Abstract
Background
Chronic hepatitis B virus (HBV) infection is a severe disease affecting the physical and economic well-being of patients. The relationship between polymorphisms in the MTHFR gene and disease progression following HBV infection remains a controversial topic.
Aim
To study MTHFR and MTRR gene polymorphisms in patients with chronic HBV infections in Zigong, Sichuan Province.
Subjects and methods
One hundred and ninety-one patients with chronic HBV infections were divided into three groups: the chronic hepatitis B (CHB) group (n = 71), the hepatitis B-induced liver cirrhosis (LC) group (n = 56), and the hepatitis B-related primary liver cancer (PLC) group (n = 64). The gene polymorphisms were detected using the PCR-melt curve method and analysed.
Results
The distributions of MTHFR C677T (CC: 41.2% vs. 41.8%; CT: 50% vs. 45.5%; TT: 8.8% vs. 12.7%; p = 0.714), MTHFR A1298C (AA: 70.6% vs. 72.7%; AC: 26.5% vs. 25.5%; CC: 2.9% vs. 1.8%; p = 1.000), and MTRR A66G (AA: 58.1% vs. 65.5%; AG: 39.0% vs. 29.1%; 2.9% vs. 5.5%; p = 0.353) genetic polymorphisms did not vary between male and female patients from Zigong. In addition, there were no differences in the distributions of MTHFR C677T (CC: 43.4% vs. 38.8%; CT: 49.1% vs. 48.2%; TT: 7.5% vs. 12.9%; p = 0.444), MTHFR A1298C (AA: 76.4% vs. 64.7%; AC: 20.8% vs. 32.9%; CC: 2.8% vs. 2.4%; p = 0.155), and MTRR A66G (AA: 62.3% vs. 57.6%; AG: 34.0% vs. 38.8%; 3.8% vs. 3.5%; p = 0.353) genetic polymorphisms between the patients <60 and >60 years of age. The distributions of MTHFR C677T (CHB vs. LC, p = 0.888; CHB vs. PLC, p = 0.661; PLC vs. LC, p = 0.926), MTHFR A1298C (CHB vs. LC, p = 0.12; CHB vs. PLC, p = 0.263; PLC vs. LC, p = 0.550), and MTRR A66G (CHB vs. LC, p = 0.955; CHB vs. PLC, p = 0.645; PLC vs. LC, p = 0.355) gene polymorphisms were comparable between the CHB, LC, and PLC groups.
Conclusion
The distributions of MTHFR and MRRR genetic polymorphisms in the population with HBV infections in Zigong, Sichuan Province did not differ in age and sex. The MTHFR and MRRR genetic polymorphisms were comparable between the CHB, LC, and PLC groups.
Introduction
Chronic hepatitis B virus (HBV) infection is a severe disease affecting the physical and economic well-being of patients. Genetic mutations are common in patients with chronic HBV infections. Mutant HBV strains can easily escape the host immune defense and develop resistance to antiviral drugs, which gives rise to more potent pathogenicity. Mutant HBV strains are more likely to induce chronicity and deterioration of hepatitis B and may even lead to cancer (Xu et al. Citation2017).
The 5,10-methylene tetrahydrofolate reductase (MTHFR) gene is polymorphic. The MTHFR C677T polymorphism involves the substitution of cytosine with thymine at nucleotide position 677, while the MTHFR A1298C polymorphism involves the substitution of adenine with cytosine at nucleotide position 1298. Both polymorphisms lead to higher thermal instability and lower MTHFR activity (Zappacosta et al. Citation2014). It has been reported that the MTHFR C677T polymorphism is closely related to the LINE-1 methylation level and the occurrence of hepatocellular carcinoma (HCC) in patients with chronic HBV infections (Qiao et al. Citation2017, Citation2020). Mutations in the 5-methyltetrahydrofolate-homocysteine methyltransferase reductase (MTRR) gene causes an elevation in plasma homocysteine levels. MTRR activity is four-times lower in carriers of the GG genotype compared to the MTRR A66G polymorphism AA genotype (Kwak et al. Citation2008; Lu et al. Citation2018). MTRR mutations are closely related to the risk of HCC. Host gene polymorphism plays an important role in disease progression and outcomes following HBV infection (Kwak et al. Citation2008; Zappacosta et al. Citation2014; Qiao et al. Citation2017, Citation2020; Lu et al. Citation2018). According to another study, however, the MTHFR C677T polymorphism is not a risk factor for HBV-related HCC in those at high risk for HBV (Jiao et al. Citation2017). As concluded in a meta-analysis, the MTHFR rs1801133 polymorphism decreases the susceptibility for HCC (Zhang et al. Citation2020). Indeed, the relationship between polymorphisms in the MTHFR gene and disease progression following HBV infection remains a controversial topic.
Conclusions regarding the distributions of genetic polymorphisms in MTHFR and MTRR vary depending on the research methodology, study region, and study population. In the current study patients with chronic HBV infections from Zigong, Sichuan Province, were enrolled. The genotypes of MTHFR C677T, MTHFR A1298C, and MTRR A66G polymorphism were determined. The purpose of the study was to understand the distribution characteristics of MTHFR and MTRR gene polymorphisms in patients with chronic HBV infections.
Materials and methods
Subjects
The present study was approved by the Medical Ethics Committee of Zigong Third People’s Hospital (approval number: NO. 2020-Research Ethics-05). All patients in this study provided oral consent for the publication of their data. The enrolled subjects with chronic HBV infections were treated at the Outpatient Clinic of Zigong Third People’s Hospital or were admitted to Zigong Third People’s Hospital from January 2021 to June 2022. All of the patients were diagnosed with chronic HBV infections according to the following criteria: Guidelines for the Prevention and Treatment of Chronic Hepatitis B (2019 version) (Chinese Society of Infectious Diseases, Chinese Medical Association, Chinese Society of Hepatology, Chinese Medical Association 2019); and Standardisation of Diagnosis and Treatment of Primary Liver Cancer (2019 version) (Bureau of Medical Administration, National Health Commission of the People’s Republic of China, Citation2020). Subjects meeting any of the following criteria were excluded: (1) chronic HBV infection combined with a history of other cancers; (2) a history of infection with other hepatitis viruses or AIDS; (3) alcoholic cirrhosis (with a confirmed history of alcohol abuse) and suspected of drug-induced liver cirrhosis; and (4) incomplete data. Based on the above criteria, 191 subjects were included, then divided into three groups: (1) 71 subjects in the chronic hepatitis B (CHB) group, 47 males and 24 females with a mean age of 55.87 ± 16.16 years; (2) 56 subjects with HBV-induced liver cirrhosis (LC) group, 38 males and 18 females with a mean age of 59.57 ± 13.33 years; and (3) 64 subjects in the HBV-related primary liver cancer (PLC) group, 51 males and 13 females with a mean age of 60.42 ± 12.73 years.
Research methodology
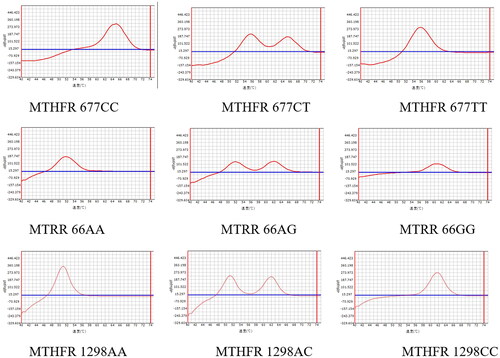
Two millilitres of peripheral venous blood were drawn from each subject into a purple anticoagulant tube. MTHFR C677T, MTHFR A1298C, and MTRR A66G polymorphisms were detected using the PCR-melt curve method, which is the combination of a real-time PCR platform, specific primers, fluorescence probes, and a melt curve. The procedures of PCR-melt curve method were as follows: (1) DNA was extracted from whole blood. The blood sample in the purple anticoagulation tube was properly mixed. Two hundred microlitres of the whole blood sample were used for DNA extraction according to the kit instructions. The blood sample was added to the sample hole of the extraction plate, the genome was extracted in the automatic extraction instrument, and the sample DNA was obtained after extraction. Nucleic acid was extracted according to the instructions of the extraction reagent. (2) Genotyping of polymorphisms in the MTHFR and MTRR genes was conducted according to the kit instructions. A PCR reaction system was prepared and PCR amplification, result interpretation, and quality control procedures were undertaken. The reagent was taken out of the refrigerator, balanced at room temperature for 30 min, mixed, and centrifuged for 20 s. Then, the PCR reaction amplification system was prepared according to the proportion of each component and packaged into a PCR reaction tube. The DNA extracted from 2-μL blood samples was added to the PCR reaction amplification system, the PCR reaction tube was covered, and the bubbles were removed by instantaneous centrifugation. Finally, the PCR reaction tube was placed on a fluorescence PCR analyser for PCR amplification. The PCR reaction parameters were as follows: 1 cycle at 95 °C for 2 minutes; and 50 cycles at 94 °C for 15 seconds, 56 °C for 30 seconds, and 72 °C for 10 seconds. The melting stage temperature was 45 °C→75 °C and the fluorescence was detected. Analysis and interpretation of results were performed after the operation (). All procedures were performed according to the kit instructions.
Instruments and reagents
The SLAN-96P real-time PCR system was purchased from Shanghai Hongshi Medical Treatment Technology Co., Ltd. (Shanghai, China). The biosafety cabinet was purchased from Biobase Biodustry (Shandong) Co., Ltd. (Shandong, China). The fully automatic nucleic acid extraction system was purchased from Shanghai BioGerm Medical Technology Co., Ltd. (Shanghai, China). The MTHFR (C677T), MTHFR (A1298C), and MTRR (A66G) Gene Detection kits (PCR-melt curve method) were purchased from Wuxi RiQiGen Biotech Co., Ltd. (Wuxi, China).
Statistical method
All data were analysed using SPSS 17.0 software. The included data are expressed as counts (percentages). Cross-tabulation and the chi-square test or Fisher’s exact test were used for the differences between sexes, age groups, and HBV types. The Hardy-Weinberg equilibrium test was used to confirm the samples were representative of the target population using the HW formula: theoretical frequency CC = total × C%2, CT = total × 2 C%*T%, TT = total × T%2.
Results
Hardy-Weinberg equilibrium analysis
The Hardy-Weinberg equilibrium test was carried out for the MTHFR C677T (χ2 = 0.592, p = 0.744), MTRR A66G (χ2 = 0.387, p = 0.824), and MTHFR A1298C (χ2 = 0.014, p = 0.993) polymorphisms among the enrolled patients with chronic HBV infections (). The entire population was in Hardy-Weinberg equilibrium, indicating that the samples were representative of the target population.
Table 1. Hardy-Weinberg equilibrium test for analysing MTHFR and MTRR gene polymorphisms in patients with chronic HBV infection from Zigong, n (%).
Distribution of MTHFR and MTRR genetic polymorphisms in patients with chronic HBV infections
The frequencies of the MTHFR C677T polymorphism CC, GT, and TT genotypes were 41.36% (79/191), 48.69% (93/191), and 9.95% (19/191), respectively. The frequencies of the C and T alleles were 65.71% and 34.29%, respectively. The frequencies of the MTRR A66G polymorphism AA, AG, and GG genotypes were 60.21% (115/191), 36.13% (69/191), and 3.66% (7/191), respectively. The frequencies of the A and G alleles were 78.27% and 21.73%, respectively. The frequencies of the MTHFR A1298C polymorphism AA, AG, and GG genotypes were 71.2% (136/191), 21.68% (50/191), and 2.62% (5/191), respectively. The frequencies of the A and C alleles for the MTHFR A1298C polymorphism were 84.29% and 15.71%, respectively ( and ).
Table 2. Analysis of genetic polymorphisms of MTHFR and MTRR in patients with chronic HBV infection from Zigong.
Analysis of MTHFR and MTRR genetic polymorphisms in patients with chronic HBV infections stratified by age and sex
The differences of genetic polymorphisms in the distributions of MTHFR C677T (χ2 = 1.625, p = 0.444), MTRR A66G (Fi = 0.557, p = 0.835), and MTHFR A1298C (Fi = 3.671, p = 0.155) between the patients ≤ 60 and > 60 years of age are shown in . In addition, the distributions of MTHFR C677T (χ2 = 0.770, p = 0.714), MTRR A66G (Fi = 2.249, p = 0.353), and MTHFR A1298C (Fi = 0.176, p = 1.000) genetic polymorphisms did not vary between male and female patients from Zigong ().
Table 3. Comparative analysis of genetic polymorphisms of MTHFR and MTRR in patients with chronic HBV infection stratified by age, n (%).
Table 4. Comparative analysis of genetic polymorphisms of MTHFR and MTRR in patients with chronic HBV infection stratified by gender, n (%).
Analysis of MTHFR and MTRR genetic polymorphisms in different groups of patients
The distributions of MTHFR and MTRR gene polymorphisms were compared between the CHB, LC, and PLC groups. The frequencies of MTHFR C677T genetic polymorphisms did not vary in the pairwise comparison between the three groups (CHB vs. LC, χ2 = 0.239, p = 0.888; CHB vs. PLC, χ2 = 0.882, p = 0.661; PLC vs. LC, χ2 = 0.326, p = 0.926; ). The frequencies of MTRR A66G genetic polymorphisms did not vary in the pairwise comparison between the three groups (CHB vs. LC, Fi = 0.331, p = 0.955; CHB vs. PLC, Fi = 1.114, p = 0.645; PLC vs. LC, Fi = 2.092, p = 0.355; ). The frequencies of MTHFR A1298C genetic polymorphisms did not vary in the pairwise comparison between the three groups (CHB vs. LC, Fi = 3.510, p = 0.12; CHB vs. PLC, Fi = 3.015, p = 0.263; PLC vs. LC, Fi = 1.412, p = 0.550; ).
Table 5. Comparative analysis of genetic polymorphisms of MTHFR and MTRR in different groups of patients [n(%)].
Discussion
MTHFR and MTRR are key enzymes in folate metabolism and are involved in DNA synthesis, repair, methylation, and the regulation of gene expression (Jiajin et al. Citation2019). The progression of HBV-related diseases after an infection is the combined result of host and viral factors. The liver is the key organ where folate is metabolised and homocysteine is cleared. Recent studies have shown that polymorphisms in the MTHFR and MTRR genes affect the disease course after HBV infection (Kwak et al. Citation2008; Jiao et al. Citation2017; Zhang et al. Citation2020). The MTHFR C677T polymorphism induces hyperhomocysteinemia, which may be the basis for vascular complications, such as liver fibrosis and liver cirrhosis (Zhang et al. Citation2020); however, the MTHFR C677T polymorphism has dual effects. Specifically, carriers of the T allele may have a higher risk of cancers in light of the role of the MTHFR C677T polymorphism in DNA methylation, but when the positive role of MTHFR C677T polymorphism in DNA synthesis is considered, the T allele is a protective factor against cancers (Kwak et al. Citation2008; Jiao et al. Citation2017). Our study compared the MTHFR and MTRR gene polymorphism distributions across three groups of HBV infections (CHB, LC, and PLC groups) and demonstrated few differences in the MTHFR C677T, MTHFR A1298C, and MTRR A66G polymorphism distributions (p > 0.05). The above results suggest that polymorphisms in the MTHFR and MTRR genes might not be risk factors for the progression of HBV-related diseases.
In one study, the MTHFR C677T polymorphism was more strongly correlated with DNA methylation in females than males (Qiao et al. Citation2020). According to another study, the TT genotype and T allele had a stronger protective effect against HCC and liver cirrhosis in males (Jiao et al. Citation2017). Based on data stratified by age and aetiology, the MTHFR 1298A > C and MTRR 66AG + GG genotypes were risk factors for disease onset following HBV infection in the group > 65 years of age (Kwak et al. Citation2008). Our results indicated that, in the study population with HBV infections from Zigong, the frequencies of MTHFR C677T, MTHFR A1298C, and MTRR A66G genetic polymorphisms did not vary with age and sex. Conflicting conclusions drawn from various studies point to the need for further investigation into the correlation between MTHFR and MTRR gene polymorphisms as a function of age and sex in HBV-infected patients.
Important heterogeneity has been reported in the genotype and allele frequencies of MTHFR and MTRR gene polymorphisms across geographic regions and ethnic groups (Yang et al. Citation2013; Jiao et al. Citation2017). Supplemental Tables 1–3 showed that the CC, CT, and TT genotype frequencies of the MTHFR C677T polymorphism in the population with chronic HBV infections from Zigong were 41.36% (79/191), 48.69% (93/191), and 9.95% (19/191), respectively. The C and T allele frequencies were 65.71% and 34.29%, respectively. When compared to the corresponding subjects from Luzhou, Suining, Deyang, and northeast Sichuan (Zhang et al. Citation2012; Fang et al. Citation2018; Xiang et al. Citation2019; Chen et al. Citation2020), the differences were obvious. The above results suggest that the MTHFR C677T polymorphism distribution characteristics were basically consistent across different parts of Sichuan. We found that the MTHFR C677T genotype and allele distributions in the study population from Zigong were different from Beijing and Gansu (Li et al. Citation2019; Bao et al. Citation2021). We concluded, therefore, that the further the geographic distance, the greater the differences. The differences also existed between Zigong and northern India with respect to the distribution of MTHFR C677T genotypes (Fang et al. Citation2018). The above results indicated that there were geographic differences in the distribution of MTHFR C677T genotypes between Zigong and northern India; however, such geographic differences were not observed between Zigong and countries other than northern India (Omsk, Russia, Macedonia, Australia, Poland, and Tunisia [Markan et al. Citation2007; Spiroski et al. Citation2008; Reeves et al. Citation2009; Vilms et al. Citation2023]). The frequencies of the AA, AG, and GG genotypes of the MTRR A66G polymorphism were 60.21% (115/191), 36.13% (69/191), and 3.66% (7/191), respectively. The frequencies of the A and G alleles were 78.27% and 21.73%, respectively. The genotype and allele frequencies of the MTRR A66G polymorphisms were quite different in the study population from Zigong compared to Deyang and Sichuan (Zhang et al. Citation2012) and Gansu (Bao et al. Citation2021). Differences in the genotype distribution of the MTRR A66G polymorphism existed between the study population from Zigong and Omsk and Russia (Vilms et al. Citation2023), and Tunisia (Nasri et al. Citation2019). As seen above, the genotype and allele distributions of the MTRR A66G polymorphism varied across geographic regions, but such geographic differences might also be related to population differences. Several confounding factors might be involved in the explanation of the above differences, including intrinsic features of the study population and sample size. Further investigations are needed to clarify this finding. In a previous study the prevalence of MTHFR C677T and A1298C, and MTRR A66G showed geographic variations among Chinese Han populations, which are consistent with our study findings. The geographic variations among different countries also warrant further study.
The present study had several limitations we would like to acknowledge. First, the study scope was limited to the HBV-infected population in Zigong and the sample size was quite small, which might introduce geographic bias and affect the generalisability of the findings. Second, the study did not delve into the potential influence of various factors, such as age, sex, and lifestyles on the observed polymorphisms in the MTHFR and MTRR genes within the HBV-infected population. The comorbidities and medications of this population were not analysed. The uninfected controls from the same population were not analysed either. Further research involving a more diverse population and considering broader variables is necessary to enhance the comprehensiveness and applicability of the findings.
Conclusion
The distributions of MTHFR and MRRR genetic polymorphisms in the population with HBV infections in Zigong, Sichuan Province did not differ in age and sex.
Ethics approval and consent to participate
The present study was approved by the Medical Ethics Committee of Zigong Third People’s Hospital [approval number: NO. 2020-Research Ethics-05]. All patients in this study provided oral consent for the publication of their data.
Authors’ contributions
Shunhua Qiu: guarantor of integrity of the entire study; study concepts; study design; definition of intellectual content; clinical studies; manuscript preparation. Lifen Jin: definition of intellectual content; literature research; clinical studies; manuscript preparation. Dan Yan: literature research; clinical studies; manuscript preparation. Dewen Zhang: guarantor of integrity of the entire study; data analysis; manuscript editing; manuscript review. All authors read and approved the final manuscript.
Supplemental Material
Download PDF (287.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Bao L, Shen D, Yang Y, Zhang H, Guo X. 2021. Study on gene polymorphism of folate metabolism related enzymes MTHFR and MTRR in Gansu. Lab Med Clinic. 18:1–7.
- Bureau of Medical Administration, National Health Commission of the People’s Republic of China. 2020. Standard of diagnosis and treatment of primary liver cancer (2019 edition). J Clin Hepatology. 36 (2):277–292.
- Chen Y, Ren X, Li Y, Li H. 2020. Study on the distribution of MTHFR gene polymorphism among Han population in Luzhou and the correlation between MTHFR gene polymorphism and recurrent spontaneous abortion in women of childbearing age. Matern Child Health Care China. 5:87–90.
- Chinese Society of Infectious Diseases, Chinese Medical Association, Chinese Society of Hepatology, Chinese Medical Association. 2019. [The guidelines of prevention and treatment for chronic hepatitis B (2019 version)]. Zhonghua Gan Zang Bing Za Zhi. 27:938–961. doi: 10.3760/cma.j.issn.1007-3418.2019.12.007.
- Fang L, Mu C, Zhang L, Xu Y, Zhao W, Chen Y. 2018. Study on distributions of MTHFR C677T gene polymorphism in pregnant women from northeast of Sichuan. Genomics Appl Biol. 37:1820–1824.
- Jiajin L, Shuyan C, Ying W, Junxiao C, Xiudi W. 2019. Genetic polymorphisms in folate metabolism as risk for Down syndrome in the southern China. J Matern Fetal Neonatal Med. 32(12):2030–2035. doi: 10.1080/14767058.2018.1424818.
- Jiao X, Luo Y, Yang B, Jing L, Li Y, Liu C, Jing X, Wang F, Wang Y, Du Z, et al. 2017. The MTHFR C677T mutation is not a risk factor recognized for HBV-related HCC in a population with a high prevalence of this genetic marker. Infect Genet Evol. 49:66–72. doi: 10.1016/j.meegid.2017.01.008.
- Kwak SY, Kim UK, Cho HJ, Lee HK, Kim HJ, Kim NK, Hwang SG. 2008. Methylenetetrahydrofolate reductase (MTHFR) and methionine synthase reductase (MTRR) gene polymorphisms as risk factors for hepatocellular carcinoma in a Korean population. Anticancer Res. 28:2807–2811.
- Li D, Ye A, Gan Y, Li P, Wu J, Qiu L. 2019. Analysis for polymorphism of MTHFR C677T gene in Han population in Beijing. Linchuang Jian Yan Za Zhi. 2:156–160.
- Lu D, Zhuo J, Yang M, Wang C, Pan L, Xie H, Xu X, Zheng S. 2018. The association between donor genetic variations in one-carbon metabolism pathway genes and hepatitis B recurrence after liver transplantation. Gene. 663:121–125. doi: 10.1016/j.gene.2018.03.071.
- Markan S, Sachdeva M, Sehrawat BS, Kumari S, Jain S, Khullar M. 2007. MTHFR 677 CT/MTHFR 1298 CC genotypes are associated with increased risk of hypertension in Indians. Mol Cell Biochem. 302(1-2):125–131. doi: 10.1007/s11010-007-9434-5.
- Nasri K, Midani F, Kallel A, Ben Jemaa N, Aloui M, Boulares M, Lassoued M, Ben Halima M, Ben Wafi S, Soussi M, et al. 2019. Association of MTHFR C677T, MTHFR A1298C, and MTRR A66G polymorphisms with neural tube defects in Tunisian parents. Pathobiology. 86(4):190–200. doi: 10.1159/000499498.
- Qiao K, Zhang S, Huo Z, Hou W, Dai Q, Su R, Wang F. 2020. LINE-1 methylation in chronic HBV infected patients: association with HCC, gender and MTHFR C677T polymorphism. Clin Lab. 66(5):1–6. doi: 10.7754/Clin.Lab.2019.190906.
- Qiao K, Zhang S, Trieu C, Dai Q, Huo Z, Du Y, Lu W, Hou W. 2017. Genetic polymorphism of MTHFR C677T influences susceptibility to HBV-related hepatocellular carcinoma in a Chinese population: a case-control study. Clin Lab. 63(4):787–795. doi: 10.7754/Clin.Lab.2016.161003.
- Reeves SG, Meldrum C, Groombridge C, Spigelman AD, Suchy J, Kurzawski G, Lubinski J, McElduff P, Scott RJ. 2009. MTHFR 677 C > T and 1298 A > C polymorphisms and the age of onset of colorectal cancer in hereditary nonpolyposis colorectal cancer. Eur J Hum Genet. 17(5):629–635. doi: 10.1038/ejhg.2008.239.
- Spiroski I, Kedev S, Antov S, Arsov T, Krstevska M, Dzhekova-Stojkova S, Kostovska S, Trajkov D, Petlichkovski A, Strezova A, et al. 2008. Association of methylenetetrahydrofolate reductase (MTHFR-677 and MTHFR-1298) genetic polymorphisms with occlusive artery disease and deep venous thrombosis in Macedonians. Croat Med J. 49(1):39–49. doi: 10.3325/cmj.2008.1.39.
- Vilms EA, Turchaninov DV, Antonova IV, Kozubenko OV. 2023. [Assessment of the role of nutritional and genetic determinants in the formation of the risk of diseases associated with folate cycle disorders in the population of the Omsk region]. Vopr Pitan. 92(2):35–42. doi: 10.33029/0042-8833-2023-92-2-35-42.
- Xiang Y, Zhao Q, Liu YL, Liu YJ, Lv J. 2019. Polymorphism of methylenetetrahydrofolate reductase gene in women of childbearing age in Suining region. J Mod Med Health. 35:2108–2112.
- Xu W, Yu J, Wong VW. 2017. Mechanism and prediction of HCC development in HBV infection. Best Pract Res Clin Gastroenterol. 31(3):291–298. doi: 10.1016/j.bpg.2017.04.011.
- Yang B, Liu Y, Li Y, Fan S, Zhi X, Lu X, Wang D, Zheng Q, Wang Y, Wang Y, et al. 2013. Geographical distribution of MTHFR C677T, A1298C and MTRR A66G gene polymorphisms in China: findings from 15357 adults of Han nationality. PLoS One. 8(3):e57917. doi: 10.1371/journal.pone.0057917.
- Zappacosta B, Graziano M, Persichilli S, Di Castelnuovo A, Mastroiacovo P, Iacoviello L. 2014. 5,10-Methylenetetrahydrofolate reductase (MTHFR) C677T and A1298C polymorphisms: genotype frequency and association with homocysteine and folate levels in middle-southern Italian adults. Cell Biochem Funct. 32(1):1–4. doi: 10.1002/cbf.3019.
- Zhang S, Jiang J, Tang W, Liu L. 2020. Methylenetetrahydrofolate reductase C677T (Ala > Val, rs1801133 C > T) polymorphism decreases the susceptibility of hepatocellular carcinoma: a meta-analysis involving 12,628 subjects. Biosci Rep. 40(2):1–12. doi: 10.1042/bsr20194229.
- Zhang Y, Zhu Z, Wang W. 2012. Polymorphism of MTHFR and MTRR among Han women in Deyang, Sichuan. Chin J Evid-Based Med. 12:631–634.