. POD 1: liposomal bupivacaine, n = 55; control, n = 56. POD 2: liposomal bupivacaine, n = 32; control, n = 32. Day of discharge: liposomal bupivacaine, n = 54; control, n = 41. POD: postoperative day; SD: standard deviation.
The mean (SD) LOS was shorter in the liposomal bupivacaine group compared with the control group (2.0 [1.2] versus 2.7 [1.2] days; unadjusted p < .001, adjusted p = .002). The proportion of patients discharged on the day of surgery and on POD 1 was significantly greater in the liposomal bupivacaine group compared with the control group (day of surgery: 5% versus 0%, unadjusted and adjusted p < .001; POD 1: 39% vs. 9%, unadjusted and adjusted p < .01). In addition, 72% (46/64) of patients in the liposomal bupivacaine group were discharged directly to their home compared with 61% (40/66) of controls (unadjusted p = .175, adjusted p = .357).
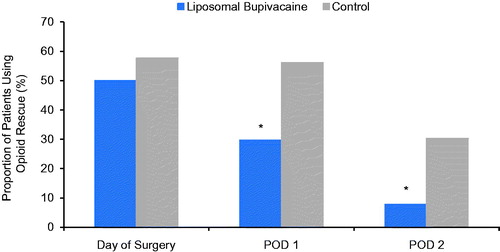
The proportion of patients who used rescue opioids is summarized in . Significantly fewer patients in the liposomal bupivacaine group required opioid rescue on POD 1 (29.7% vs. 56.1%; unadjusted p = .002, adjusted p = .003) and POD 2 (7.8% vs. 30.3%; unadjusted p = .001, adjusted p = .003) compared with the control group. The proportion of patients in the liposomal bupivacaine group who were opioid free after surgery increased from 50.0% on the day of surgery to 70.3% on POD 1 and 92.2% on POD 2.
Figure 2. Proportion of patients using opioid rescue. *Unadjusted and adjusted p < .01. Day of surgery: liposomal bupivacaine, n = 32; control, n = 38. POD 1: liposomal bupivacaine, n = 19; control, n = 37. POD 2: liposomal bupivacaine, n = 5; control, n = 20. POD: postoperative day.
When accounting for patients who did not use any opioids on a given day (i.e. amount used was 0 mg), the mean (SD) amount of daily opioids used was higher (but not statistically significantly so) in the liposomal bupivacaine group on the day of surgery (22.2 mg [75.3 mg] vs. 16.8 mg [42.3 mg], p = .813) but lower on POD 1 (9.6 mg [20.5 mg] versus 14.5 mg [29.4 mg], p = .008) and POD 2 (2.0 mg [9.2 mg] vs. 7.5 mg [27.0 mg], p < .001).
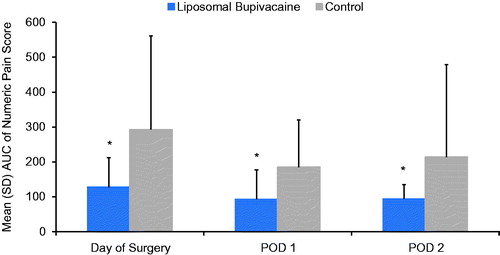
The mean (SD) cumulative AUC for pain score was significantly lower in the liposomal bupivacaine group versus the control group on the day of surgery (127.6 vs. 292.5; unadjusted and adjusted p < .001), POD 1 (92.9 vs. 185.0; unadjusted and adjusted p < .001), and POD 2 (93.8 vs. 213.8; unadjusted and adjusted p = .006; ). The mean (SD) pain scores in the liposomal bupivacaine and control groups on the day of surgery were 2.9 (1.5) versus 3.6 (2.1), respectively (unadjusted p = .030, adjusted p = .055), 2.9 (1.4) versus 3.7 (1.8) on POD 1 (unadjusted p = .008, adjusted p = .009), and 3.2 (1.2) versus 3.8 (1.7) on POD 2 (unadjusted p = .074, adjusted p = .032).
Figure 3. Mean cumulative AUC of the numeric pain score. *Unadjusted and adjusted p < .01. Day of surgery: liposomal bupivacaine, n = 62; control, n = 55. POD 1: liposomal bupivacaine, n = 61; control, n = 62. POD 2: liposomal bupivacaine, n = 35; control, n = 51. AUC: area under the curve; POD: postoperative day; SD: standard deviation.
Hospital charges
Hospital charges for the subset of patients with available financial information are summarized in ; the adjusted mean hospital charges were significantly lower in the liposomal bupivacaine group ($43,794 [n = 24]) versus the control group ($48,010 [n = 66]; unadjusted and adjusted p < .001). Charges for room and board, medical and surgical supplies, diagnostic/laboratory testing/ORs, and PT/OT/ST were also significantly lower in the liposomal bupivacaine group compared with the control group (unadjusted and adjusted p < .01 for all comparisons); pharmacy charges were similar between the two groups (unadjusted p = .59, adjusted p = .76). Based on the CMS CCR of 0.228 at this institution, the estimated costs of the THA hospitalization were $965 lower per patient in the liposomal bupivacaine group ($9984 versus $10,949). Although using a hospital’s global CCR to estimate the costs of a specific surgical procedure is challenging, the difference noted between the study groups may nevertheless be directionally accurate.
Table 3. Adjusted hospital charges and cost.
Adverse events and readmission
Six patients (9%) in the liposomal bupivacaine group experienced postsurgical AEs compared with three patients (5%) in the control group (p = .460). No falls were reported in either group. Three patients (5%) in the control group were readmitted within 30 days after discharge versus none in the liposomal bupivacaine group (unadjusted p = .254, adjusted p = .982).
Discussion
In this retrospective study of patients undergoing THA, those who received a liposomal-bupivacaine-based multidrug injection for the management of postsurgical pain were able to walk for a longer mean distance on the day of hospital discharge, had a shorter mean LOS, were less likely to require rescue opioids after surgery, and had lower mean cumulative pain scores than a control group of patients who received the historical standard of care at our hospital. On average, total hospital charges were also lower in the liposomal bupivacaine group.
Other studies describing the use of liposomal bupivacaine in THA have been recently reportedCitation4,Citation22,Citation27–31. Overall, the findings from these studies are consistent with our observations in the current study. For example, a recently published retrospective study of THA patientsCitation31 demonstrated that the use of liposomal bupivacaine was associated with effective postsurgical pain relief, expedited achievement of physical therapy milestones needed for discharge, shorter LOS, and improved discharge disposition versus a historical standard of care regimen for postsurgical pain management that was used for comparisonCitation31. Furthermore, the investigators reported that improvements in quality metrics in patients receiving liposomal bupivacaine were accomplished without PCA and with lower opioid consumption, and postulated that the reduction in opioid use may have contributed to improvements in some performance metrics such as LOS, physical therapy performance, and discharge locationCitation31.
From a financial perspective, discharge destination following total joint arthroplasty is an important consideration, as discharge to inpatient facilities has been reported to cost about $7000 more than discharge to home with health servicesCitation32. Also, discharge to inpatient facilities is associated with a higher risk of 30 day readmission, which can incur an average additional cost of about $22,000Citation32,Citation33. A retrospective study of patients who underwent total joint arthroplasty (including THA) at a single institution showed that postdischarge payments accounted for 36% of the total cost of careCitation34. The financial burden of postdischarge services could potentially be exacerbated by the Comprehensive Care for Joint Replacement model, a CMS initiative that holds acute care hospitals financially responsible for costs of care incurred within 90 days of hospital discharge after total joint arthroplastyCitation35. Readmission during the 90 day postdischarge period was recently examined in a retrospective health insurance claims database of patients who underwent THA or total knee arthroplasty (N = 526,481) and was most prevalent among patients discharged to skilled nursing facilities (range, 22% to 34%) compared with patients discharged home under self-care (12% to 19%) or with home health services (10% to 20%)Citation33. In the present study, the liposomal bupivacaine and control groups had similar rates of discharge home (71.9% versus 60.6%, respectively; unadjusted p = .175, adjusted p = .357) and similar 30 day readmission rates (0% versus 4.5%, respectively; unadjusted p = .254, adjusted p = .982). The study may not have had sufficient power to detect a between-group difference in these outcomes.
For some of the outcomes in our study – e.g. distance ambulated during the immediate postsurgical period, percentage of patients that used rescue opioid medications, and cumulative pain scores – it was not possible to compare our data with those of other investigators due to the dearth of published studies that have assessed similar outcomes in THA patients who received liposomal bupivacaine. However, the mean LOS for the liposomal bupivacaine group in our study (2.0 days) is within the range reported in other published studies (1.9 days–3.1 days)Citation4,Citation22,Citation27,Citation28,Citation30,Citation31.
In our study, the mean distance walked was significantly greater in the liposomal bupivacaine group compared with the control group on the day of discharge (which, on average, was POD 2 in the liposomal bupivacaine group). However, there was no significant difference between groups on POD 2. This finding may be explained by the fact that the day of discharge was POD 2 for only 13 of the 64 patients (20.3%) in the liposomal bupivacaine group. Furthermore, on POD 2, the mean distance walked in the liposomal bupivacaine group was calculated from 32 patients, 11 of whom were discharged that day and 21 of whom were discharged on POD 3 or later.
Reasons for the lack of a significant between-group difference in 30 day readmission rates in our study are unclear. Similar findings have been reported in previous studies. In a retrospective study reported by Domb and colleaguesCitation27, no readmissions were observed in either treatment group in a population of 57 hip surgery patients who received a mixture containing liposomal bupivacaine plus bupivacaine HCl 0.25%/epinephrine or bupivacaine HCl 0.25%/epinephrine alone. Yu and colleaguesCitation31 reported readmission rates of 2.4% in patients who received liposomal bupivacaine (n = 586) versus 1.7% in patients who were treated according to the same pain management protocol but without liposomal bupivacaine (n = 686; p = .422). The 30 day readmission rate observed in the control group in our study was comparable to what has been previously reported in larger-scale studiesCitation36,Citation37. Schairer and colleaguesCitation36 used a large administrative claims database to identify 1415 consecutive patients undergoing primary and revision THA between 2005 and 2011 and reported 3.5% of those who underwent primary THA had an unplanned readmission within 30 days. Another study by Kurtz and colleaguesCitation37 used the Medicare national hospital claims database to identify 442,333 older patients (aged ≥65 years) who underwent primary THA in 3730 US hospitals between 2010 and 2013 and reported a median 30 day readmission rate of 5.8%.
The retrospective nature of data collection and possibility of coding inaccuracies in the administrative database represent important limitations of our study. Data on patient outcomes at our institution may not be generalizable to other institutions because factors that may have an impact on postsurgical outcomes, such as patient demographics, baseline comorbidities, THA technique performed, and the postsurgical pain management protocol used, may differ between patient populations. The analyses of hospital charges and costs were limited by having financial information available only for a subset of patients. Extrapolation of the findings from our study to a larger or more heterogeneous population may also be limited. For example, geographic location and hospital volume can affect readmission ratesCitation37. The readmission rates observed in our study may have been underestimated if some patients were rehospitalized at another institution.
Conclusion
In this retrospective cohort study of patients undergoing THA, the use of liposomal bupivacaine was associated with improvement in the postsurgical outcomes of distance walked, LOS, consumption of opioid rescue medication, pain scores, and hospital charges compared with the historical standard of care. Large, randomized, controlled, prospective studies would be helpful in further clarifying postsurgical clinical and economic outcomes from this study.
Transparency
Declaration of funding
This manuscript was funded by Pacira Pharmaceuticals.
Declaration of financial/other relationships
C.V.A. has disclosed that he is a member of the Health Outcomes and Economics Advisory Board for Pacira Pharmaceuticals Inc. Pacira Pharmaceuticals Inc. is the manufacturer of Exparel. J.R., M.K., K.G., M.M., C.S.K. and B.T.M. have disclosed that they have no significant relationships with or financial interests in any commercial companies related to this study or article.
CMRO peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Acknowledgements
Editorial and medical writing assistance was provided by Michael D. Morren RPh MBA of Peloton Advantage LLC, supported by Pacira Pharmaceuticals Inc. The authors were fully responsible for the content, editorial decisions, and opinions expressed in the current article. The authors did not receive an honorarium related to the development of this manuscript.
Note
Notes
1 Exparel is a registered trade name of Pacira Pharmaceuticals Inc., Parsippany, NJ, USA
References
- Centers for Disease Control and Prevention. Number of all-listed procedures for discharges from short-stay hospitals, by procedure category and age: United States, 2010. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberprocedureage.pdf [Last accessed 21 July 2016]
- Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 2014;73:1323-30
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5
- Cherian JJ, Barrington J, Elmallah RK, et al. Liposomal bupivacaine suspension, can reduce length of stay and improve discharge status of patients undergoing total hip arthroplasty. Surg Technol Int 2015;27:235-39
- Barrington JW, Halaszynski TM, Sinatra RS; for the Expert Working Group on Anesthesia and Orthopaedics: Critical Issues in Hip and Knee Replacement Arthroplasty. Perioperative pain management in hip and knee replacement surgery. Am J Orthop 2014;43:S1-S16
- Barrington JW, Dalury DF, Emerson RH Jr, et al. Improving patient outcomes through advanced pain management techniques in total hip and knee arthroplasty. Am J Orthoped 2013;42:S1-S17
- Hojer Karlsen AP, Geisler A, Petersen PL, et al. Postoperative pain treatment after total hip arthroplasty: a systematic review. Pain 2015;156:8-30
- American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology 2012;116:248-73
- Raiff D, Vaughan C, McGee A. Impact of intraoperative acetaminophen administration on postoperative opioid consumption in patients undergoing hip or knee replacement. Hosp Pharm 2014;49:1022-32
- Husted H, Lunn TH, Troelsen A, et al. Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthop 2011;82:679-84
- Centers for Medicare & Medicaid Services. HCAHPS: Patients’ Perspectives of Care Survey. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-patient-assessment-instruments/hospitalqualityinits/hospitalhcahps.html [Last accessed 21 July 2016]
- Centers for Medicare & Medicaid Services. Medicare program; hospital inpatient value-based purchasing program. Final rule. Fed Regist 2011;76:26490-547
- Centers for Medicare & Medicaid Services. HCAHPS Survey. Available at: http://www.hcahpsonline.org/files/March%202016_Survey%20Instruments_English_Mail.pdf [Last accessed 13 September 2016]
- McCarthy D, Iohom G. Local infiltration analgesia for postoperative pain control following total hip arthroplasty: a systematic review. Anesthesiol Res Pract 2012;2012:709531
- Joshi GP, Beck DE, Emerson RH, et al. Defining new directions for more effective management of surgical pain in the United States: highlights of the Inaugural Surgical Pain Congress. Am Surg 2014;80:219-28
- Jimenez-Almonte JH, Wyles CC, Wyles SP, et al. Is local infiltration analgesia superior to peripheral nerve blockade for pain management after THA: a network meta-analysis. Clin Orthop Relat Res 2016;474:495-516
- Golembiewski J, Dasta J. Evolving role of local anesthetics in managing postsurgical analgesia. Clin Ther 2015;37:1354-71
- Exparel [prescribing information]. Parsippany, NJ: Pacira Pharmaceuticals Inc., 2015
- Bergese SD, Ramamoorthy S, Patou G, et al. Efficacy profile of liposome bupivacaine, a novel formulation of bupivacaine for postsurgical analgesia. J Pain Res 2012;5:107-16
- Dasta J, Ramamoorthy S, Patou G, Sinatra R. Bupivacaine liposome injectable suspension compared with bupivacaine HCl for the reduction of opioid burden in the postsurgical setting. Curr Med Res Opin 2012;28:1609-15
- Viscusi ER, Sinatra R, Onel E, Ramamoorthy SL. The safety of liposome bupivacaine, a novel local analgesic formulation. Clin J Pain 2014;30:102-10
- Barrington JW, Olugbode O, Lovald S, et al. Liposomal bupivacaine: a comparative study of more than 1000 total joint arthroplasty cases. Orthop Clin North Am 2015;46:469-77
- Kharitonov V. A review of the compatibility of liposome bupivacaine with other drug products and commonly used implant materials. Postgrad Med 2014;126:129-38
- Crawford M, Church J, Akin B. CPI Detailed Report: Data for December 2015. Available at: http://www.bls.gov/cpi/cpid1512.pdf [Last accessed 10 November 2016]
- Medicare Acute Inpatient PPS FY 2013 Final Rule Data Files. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Downloads/FY_13_FR_Impact_File.zip [Last accessed 10 November 2016]
- Kirkness CS, Asche CV, Ren J, et al. Assessment of liposome bupivacaine infiltration versus continuous femoral nerve block for postsurgical analgesia following total knee arthroplasty: a retrospective cohort study. Curr Med Res Opin 2016;32:1727-33
- Domb BG, Gupta A, Hammarstedt JE, et al. The effect of liposomal bupivacaine injection during total hip arthroplasty: a controlled cohort study. BMC Musculoskelet Disord 2014;15:310
- Springer BD. Transition from nerve blocks to periarticular injections and emerging techniques in total joint arthroplasty. Am J Orthop (Belle Mead NJ) 2014;43:S6-S9
- Lombardi AV Jr. Recent advances in incorporation of local analgesics in postsurgical pain pathways. Am J Orthop (Belle Mead NJ) 2014;43:S2-S5
- Emerson RH, Barrington JW, Olugbode O, et al. Comparison of local infiltration analgesia to bupivacaine wound infiltration as part of a multimodal pain program in total hip replacement. J Surg Orthop Adv 2015;24:235-41
- Yu SW, Szulc AL, Walton SL, et al. Liposomal bupivacaine as an adjunct to postoperative pain control in total hip arthroplasty. J Arthroplasty 2016;31:1510-15
- Ramos NL, Karia RJ, Hutzler LH, et al. The effect of discharge disposition on 30-day readmission rates after total joint arthroplasty. J Arthroplasty 2014;29:674-7
- Nichols CI, Vose JG. Clinical outcomes and costs within 90 days of primary or revision total joint arthroplasty. J Arthroplasty 2016;31:1400-6
- Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clin Orthop Relat Res 2014;472:188-93
- Centers for Medicare & Medicaid Services. Medicare program; Comprehensive Care for Joint Replacement payment model for acute care hospitals furnishing lower extremity joint replacement services. Final rule. Fed Regist 2015;80:73273-554
- Schairer WW, Sing DC, Vail TP, Bozic KJ. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res 2014;472:464-70
- Kurtz SM, Lau EC, Ong KL, et al. Hospital, patient, and clinical factors influence 30- and 90-day readmission after primary total hip arthroplasty. J Arthroplasty 2016;31:2130-8

