Abstract
Background: The adolescent growth spurt is associated with an increased risk of injury in young athletes.
Aim: This study aimed to use an interdisciplinary collaboration between technical coaches, sports scientists, and medical staff to mitigate this risk.
Subjects and methods: 77 male academy footballers were followed across two seasons. At-risk players were identified using somatic maturity status and growth rate in stature and the lower limbs, using thresholds of 88% to 92.8% of predicted adult stature, ≥7.2 cm/year, and ≥3.6 cm/year, respectively. During the 2019–20 season, players with symptoms of a growth-related injury or two of three risk factors were included in an intervention strategy that included modified training load, football-specific skills, balance, coordination and landing drills, and an individualised strength program.
Results: For players with the three risk factors, there was a significant reduction in the incidence (rate ratio [RR] = 0.14 (5.2 per 1000h → 0.8 per 1000h, p = 0.05) and burden (RR = 0.08 (216 per 1000h → 17 per 1000h, p = 0.02) between the seasons. For players with ≤2 risk factors, there were no significant differences in injury risk between the baseline and intervention seasons.
Conclusion: Overall, it may be possible to mitigate injury incidence and burden during the adolescent growth spurt in high-risk athletes.
Introduction
A key objective in academy football is the reduction of injury incidence, severity, and burden during the adolescent growth spurt (Read et al. Citation2018; Hall et al. Citation2020). Injuries are of paramount importance as they result in reduced playing and training time and, thus, hinder player development (Larruskain et al. Citation2022). Injuries may also impact players physically and psychologically, increasing the likelihood of future injuries, health problems, drop-out, and/or burnout (Tveit et al. Citation2012; DiFiori et al. Citation2014). The adolescent growth spurt describes a period of accelerated growth in stature that follows the onset of puberty. The most rapid point of growth is referred to as peak height velocity (PHV), which occurs, on average, at 13.8 years in males, however, there is a considerable inter-individual variation of up to 4 to 6 years (Malina et al. Citation2004). During this phase, individuals experience concurrent changes in limb length, limb mass, moments of inertia and functional capacity (Hawkins and Metheny Citation2001; Adirim and Cheng Citation2003). As a result of these collective changes, adolescents may also experience temporary delays or regressions in sensorimotor mechanisms and motor control (Quatman-Yates et al. Citation2012), which may also adversely impact injury risk.
Growth is defined as an increase in the size of the body as a whole or a specific part of the body (Malina et al. Citation2004). Biological maturation is defined as the timing and tempo of progress towards an adult biological state and maturity status is the level of maturity at a given time point (e.g. circa-PHV) (Malina et al. Citation2004; Malina Citation2011). Growth-related injuries have been shown to be prevalent in youth footballers (Jones et al. Citation2019). In general population adolescents, growth-related injuries have been shown to have lasting negative effects on strength and endurance function (Kaya et al. Citation2013; Rathleff et al. Citation2020a, Citation2020b) that remain after the resolution of symptoms (Pihlajamäki et al. Citation2009). Research has previously identified three risk factors that are associated with an increased likelihood of injury during adolescence. The first is maturation status (Van der Sluis et al. Citation2014; Bult et al. Citation2018; Johnson et al. Citation2020), with the period of circa PHV (identified as between 88–92% of predicted adult stature) being associated with an increased injury incidence and burden (Johnson et al. Citation2020). Monasterio et al. (Citation2023) found that growth-related injuries had the highest burden circa-PHV. Although, this study also demonstrated a higher overall injury burden post-PHV due to the increased burden of muscle and ligament injuries in this group (Monasterio et al. Citation2023). The second risk factor is the rate of growth in stature; Kemper et al. (Citation2015) suggested that athletes growing above 7.2 cm/year were at greater risk for injury. Similarly, in adolescent track and field athletes, Wik et al. (Citation2020) found a greater growth rate in stature was associated with an increased risk of bone and growth plate injuries. The third risk factor that is associated with an increased likelihood of overuse injury is lower limb growth rate (Rommers et al. Citation2020). In high‑level male youth footballers, where most injuries (72% to 93%) are in the lower limbs (Jones et al. Citation2019), information about the growth of specific body dimensions, such as the lower limbs, could be of practical value. Moreover, Wik et al. (Citation2020) also found that lower-limb growth rate was associated with a greater risk of bone and growth plate injuries in track and field athletes. Building upon previous literature on risk factors for injury in adolescent athletes, Johnson et al. (Citation2022) explored the influence of growth rate, lower-limb growth rate, and percentage of predicted adult stature on time-loss injury risk. This study reported a significant positive linear relationship between both growth rate and lower limb growth rate with injury incidence. More specifically, there was a significantly greater likelihood of injury for players with a growth rate ≥7.2 cm/year. For both injury incidence and burden, there was a significant non-linear relationship with the percentage of predicted adult stature, with peak risk occurring at 92% and 95% of predicted adult stature, respectively. Accordingly, the evidence suggests practitioners should consider growth rates, lower limb growth rates, maturity status, and training loads if they are seeking to reduce injury risk and incidence in youth football players.
The risks associated with growth and maturation have been established, however, there is limited evidence on practical solutions to address these risks (McKay et al. Citation2019). In an attempt to mitigate growth-related injuries in nine highly-trained youth squash players, training loads were reduced for ‘at-risk’ players with symptoms and this intervention resulted in fewer training days being lost due to growth-related problems (Horobeanu et al. Citation2017). However, these findings are yet to be replicated in a full, peer-reviewed study. Nonetheless, the early detection of at-risk adolescent athletes and the prescription of developmentally appropriate training load and content could reduce injury prevalence and burden during the adolescent growth spurt, as well as reduce future negative health consequences. In addition to safeguarding the athletes, such an intervention would allow continued training through the adolescent growth spurt, at a reduced or modified level. Several strategies could allow for the better identification and management of young athletes during the growth spurt. The first stage of managing players at risk of injury is reducing aggravating mechanisms and giving sufficient recovery time will allow symptoms to settle (Circi et al. Citation2017). Another consideration is variation in the type of load placed on the players; the athletic skills model advocates a greater variation in the exercises, to reduce the physical monotony of programmes (Savelsbergh and Wormhoudt Citation2018). This is a logical solution as the prevalence of OSD is four times greater in individuals who have specialised in their sport early (Hall et al. Citation2015). It is, therefore, important to continue to train physical qualities during this time (Moran et al. Citation2017). Moreover, using impact attenuation allows individuals to efficiently absorb the energy from the impact of jumping, which could benefit adolescent athletes as insufficient impact attenuation could result in overloading tissues and subsequently increase injury risk (Steffen et al. Citation2007).
The available evidence suggests an intervention designed to reduce injuries in adolescent soccer players during the growth spurt should include; modification of training load, balance, coordination and landing drills, and an individualised strength program. A suggested method of dealing with injuries in applied settings is the “iterative sequence of prevention” approach (Tee et al. Citation2018). This approach involves an interdisciplinary collaboration between technical coaches, sports scientists, and medical staff to have a meaningful impact on injury risk (Tee et al. Citation2018). Therefore, this study aims to use interdisciplinary collaboration to mitigate this risk in adolescent academy footballers. More specifically, the effect of identifying at-risk adolescent footballers using growth rate, lower-limb growth rate, and maturity and subsequently modifying their training to reduce injury risk.
Materials and methods
An opportunity sample of seventy-seven male academy footballers aged 12 to 16 years, representing players across four age groups (U13 – U16) within an English professional football club’s academy took part in this study. No a priori sample size calculation was conducted; however, Bahr and Holme (Citation2003) suggest that 20–50 injury cases are needed to detect moderate-to-strong associations between risk factors and injury, and thus this sample size was deemed adequate for this purpose. Ethical approval was gained from the University of Bath’s Research Ethics Approval Committee for Health (EP 19/20 002). Participants and their parents and guardians provide assent and consent, respectively, for the data collection.
The anthropometric data were collected consistent with the International Society for the Advancement of Kinanthropometry (ISAK) guidelines (Silva and Vieira Citation2020). Each player’s stature, seated stature, and mass were measured by the same trained staff member 3 to 5 times per year. Estimated leg length was also calculated by subtracting seated height from stature. The staff member’s absolute and relative intra-rater typical error of measurement for standing stature was 0.03 cm and 0.02%, and for seated stature was 0.02 cm and 0.02%, respectively (Perini et al. Citation2005). The growth rate and lower limb growth rate were calculated for each player as the change in stature or estimated leg length over the change in time (years). This rate was then inputted on the midpoint between the two measurements and smoothed using a Bessel spline. An estimated growth rate and lower limb growth rate were computed for each day, aligning with the training exposures and injury data. The growth rate was split into a high (>7.2 cm/year) and a low (<7.2 cm/year) (Kemper et al. Citation2015; Johnson et al. Citation2022). The lower limb growth rate was also split into a high (>3.6 cm/year) and a low (<3.6 cm/year) (Johnson et al. Citation2022). The players’ stature, mass, chronological age and mid-parent stature were also used to predict the adult stature of each player (Khamis and Roche Citation1994). Each player’s biological parents’ statures were self-reported and adjusted for over-estimation (Epstein et al. Citation1995). The player’s current stature was then expressed as a percentage of predicted adult stature as an index of somatic maturation (Roche et al. Citation1983). A Bessel spline was used to provide a percentage of predicted adult stature data points for each day within the season. A percentage of predicted adult stature of 88% to 92% was used to identify the phase of circa-PHV, to provide a narrow bandwidth of around 90%, which is when the peak rate of adolescent growth occurs (Sanders et al. Citation2017). For statistical analysis values of 88% to 92.8% were used, as during the 3-month intervention stage the average increase in the percentage of predicted adult stature was 0.8%. This was important to reduce false negatives (i.e. a player is included in the intervention but their data is being analysed as part of the non-intervention group).
As with the growth and maturation data, the injury data were collected following procedures previously described by Johnson et al. (Citation2022). Total exposure was calculated as the sum of training, match, and gym exposure within the academy. Participants with exposure >2 standard deviations below the mean were excluded as outliers before analysis (Hopkins et al. Citation2009). Time-loss injuries were recorded using the club’s online database by academy medical staff. The injury data were collected in line with the consensus statement for football injury studies (Fuller et al. Citation2006). A time-loss injury was defined as a player being unable to take part in full football training or match play (Fuller et al. Citation2006). Only injuries that occurred in football competitions or training were counted, those unrelated to academy activities were not recorded (Fuller et al. Citation2006). Non-contact injuries were analysed; these were defined as those sustained by a player without extrinsic contact by another player or other object on the field of play (Marshall Citation2010). Injuries are represented as a total value and as the number of injuries per 1000 player-hours (Fuller et al. Citation2006). The injury severity is the number of days elapsed between the initial injury date and the player’s return to full availability for training or matches (Fuller et al. Citation2006). The injury burden is equal to the product of the incidence rate and the mean days missed per injury, giving the number of days missed per 1000 h (Fuller Citation2018).
The current study considered data collected across two consecutive seasons. Season one was the 2018/19 football season and season two was the 2019/20 football season. Seasons one and two were the same in terms of staff, coaching philosophy, and the number of sessions per week (), but the second season finished early due to the 2020 Covid-19 outbreak. The protocol in the first season represented existing club practice to prevent injuries through the growth spurt. This involved the measurement and feedback of growth and maturation to identify at-risk players to the coaches. The training and competition schedule for the players identified as at-risk was not altered. Any changes were made at the coaches’ discretion and medical staff monitored growth-related injuries, reducing the volume for those with ongoing soreness.
Table 1. The club’s training schedule for the 2019/20 season. The type of training (planned minutes) is provided for each day and age-group (Johnson et al. Citation2022) (S&C: strength and conditioning).
The injury prevention protocol was implemented in the second season and was developed through an iterative sequence of prevention-related activities and strategies. The process involved identifying injury risk factors, then conducting a focus group, including coaches, key stakeholders, medical and sports science staff to discuss the current practice for managing training load during the growth spurt. Two key types of risk factors were identified before the intervention. Firstly, medical personnel assessed for soreness upon palpation of common growth-related injury sites (including OSD, Severs Disease, and Sinding-Larsen-Johansson syndrome). These we classified as those stated above and were diagnosed by the same medical professional across the study period. Soreness for all players was measured at the start of each intervention period and measured on the scale provided by Rathleff et al. Citation2020a, Citation2020b. These injuries require a modified training schedule to allow players to continue to train, so they were included in the intervention group to alleviate soreness. These modifications took place on Wednesday for the U13/U14 group and Monday for the U15/U16 group. The other was growth and maturation risk factors; a percentage of predicted adult stature between 88-92%, a growth rate of greater than 7.2 cm/year, and a lower limb growth rate greater than 3.6 cm/year (Johnson et al. Citation2022). If players had soreness upon palpation or at least 2 of the 3 growth and maturation risk factors, they were placed into the intervention group.
The second season included two intervention phases to account for those participants who changed in their ‘at risk status’ due to changes in growth, maturity status, or soreness. In total 14 players were identified as at-risk, 8 of these players were identified as at-risk in both stages and, thus, participated in the intervention across the season. Both phases contained the same intervention, phase one included 12 players occurring between August to November. Phase two included ten players occurring between November and February.
All players in both groups (intervention and regular training) participated in a standardised warm-up. The warm-up involved football-specific technical drills on arrival, followed by activation, mobilisation, and potentiation conducted by the strength and conditioning coach. The intervention activities were designed to be fun whilst still football and individual-specific, aiming to reduce the risk of overuse injury while maximising opportunities to improve performance. The intervention activities targeted four key areas; 1) modified training load (e.g. reduced accelerations and decelerations, reduced impacts and ground contacts), 2) football-specific technical skills (e.g. ball manipulation and passing challenges), 3) balance, coordination, and landing mechanics, including impact attenuation, 4) and an individualised strength program. The total time of the sessions was 90 min to match the “normal” training schedule. Therefore, training volume was not decreased but rather the intensity as collected through ratings of perceived exertion was reduced.
A questionnaire (Appendix 1) consisting of twelve items including both open and Likert questions was used to gain a deeper insight into players’ experiences of the intervention. Each item was developed based on the researchers’ perceived advantages and disadvantages of the intervention. Of the 14 players included in the intervention periods, 9 agreed to participate in the feedback surveys. Single items cannot be tested for internal reliability but are valid estimates of relevant constructs and can exceed the validity coefficients of multiple-item scales (Burisch Citation1984; Russell et al. Citation1989; Raffety et al. Citation1997). Additionally, single-item measures are equally valid when measuring contextual differences within a construct that is sufficiently narrow and/or unambiguous (Wanous et al. Citation1997). Questions 2, 3, and 4 were open-ended to assess what players enjoyed, did not enjoy, and would have improved, respectively. These questions allowed participants the opportunity to add qualitative comments concerning the intervention. Question 5 assessed whether the players would choose to participate in the intervention again, with a simple yes, no answer.
All analysis was performed using R (version 4.0.5, R Foundation for Statistical Computing, Vienna, Austria). Generalised linear mixed-effects models were fitted using the lme4 package (Bates et al. Citation2014), to compare both seasons and model the association between growth rate, lower-limb growth rate, and maturity status upon estimated injury likelihood. Symptomology was not included as part of this analysis due to missing data. For injury incidence analyses, daily injury and risk factor data and a binomial distribution and log-link function were used. For injury burden analyses, data were grouped into weekly values, with the dependent variable being the count of days missed each week, with a Poisson distribution, log-link function, and exposure offset used. Predictor variables were modelled as categorical variables, using the groups highlighted above. Player ID was included as a random effect to account for repeated observations. For the models, statistical significance was set at p ≤ 0.05. To compare between seasons estimated marginal means and Rate Ratios (RR) were used (Lenth Citation2022), with statistical significance set at p ≤ 0.05.
One sample means t-tests were conducted for items 1 and 6–12 to determine the degree to which the players agreed or disagreed with the statements about the intervention. For each item, the observed mean was compared with the response that indicated no difference between the intervention and normal age-group training (i.e. 3, “neither agree nor disagree”). Cohens D effect sizes and 95% Confidence Intervals were presented, with calculations performed using pooled standard deviations via the effect size package (Ben-Shachar et al. Citation2020). Pre-determined upper and lower equivalence bounds of ±0.25 determined if the differences were worthy of practical consideration (Lakens et al. Citation2018).
Results
Across both seasons, there were a total of 89 injuries, a rate of 5.52 (95% CI: 4.48 − 6.79) per 1000 h, a mean severity of 38 (95% CI: 31—47) days, and an injury burden of 209 (95% CI: 170 – 258) per 1000 h. shows the comparison between seasons (2018–19 and 2019–20); no significant differences were found. A between-season and age groups comparison for injury incidence, severity, and burden can be found in ; the only significant difference observed between 2018–19 (pre-intervention) and 2019–20 (intervention) was a greater injury burden in the U16 group.
Table 2. Injury counts, incidence rates, mean severity, and injury burden for each season, 2018-19 (pre-intervention) and 2019–20 (intervention) (95% Confidence Intervals Lower – Upper).
Table 3. Comparison between seasons for injury counts, incidence rates, mean severity, and injury burden for each age group (95% Confidence Intervals Lower – Upper), * highlighting a significant difference between 2018–19 (pre-intervention) and 2019–20 (intervention).
Figure 1. A heat map showing the combined effects of Growth Rate and Percentage of Predicted Adult Stature on estimated injury likelihood for the whole sample in A) 2018–19 season (pre-intervention) and B) 2019–20 season (intervention).
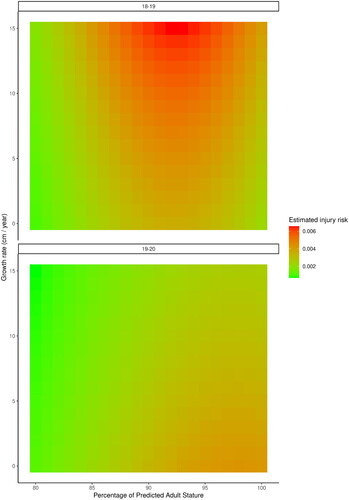
Figure 2. A heat map showing the combined effects of Growth Rate and Percentage of Predicted Adult Stature on estimated injury burden for the whole sample in A) 2018–19 season (pre-intervention) and B) 2019–20 season (intervention).
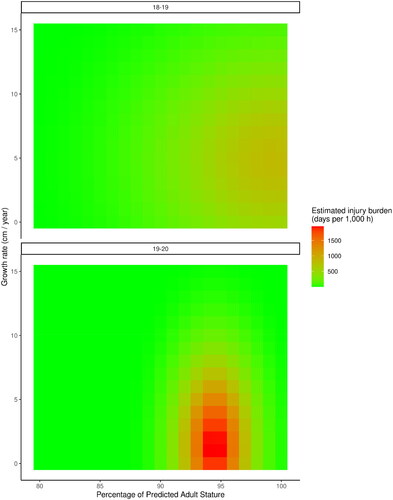
Table 4. Comparison between seasons for injury counts, incidence rates, mean severity, and injury burden for each level of risk factor (95% Confidence Intervals Lower – Upper), * highlighting a significant difference between 2018–19 (pre-intervention) and 2019–20 (intervention).
Discussion
This study aimed to describe the process and outcomes of an iterative injury prevention approach in academy football. Moreover, the intervention identified at-risk adolescent footballers using growth rate, lower-limb growth rate and maturity, then made developmentally appropriate training load and content modifications. For players at greatest risk (three risk factors), there was a significant reduction in injury incidence and burden between the 2018–19 (pre-intervention) and 2019–20 (intervention) seasons. There were 5.2 injuries per 1000 h in 2018–19 (pre-intervention) and 0.8 injuries per 1000 h in 2019-–20 (intervention), which represents an 86% reduction in injury incidence. For injury burden, there were 216 days missed per 1000 h in 2018–19 (pre-intervention) and 17 days missed per 1000 h in 2019–20 (intervention), which represents a 92% reduction in injury burden. This shows that the intervention had the desired impact on the players who were at the most risk in the initial analysis (Johnson et al. Citation2022). This finding informs practice by suggesting that football academies should monitor all three risk factors and adapt training programmes where appropriate.
The injury incidence heat map illustrates how the risk has changed between the two seasons, with the first season having a high injury incidence at high growth rates and circa-PHV, whereas, the 2019–20 season (intervention) has a greater injury incidence at low growth rates post-PHV. Future iterations of this injury prevention process should seek to implement strategies aimed at preventing severe injuries post-PHV (Hall et al. Citation2022), for example muscle and ligament injuries (Monasterio et al. Citation2023). This study represents the first intervention to show a reduction in injury incidence and injury burden risk during periods of accelerated growth (PHV and high growth rate) in academy football. Further research is, however, warranted to validate these findings.
Players with two of three risk factors were also included in the intervention. For this group, injury incidence rates were reduced in the second season, but these differences were not significant. For injury burden, there was an increase in the second season but these differences were also not significant and may have been skewed by a small number of severe injuries. These findings in combination suggest that the intervention had a smaller or potentially negative effect on players with two of three risk factors. This is expected, as these players were not at as high of a risk in the previous season (Johnson et al. Citation2022) and the intervention had a smaller potential for injury reduction. For players with two risk factors, multi-disciplinary teams should monitor these players closely and use further information about their injury risk and training programme to make adjustments (e.g. recent training loads, previous injury history, and well-being). For players with zero or one growth and maturation risk factor, there was no significant difference in injury incidence or injury burden between seasons. These players had the same schedule and training in both seasons; these findings highlight that the two seasons were similar in terms of baseline injury rates. The survey results suggest that players understood the purpose of the intervention and felt that the intervention allowed them to perform better in training and games. This demonstrates that the intervention was perceived as an acceptable and viable solution by the end users, which is an important consideration in youth injury research (Appendix 2 and 3) (Donaldson and Finch Citation2012).
The results of this study should be acknowledged with caution as they are from a small sample at one football academy. Moreover, the results are context-dependent, and it was an iterative sequence of prevention rather than a controlled trial. It also should be noted that the effectiveness of interventions when transferred between contexts is uncertain. Tee et al. (Citation2020) subsequently suggest that to manage injury in different contexts an iterative sequence of prevention in response to emergent injury outcomes should be used. This limitation could also be seen as a strength in that it allowed access to an elite environment where reducing injury rates has a real-world impact on future progression. This limitation also relates to whether this study can be applied more broadly, which is even more difficult to predict. The intervention was designed by the specific members of the academy and for the context in which they work, so there is no guarantee that this intervention would work in another context (O’Brien and Finch 2019). Furthermore, work is required to investigate similar strategies in other sports and populations (e.g. females). Nonetheless, the authors do believe that practitioners should seek to use the team sports prevention cycle (O’Brien et al. Citation2019) and iterative sequence of prevention (Tee et al. Citation2019) to reduce injuries in elite sports environments. Moreover, players’ symptomology was not analysed in the present study due to missing data; this information could further contribute to the effects seen in this study. Moreover, ultrasound or other objective methods were not used to diagnose growth-related injuries, this could be utilised in future studies. Future research should further analyse existing risk factors (e.g. percentage of predicted adult height at different bands) and other risk factors (e.g. reported symptomology, fatigue) that may contribute to the identification of players at greatest risk. The authors would recommend that those working in youth sports should specifically consider the effect of the growth spurt on injuries and how training should be managed during this phase. Based on existing literature and the findings of the present study, the key recommendations for practitioners for managing ‘at-risk’ players during the growth spurt include modifying the training load; the addition of balance, coordination and landing drills; and an individualised strength program.
Overall, this study has shown that an iterative sequence of prevention applied in a youth football academy can significantly reduce the injury incidence and burden during the growth spurt. Practitioners should consider how they can incorporate such prevention protocols into their environment to aid youth athletic development. The results of the study also support the need to consider individual differences in growth and maturation in the design, prescription, and implementation of training programmes for young athletes.
Supplemental Material
Download PDF (387.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author, [DJ], upon reasonable request.
Additional information
Funding
References
- Adirim TA, Cheng TL. 2003. Overview of injuries in the young athlete. Sports Med. 33(1):75–81. doi: 10.2165/00007256-200333010-00006.
- Bahr R, Holme I. 2003. Risk factors for sports injuries–a methodological approach. Br J Sports Med. 37(5):384–392. doi: 10.1136/bjsm.37.5.384.
- Bates D, Mächler M, Bolker B, Walker S. 2014. Fitting linear mixed-effects models using lme4. arXiv preprint arXiv:1406.5823.
- Ben-Shachar MS, Lüdecke D, Makowski D. 2020. Effectsize: estimation of effect size indices and standardized parameters. JOSS. 5(56):2815. doi: 10.21105/joss.02815.
- Bult HJ, Barendrecht M, Tak IJR. 2018. Injury risk and injury burden are related to age group and peak height velocity among talented male youth soccer players. Orthop J Sports Med. 6(12):1–10. eng.
- Burisch M. 1984. Approaches to personality inventory construction: a comparison of merits. Am Psychol. 39(3):214–227. doi: 10.1037/0003-066X.39.3.214.
- Circi E, Atalay Y, Beyzadeoglu T. 2017. Treatment of Osgood-Schlatter disease: review of the literature. Musculoskelet Surg. 101(3):195–200. doi: 10.1007/s12306-017-0479-7.
- DiFiori JP, Benjamin HJ, Brenner JS, Gregory A, Jayanthi N, Landry GL, Luke A. 2014. Overuse injuries and burnout in youth sports: a position statement from the American medical society for sports medicine. Br J Sports Med. 48(4):287–288. doi: 10.1136/bjsports-2013-093299.
- Donaldson A, Finch CF. 2012. Planning for implementation and translation: seek first to understand the end-users’ perspectives. Br J Sports Med. 46(5):306–307. doi: 10.1136/bjsports-2011-090461.
- Epstein LH, Valoski AM, Kalarchian MA, McCurley J. 1995. Do children lose and maintain weight easier than adults: a comparison of child and parent weight changes from six months to ten years. Obes Res. 3(5):411–417. doi: 10.1002/j.1550-8528.1995.tb00170.x.
- Fuller CW. 2018. Injury risk (burden), risk matrices and risk contours in team sports: a review of principles, practices and problems. Sports Med. 48(7):1597–1606. doi: 10.1007/s40279-018-0913-5.
- Fuller CW, Ekstrand J, Junge A, Andersen TE, Bahr R, Dvorak J, Hägglund M, McCrory P, Meeuwisse WH. 2006. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scand J Med Sci Sports. 16(2):83–92. doi: 10.1111/j.1600-0838.2006.00528.x.
- Hall ECR, Larruskain J, Gil SM, Lekue JA, Baumert P, Rienzi E, Moreno S, Tannure M, Murtagh CF, Ade JD, et al. 2020. An injury audit in high-level male youth soccer players from English, Spanish, Uruguayan and Brazilian academies. Phys Ther Sport. 44:53–60. doi: 10.1016/j.ptsp.2020.04.033.
- Hall ECR, Larruskain J, Gil SM, Lekue JA, Baumert P, Rienzi E, Moreno S, Tannure M, Murtagh CF, Ade JD, et al. 2022. Injury risk is greater in physically mature versus biologically younger male soccer players from academies in different countries. Phys Ther Sport. 55:111–118. doi: 10.1016/j.ptsp.2022.03.006.
- Hall R, Foss KB, Hewett TE, Myer GD. 2015. Sport specialization’s association with an increased risk of developing anterior knee pain in adolescent female athletes. J Sport Rehabil. 24(1):31–35. doi: 10.1123/jsr.2013-0101.
- Hawkins D, Metheny J. 2001. Overuse injuries in youth sports: biomechanical considerations. Med Sci Sports Exerc. 33(10):1701–1707. doi: 10.1097/00005768-200110000-00014.
- Hopkins WG, Marshall SW, Batterham AM, Hanin J. 2009. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. 41(1):3–13. doi: 10.1249/MSS.0b013e31818cb278.
- Horobeanu C, Jones T, Johnson A. 2017. Can we limit training days lost due to Osgood Schlatters disease in junior squash athletes? Br J Sports Med. 51(4):331.2–332. doi: 10.1136/bjsports-2016-097372.122.
- Johnson DM, Cumming SP, Bradley B, Williams S. 2023. How much training do English male academy players really do? Load inside and outside of a football academy. Int J Sports Sci Coach. 18(4):1123–1131. doi: 10.1177/17479541221101847.
- Johnson DM, Cumming SP, Bradley B, Williams S. 2022. The influence of exposure, growth and maturation on injury risk in male academy football players. J Sports Sci. 40(10):1127–1136. doi: 10.1080/02640414.2022.2051380.
- Johnson DM, Williams S, Bradley B, Sayer S, Murray Fisher J, Cumming S. 2020. Growing pains: maturity associated variation in injury risk in academy football. Eur J Sport Sci. 20(4):544–552. doi: 10.1080/17461391.2019.1633416.
- Jones S, Almousa S, Gibb A, Allamby N, Mullen R, Andersen TE, Williams M. 2019. Injury incidence, prevalence and severity in high-level male youth football: a systematic review. Sports Med. 49(12):1901–1899. doi: 10.1007/s40279-019-01169-8.
- Kaya DO, Toprak U, Baltaci G, Yosmaoglu B, Ozer H. 2013. Long-term functional and sonographic outcomes in Osgood-Schlatter disease. Knee Surg Sports Traumatol Arthrosc. 21(5):1131–1139. doi: 10.1007/s00167-012-2116-1.
- Kemper GL, van der Sluis A, Brink MS, Visscher C, Frencken WG, Elferink-Gemser MT. 2015. Anthropometric injury risk factors in elite-standard Youth soccer. Int J Sports Med. 36(13):1112–1117. doi: 10.1055/s-0035-1555778.
- Khamis HJ, Roche AF. 1994. Predicting adult stature without using skeletal age: the Khamis-Roche method. Pediatrics. 94(4):504–507.
- Lakens D, Scheel AM, Isager PM. 2018. Equivalence testing for psychological research: a Tutorial. Adv Methods Pract Psychol Sci. 1(2):259–269. doi: 10.1177/2515245918770963.
- Larruskain J, Lekue JA, Martin-Garetxana I, Barrio I, McCall A, Gil SM. 2022. Injuries are negatively associated with player progression in an elite football academy. Sci Med Footb. 6(4):405–414. doi: 10.1080/24733938.2021.1943756.
- Lenth RV. 2022. Emmeans: Estimated Marginal Means, aka Least-Squares Means. R package version 1.7.2. [accessed]. https://github.com/rvlenth/emmeans.
- Malina RM. 2011. Skeletal age and age verification in youth sport [journal article. Sports Med. 41(11):925–947. doi: 10.2165/11590300-000000000-00000.
- Malina RM, Bouchard C, Bar-Or O. 2004. Growth, maturation, and physical activity. 2nd ed. Champaign (IL): Human Kinetics.
- Marshall SW. 2010. Recommendations for defining and classifying anterior cruciate ligament injuries in epidemiologic studies. J Athl Train. 45(5):516–518. doi: 10.4085/1062-6050-45.5.516.
- McKay CD, Cumming SP, Blake T. 2019. Youth sport: friend or foe? Best Pract Res Clin Rheumatol. 33(1):141–157. doi: 10.1016/j.berh.2019.01.017.
- Monasterio X, Gil SM, Bidaurrazaga-Letona I, Lekue JA, Santisteban JM, Diaz-Beitia G, Lee DJ, Zumeta-Olaskoaga L, Martin-Garetxana I, Bikandi E, et al. 2023. The burden of injuries according to maturity status and timing: a two-decade study with 110 growth curves in an elite football academy. Eur J Sport Sci. 23(2):267–277. doi: 10.1080/17461391.2021.2006316.
- Moran JJ, Sandercock GR, Ramirez-Campillo R, Meylan CM, Collison JA, Parry DA. 2017. Age-related variation in male youth athletes’ countermovement jump after plyometric training: a Meta-analysis of controlled trials. J Strength Cond Res. 31(2):552–565. doi: 10.1519/JSC.0000000000001444.
- OʼBrien J, Finch CF. 2017. Injury prevention exercise programs for professional soccer: understanding the perceptions of the end-users. Clin J Sport Med. 27(1):1–9. doi: 10.1097/JSM.0000000000000291.
- O’Brien J, Finch CF, Pruna R, McCall A. 2019. A new model for injury prevention in team sports: the Team-sport Injury Prevention (TIP) cycle. Sci Med Football. 3(1):77–80. doi: 10.1080/24733938.2018.1512752.
- Perini TA, Oliveira GLd, Ornellas JS, Oliveira FPd. 2005. Technical error of measurement in anthropometry. Rev Bras Med Esporte. 11(1):81–85. doi: 10.1590/S1517-86922005000100009.
- Pihlajamäki HK, Mattila VM, Parviainen M, Kiuru MJ, Visuri TI. 2009. Long-term outcome after surgical treatment of unresolved Osgood-Schlatter disease in young men. J Bone Joint Surg Am. 91(10):2350–2358. eng. doi: 10.2106/JBJS.H.01796.
- Quatman-Yates CC, Quatman CE, Meszaros AJ, Paterno MV, Hewett TE. 2012. A systematic review of sensorimotor function during adolescence: a developmental stage of increased motor awkwardness? Br J Sports Med. 46(9):649–655. doi: 10.1136/bjsm.2010.079616.
- Raffety BD, Smith RE, Ptacek J. 1997. Facilitating and debilitating trait anxiety, situational anxiety, and coping with an anticipated stressor: A process analysis. J Pers Soc Psychol. 72(4):892–906. doi: 10.1037//0022-3514.72.4.892.
- Rathleff MS, Winiarski L, Krommes K, Graven-Nielsen T, Holmich P, Olesen JL, Holden S, Thorborg K. 2020a. Pain, sports participation, and physical function in adolescents with patellofemoral pain and Osgood-Schlatter disease: a matched cross-sectional study. J Orthop Sports Phys Ther. 50(3):149–157. doi: 10.2519/jospt.2020.8770.
- Rathleff MS, Winiarski L, Krommes K, Graven-Nielsen T, Hölmich P, Olesen JL, Holden S, Thorborg K. 2020b. Activity modification and knee strengthening for Osgood-Schlatter disease: a prospective cohort study. Orthop J Sports Med. 8(4):2325967120911106. doi: 10.1177/2325967120911106.
- Read PJ, Oliver JL, De Ste Croix MBA, Myer GD, Lloyd RS. 2018. An audit of injuries in six english professional soccer academies. J Sports Sci. 36(13):1542–1548. doi: 10.1080/02640414.2017.1402535.
- Roche AF, Tyleshevski F, Rogers E. 1983. Non-invasive measurements of physical maturity in children. Res Q Exerc Sport. 54(4):364–371. doi: 10.1080/02701367.1983.10605321.
- Rommers N, Rossler R, Goossens L, Vaeyens R, Lenoir M, Witvrouw E, D’Hondt E. 2020. Risk of acute and overuse injuries in youth elite soccer players: body size and growth matter. J Sci Med Sport. 23(3):246–251. doi: 10.1016/j.jsams.2019.10.001.
- Russell JA, Weiss A, Mendelsohn GA. 1989. Affect grid: a single-item scale of pleasure and arousal. J Pers Soc Psychol. 57(3):493–502. doi: 10.1037/0022-3514.57.3.493.
- Sanders JO, Qiu X, Lu X, Duren DL, Liu RW, Dang D, Menendez ME, Hans SD, Weber DR, Cooperman DR. 2017. The uniform pattern of growth and skeletal maturation during the human adolescent growth spurt. Sci Rep. 7(1):16705. doi: 10.1038/s41598-017-16996-w.
- Savelsbergh GJ, Wormhoudt R. 2018. Creating adaptive athletes: the athletic skills model for enhancing physical literacy as a foundation for expertise. Mov Sport Sci/Sci Mot. (102):31–38. doi: 10.1051/sm/2019004.
- Silva VSd, Vieira MFS. 2020. International Society for the Advancement of Kinanthropometry (ISAK) global: international accreditation scheme of the competent anthropometrist. Rev Bras Cineantropom Desempenho Hum. 22:e70517. doi: 10.1590/1980-0037.2020v22e70517.
- Steffen K, Andersen TE, Bahr R. 2007. Risk of injury on artificial turf and natural grass in young female football players. Br J Sports Med. 41(Suppl 1):i33–i37. doi: 10.1136/bjsm.2007.036665.
- Tee JC, Becker S, Collins R. 2019. The efficacy of an iterative "sequence of prevention" approach to injury prevention by a multidisciplinary team in professional rugby union.
- Tee JC, Bekker S, Collins R, Klingbiel J, Van Rooyen I, Van Wyk D, Till K, Jones B. 2018. The efficacy of an iterative “sequence of prevention” approach to injury prevention by a multidisciplinary team in professional rugby union. J Sci Med Sport. 21(9):899–904. doi: 10.1016/j.jsams.2018.02.003.
- Tee JC, Mclaren S, Jones B. 2020. Sports injury prevention is complex: we need to invest in better processes, not singular solutions. Sports Med. 50(4):689–702. doi: 10.1007/s40279-019-01232-4.
- Tveit M, Rosengren BE, Nilsson J-Å, Karlsson MK. 2012. Former male elite athletes have a higher prevalence of osteoarthritis and arthroplasty in the hip and knee than expected. Am J Sports Med. 40(3):527–533. doi: 10.1177/0363546511429278.
- Van der Sluis A, Elferink-Gemser MT, Coelho-e-Silva MJ, Nijboer JA, Brink MS, Visscher C. 2014. Sport injuries aligned to peak height velocity in talented pubertal soccer players. Int J Sports Med. 35(4):351–355.
- Wanous JP, Reichers AE, Hudy MJ. 1997. Overall job satisfaction: how good are single-item measures? J Appl Psychol. 82(2):247–252. doi: 10.1037/0021-9010.82.2.247.
- Wik EH, Martinez-Silvan D, Farooq A, Cardinale M, Johnson A, Bahr R. 2020. Skeletal maturation and growth rates are related to bone and growth plate injuries in adolescent athletics. Scand J Med Sci Sports. 30(5):894–903. doi: 10.1111/sms.13635.

