Abstract
Background
The charity foundation Association Soutien Enfants Togo started a child health care (CHC) centre in Togo that was modelled after the Dutch high-quality CHC system to improve child health.
Aim
To describe health care data of children who visited the centre.
Subjects and methods
Data were routinely collected between October 2010-July 2017. Outcomes were completed vaccinations, growth, development, lifestyle, physical examination, and laboratory testing results.
Results
In total, 8,809 children aged 0–24 years were available. Half (47.5%) of children aged 0–4 years did not receive all eligible free vaccinations from the government. The proportions of stunted children (all) or with a developmental delay (0–4 years) were 10.1% and 9.5%, respectively. In total, 40–50% of all children did not wash their hands with soap after toilet or before eating, or did not use clean drinking water. Furthermore, 5.1–6.6% had insufficient vision, high eye pressure or hearing loss. Sickle cell disease was detected in 5.3%.
Conclusion
A large group of children in need of prevention and early treatment were detected, informed and treated by the centre. Further research is needed to confirm if this strategy can improve children’s health in Sub-Saharan Africa. Our data are available for further research.
Introduction
Togo is a low-income country in Sub-Saharan Africa. In 2021, the neonatal mortality rate and the under-five mortality rates were high, respectively 24 and 63 per 1,000 live births (IGME Citation2023). Reasons that contribute to these high mortality rates are related to the household and the health care system. The number of households with a low maternal educational level and/or a low income is high (The World Bank Citation2023). A low education can result in a low level of knowledge and skills to effectively understand and utilise available information and resources critical for child health (Ettarh and Kimani Citation2012). A low income can lead to malnutrition and dietary deficiencies (FAO Citation2019), no adequate sanitation facilities, poor quality of drinking water (Dossè Mawussi DJAHINI-AFAWOUBO Citation2017), financial constraints to pay a doctor, and a longer distance to the nearest health facility (Dossè Mawussi DJAHINI-AFAWOUBO Citation2017). The Togolese health care system is fragile. There is no affordable health insurance for non-public servants or a social health insurance but with limited coverage for public servants. There are also restricted government expenditures for the prevention of diseases and health problems, insufficient staff and medical supplies (Petersdorf Citation2023), and suboptimal clinical knowledge of the staff (Di Giorgio et al. Citation2020). In addition, there is limited access to the services of Child Health Care (CHC) (Sanoussi Citation2017).
The most cost-effective health intervention to reduce child mortality in Togo is to prevent diseases by vaccinations (Unicef Citation2023). However, most recent data on completeness of vaccinations in Togo showed that 46% of children aged 0–11 months (in 2013) and 28% of children aged 12–23 months (in 2017) were not fully immunised (TOGO Citation2014; Ekouevi et al. Citation2018). The health region Plateaux showed the highest rate of incomplete immunisation (58%) (Ekouevi et al. Citation2018). Besides increasing the coverage rate of complete immunisation, early childhood preventative and curative services that provide households with information to prevent, detect and treat infectious diseases (e.g. pneumonia, diarrhoea and malaria) may also contribute to a decrease in child mortality (UN Citation2023).
Literature reports that the implementation of strategies to better organise preventive measures in primary care is relevant to low- and middle-income countries (Althabe et al. Citation2008; Fiori et al. Citation2021). A promising strategy may be to provide a preventive service in Togo that is modelled after CHC in the Netherlands. Dutch children are among the happiest and healthiest in the world, which is confirmed in the Health Behaviour in School-aged Children survey and the UNICEF report on well-being of children in rich countries, in which the Netherlands scored highest (HBSC Citation2020; UNICEF Innocenti Citation2020). The early stages of children’s lives are not only important for their well-being at that moment, but are also crucial for their further development, health and well-being throughout life (Jacob et al. Citation2017). We assume that the preventive service for Dutch CHC has contributed to the high score for well-being in children mentioned in the UNICEF report.
The Dutch CHC is a high-quality system based on a unique standardised preventive child health care program (Siderius et al. Citation2016). The Dutch CHC is offered to all children from birth until the age of 18 years. Children are followed-up at around 15 regularly scheduled visits during which children are assessed by CHC-professionals, including doctors, nurses, and supporting assistants. This service includes monitoring overall health, growth and development using the Dutch Development Instrument (DDI, in Dutch: Van Wiechenonderzoek) (Laurent de Angulo et al. Citation2005), speech, hearing, sight and movement, nutrition, upbringing and the home situation, and offers vaccinations for infectious diseases. During these visits parents can ask questions or share their concerns, e.g. about (breast) feeding, hygiene, care, sleep patterns and crying, colic, toilet training, temper, child behaviour and parenthood. The CHC-professional provides (preventive) information, advice, guidance or instruction and assesses whether additional support, help or care is needed, and can refer to specialist care.
In order to improve child health in Togo, the charity foundation Association Soutien Enfants Togo (Stichting Kinderhulp Togo in Dutch) started a CHC centre in Kpalimé in 2010. Kpalimé is a city in the Plateaux Region of Togo, 15 km from the border with Ghana. Kpalimé has a population of nearly 100,000, making it the fourth-biggest city in Togo. The CHC centre in Kpalimé was modelled after CHC in The Netherlands, but adapted to better align with differences in lifestyle, socio-economic factors, (mal)nutrition, hygiene, blood relationships, diseases and pathologies between the Dutch and Togolese population.
To be able to monitor the health status of children who visited the CHC centre in Kpalimé, health care data were collected between October 2010 and July 2017 and included in the Child HEalth Care in Kpalimé TOGO (CHECK2GO) study.
The aim of the program of the CHC centre was to improve child health in Togo using the criteria of the World Health Organisation (WHO) for preventive health policy: prevention, early identification of diseases, and early treatment and care of diseases to prevent disability (Présentation générale Citation2023). The objective of this study was to describe a selection of health care data of children who visited the CHC centre.
Materials and methods
Child health care centre in Kpalimé
The CHC centre in Kpalimé was founded by one of the authors, a CHC medical doctor and chief medical officer of Association Soutien Enfants Togo. To model the CHC centre in Kpalimé after the Dutch CHC, the standardised preventive child health care program in the Netherlands was used as the basis.
Patient and public involvement
The project and program of the CHC centre are unique in Togo, because there is no systematic research on children’s health in this country. To ensure that the CHC centre in Kpalimé was properly aligned with the care that children need in Togo, one of the authors visited a number of medical hospitals and facilities in different parts of Togo. We received input on cultural differences, health issues in Togo, and financial constraints, and conducted a pilot among children attending primary school. The program of the CHC centre was then adapted to better meet the needs of the Togolese children (e.g. examination of intraocular pressure, determination of blood group and anaemia). The program of the CHC centre was presented and approved before implementation by the Director General of the Ministry of Health in Togo (Dr. Dogbe at the time). After implementation, annual data were presented to the government of Togo in a detailed report. In addition, the Togo health authorities regularly visited and checked the CHC centre. The Ministry of Health supported this project, because it could serve as an example for future health policy. In accordance with the Dutch approach, the centre functions as primary health care. In case of medical issues, the child is referred to secondary health care, usually a hospital. This is in accordance with the Dutch situation and the WHO criteria (Présentation générale Citation2023).
A medical centre, a laboratory for blood and stool testing, and a small pharmacy were established in the CHC centre. A physiotherapist and an audiology centre were available at a different location, but this was under the sole responsibility of the CHC. The staff of the CHC centre consisted of a doctor, health care staff (“Techniciens Supérieurs de Santé”), assistants, a physiotherapist, speech therapists (two of them were trained abroad to measure hearing aids), health and laboratory technicians, an administrator, cleaner (to ensure good hygiene), and guards. In addition to the activities that are also carried out by the Dutch CHC, extra attention was paid towards prevention; a check whether free vaccinations from the Programme Elargi de Vaccinations of the government have been carried out completely was part of the regular investigations. In close cooperation with the Togolese health authorities, it has been jointly determined that if a child was not completely vaccinated, the CHC centre referred the child/parent to a government vaccination location. The following vaccinations were offered by the CHC centre: meningococcal AWCY, typhoid fever vaccine and pneumococcal polysaccharide vaccine (PPSV23) in children with severe sickle cell disease were offered every three years, as this is not part of the government’s vaccination program. Also, information on healthy living, good nutrition, hygiene and disease prevention, and several educational prevention programmes at the centre and the local primary and secondary schools were provided. Furthermore, laboratory testing for blood (e.g. sickle cell disease, blood type, malaria, anaemia) and stool was performed. The pharmacy could ensure that children follow the advice that follows from the screening and tests at the CHC centre, and offered affordable methods of treatment, and basic medicines. Hearing aids were provided at a lower price, and glasses were provided at no charge after full examination and approval by the CHC staff. The first examination in the hospital was paid for by the CHC centre. For children in the poorest families, a financial contribution was arranged for further follow-up treatment in hospitals.
Organisation of the health screening visits
During the health screening visits at the CHC centre in Kpalimé, CHC-professionals assessed background, perinatal (0–4 years), and neonatal (0–2 years) characteristics, completeness of vaccinations, a child’s health, growth, i.e. weight, length/height, and head circumference (0–1 years), and child development using the DDI that includes 75 age-specific milestones (gross and fine motor skills, adaptive/personal/social behaviour, communication) (0–4 years). Moreover, a physical examination (e.g. vision (≥3 years, with Landolt-C ≥ 5 years), eye pressure (≥10 years), hearing (≥5 years)), and laboratory testing (≥6 months blood tests; a check for malaria using a small finger prick <6 months) were assessed. Lifestyle (to promote healthy choices), medical complaints (≥10 years) and well-being (≥10 years) were discussed verbally with the parents (<10 years) or by means of a questionnaire completed by the child (≥10 years). To support parents daily care, parenting, and child behaviour were discussed. Hearing for babies was tested using the Ewing test, instead of neonatal hearing screening, due to financial constraints and technical problems (e.g. electricity failure) (Ewing and Ewing Citation1944).
Accessibility
Schools and parents in Kpalimé and surroundings were approached to provide children’s parents with information about Kpalimé’s CHC centre and its services. In total, 77 primary and secondary schools with approximately 25,000 children were included between October 2010 and July 2017. The target group consisted of children aged 1 month to 18 years and young adults aged 18 and over who were still in secondary school. Children and their parents could attend the CHC centre and all follow-ups on a voluntary basis after paying a small fee of 500–2500 FCFA (∼1-4 EUR). The amount depended on the age of the child, because of the age-dependent activities that were provided. Young adults attending secondary school could also attend the CHC centre in Kpalimé without explicit consent of the parents. This advanced age is due to the fact that some children are sent to school at a later age or because, due to various circumstances, they do not receive timely education in accordance with national guidelines. In case of additional treatment at the centre, 80% of the medication was reimbursed by the foundation, if necessary, for parents with limited budget. If parents visited the CHC centre with two children, the treatment of the second child at the centre was free. When referred to a hospital or a private clinic (ophthalmologist, Ear, Nose and Throat specialist, paediatrician, surgeon, stomatology, etc.), the costs of the first consultation were paid by the foundation in order to encourage the parents that children should undergo further treatment. For treatment in hospital or private clinic, 80% was reimbursed by the foundation (special fund) for parents with limited budget. Vaccinations, aside from those provided by the Togolese government, were offered at the CHC centre for a small fee.
Long-term follow-up
In addition to direct care, the CHC centre also offered long-term follow-up of any medical complaints. For example, for children with high eye pressure (more prevalent in Togo), 80% of the costs were reimbursed on a long-term basis. In case of ear problems, the examinations were repeated. For children with permanent hearing loss, the CHC centre supplied hearing aids and speech therapy.
All children who visited the CHC centre in Kpalimé between October 2010 until July 2017 were included in the CHECK2GO prospective study. Health care data from each visit were recorded in paper health records and digitised between May and December 2017 by three local data-assistants using the EpiData software (Lauritsen Citation1999). These data were subsequently checked and rechecked and analysed using R version 4.0.3 (R Core Team. R Core Team Citation2020).
Outcomes
In this study, we present a selection of data from each domain available in the CHECK2GO study. These domains were completed vaccinations, growth and development, lifestyle, physical examination, and laboratory testing. More specifically, the primary outcomes were the proportion of children with incomplete vaccinations, growth delay, developmental delay, unhealthy lifestyle, insufficient vision, high eye pressure, hearing loss, and sickle cell disease. Secondary outcomes were perinatal and neonatal characteristics of the children and how often they visited the centre. A codebook was developed to document all variables, and their definitions, and make the data interoperable (See Supplementary file 1).
Statistical analyses
Descriptive statistics were performed on background, perinatal and neonatal characteristics, and this was further stratified by age group (0–4, 5–13, 14–24 years) for each domain (completed vaccinations, growth and development, lifestyle, physical examination, and laboratory testing). The reason for choosing these age groups is that this corresponds to the regular visits and activities of the Dutch child health care system.
A developmental score (D-score) was calculated for each child at each visit from an algorithm that summarises the developmental milestones of the DDI into a single aggregated score measuring global development. It is a validated, unified indicator for early life development (Weber et al. Citation2019). Age-conditional references of the D-score (Weber et al. Citation2019) were used to calculate the D-score-for-age z-scores (DAZ). A developmental delay was defined as DAZ <-2 SD. Length or height-for-age z-scores (HAZ), weight-for-age z-scores (WAZ) and head circumference-for-age z-scores (HCZ) were calculated using WHO standards or references (WHO Multicentre Growth Reference Study Group Citation2006; de Onis et al. Citation2007; WHO Multicentre Growth Reference Study Group. Citation2007). Stunted was defined as HAZ < −2 SD, underweight as WAZ < −4 SD, and a low head circumference as HCZ < −2 SD.
Results
presents descriptive statistics on the background, neonatal (first months of life) and perinatal (at birth) characteristics of the children and their parents/caretaker. In total, 8,809 children visited this CHC centre at least once between October 2010 and July 2017. From these children, 4,444 (49.5%) made a one-time visit, and 4,365 (50.5%) visited the centre several times. The majority (87%) of the children who visited the CHC centre lived within a radius of 1 kilometre.
Table 1. Background, perinatal and neonatal characteristics of the children and their parents/caretaker.
presents the descriptive statistics of the children in the CHECK2GO study by first visit within each age group in the following domains: completed vaccinations, growth and development, lifestyle, physical examination, and laboratory testing.
Table 2. ResultsTable Footnote* of the children and their parents/caretaker stratified by age of the child.
shows that the number of children with unknown values differ per domain and parameter. These unknown values apply to activities that are not offered at that visit given the age of the child, or the activity has been performed but not recorded. When considering these unknown values, development, growth, and blood film were most often examined in the youngest age group (0–4 years). In the older age groups, the data show that most attention was paid to the visual acuity screening (5–13 years) and hearing screening (5–24 years). When excluding unknown values, we found that almost half (47.5%) of children aged 0–4 years did not receive all eligible free vaccinations that were offered by the Programme Elargi de Vaccinations. This was higher in the other age groups (>88%).
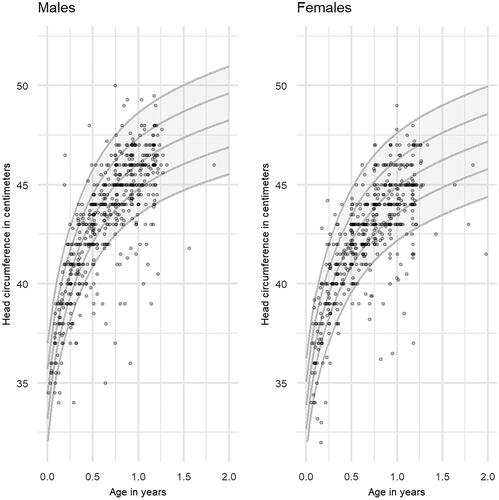
, and show the distribution of respectively height, weight and head circumference by age in males and females. The reference lines of −2, −1, 0, 1 and 2 standard deviations (SD) are shown. The proportion of children who were stunted, underweight, had a low head circumference or had a developmental delay were 10.1%, 1.4%, 12.1% and 9.5%, respectively, at their first visit (see ).
Figure 1. Distribution of height by age (in years) in males and females in the CHECK2GO study (n = 6,116).
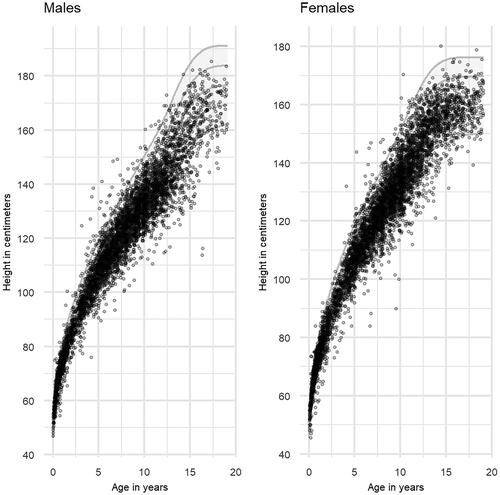
Figure 2. Distribution of weight by age (in years) in males and females in the CHECK2GO study (n = 6,112).
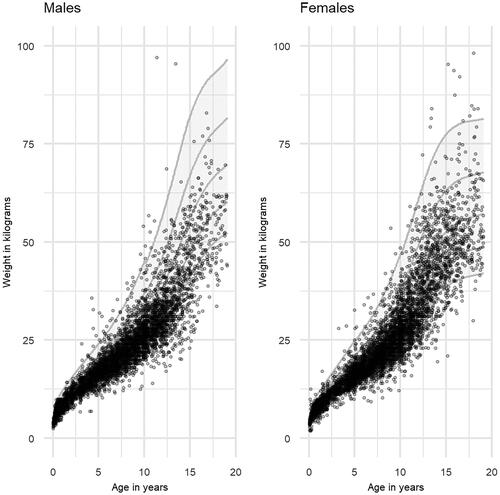
Figure 3. Distribution of head circumference by age (in years) in males and females in the CHECK2GO study (n = 478).
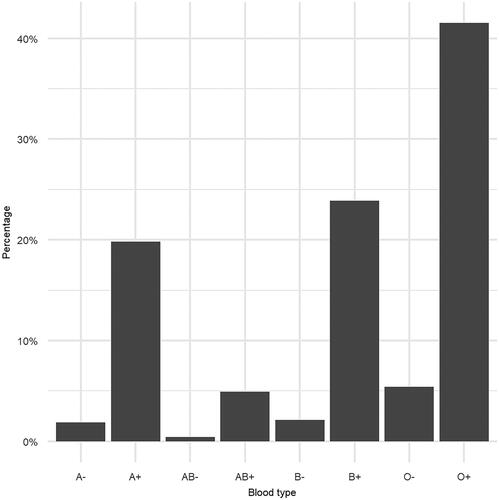
Furthermore, at their first visit, approximately 40 to 50% of children mentioned that they did not wash their hands with soap after toilet or before eating or did not use clean drinking water. Also, 27% of children aged 0–4 years slept less than 10 h, and 8% of children aged 5–13 years slept less than 8 h in the night. Furthermore, 5.1% had an insufficient result on the first vision screening (Landolt C), 5.9% had hearing loss (Fletcher Index), and 6.6% had eye pressure > 15 mm Hg. Blood count was measured in 56.1% of children, and this was 50.5% for blood film. shows the probability distribution of blood type; most children had blood type O+, B + or A+. Sickle cell disease was detected in 313 new cases out of 5,869 (5.3%) children (161 (2.7%) with type haemoglobin SS, 141 (2.4%) with type SC, and 11 (0.2%) with type SF).
Discussion
Professionals at the CHC centre in Kpalimé detected a large group of children who were in need of prevention and early treatment of diseases. Nearly half of the children did not receive complete vaccinations that were offered by the government, which is in agreement with the results of a vaccination study among children in the health region Plateaux in Togo (Ekouevi et al. Citation2018). This gave the opportunity to discuss the importance of vaccinations at the CHC centre and to refer the child/parent to a vaccination location. The data also shows that a large group of children had a developmental delay, stunting, and/or severe underweight. It is known that malnourished children, particularly those suffering from severe acute malnutrition, are at a higher mortality risk from common childhood illnesses (UN Citation2023). Furthermore, almost half of the children reported that they didn’t wash their hands with soap after toilet or before eating. Some children may not have learnt when and how they should wash their hands to stay healthy, or there were not the right facilities.
Moreover, 40% of the children reported that they did not use clean drinking water. Most children may not have had access to clean drinking water. Literature reported that Togo has a low coverage in access to basic services of drinking water (62%) and sanitation (12%) (Swe et al. Citation2021). Another concern is the potential lack of sleep in 8–27% of the youngest age groups, which may weaken their immunity, increasing organism susceptibility to infection (Ibarra-Coronado et al. Citation2015). Discussing the child’s sleep behaviour with the parents may help the parents to resolve sleep-related issues. Further improvements can also be established in the areas of vision and hearing. Vision and hearing are not systematically monitored in Africa and there is no prevention policy. As a result, children with loss in vision or hearing may experience difficulties in finding a good education and work. Moreover, sickle cell disease was detected in one in 20 children who visited the CHC centre. It is, therefore, recommended to perform systematic screening at an early age (from 6 months of age) to detect sickle cell disease so that any treatment can be started early, and additional vaccinations can be provided.
Strengths and limitations
Strengths are that the data collected by the CHC centre contain information on a wide range of parameters in several domains (completed vaccinations, growth and development, lifestyle, physical examination, and laboratory testing), which may provide a valuable insight into CHC needs in Togo and other countries within Sub-Saharan Africa. A small fee was asked to visit the CHC centre and financial support was provided for parents with limited budget or with a child’s referral to a hospital or private clinic. The criteria to identify the poorest for additional financial support for hospital visits were (1) the occupation of the parents (often the poorest parents have no occupation), (2) polygamy (as a proxy of poverty) and (3) the number of children. The fee for the service was set on the advice of the municipal authorities in Kpalimé. They advised not to offer free examinations and treatment to ensure that people regard the CHC as a serious service. This relates to the dignity of the parents who felt that they were contributing in this way. Even the poorest parents appeared to be able to pay the fee. Subsequent inquiries in the impoverished neighbourhoods revealed that the project was particularly well-received there, despite the small fee. A limitation is that it primarily includes routinely collected health care data, with only observational data and no control group. Another limitation is that the data were not examined longitudinally, which may give a better insight into the effect of the strategy. Further research is therefore recommended. Data for this research are available from the authors for further research. Also, it is unclear if all parents, adolescents or young adults (attending secondary school) fully understood the concept of prevention, however, we assume that especially those who visited the CHC centre several times (∼50%) understood this concept.
Lessons for other settings
Our programs, teaching materials, protocols, epidemiological data and other statistics are documented so that they are useful and accessible to others who want to conduct data research or establish preventive child health care in Sub-Saharan Africa. Interested parties (including researchers, government, healthcare professionals) can contact one of the authors, so that the knowledge that has been built up within this project can be shared and used to improve the health of children in Sub-Saharan Africa. In addition, the program can serve as an example for raising awareness of health problems, intensifying public scrutiny, improving access to and availability of services and making structural changes.
Conclusions
The CHC centre in Kpalimé is likely to make an important contribution to prevention and early treatment of infectious diseases. Data of the study show that the health of the children in Sub-Saharan Africa may be substantially improved if the children are periodically screened. Substantially intensifying the government’s prevention policy for children 0–4 years and extending policy to children aged 5–18 years may achieve major health gains in Sub-Saharan African countries.
Supplemental Material
Download PDF (434.9 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
We presented a selection of data from each domain. More data is available (See Supplementary file 1) for further research. Interesting future analysis on the CHECK2GO are (1) to compare the data with regional and national health statistics, which may provide indirect evidence for the effectiveness of the CHC centre in Kpalimé, (2) to assess the relationships between adverse early life events and development, health and well-being later in life, and (3) to develop a toolkit for countries for a comprehensive prevention policy for children between 0 and 18 years.
Data from the CHECK2GO study will adhere to the FAIR (http://datafairport.org/: Findable, Accessible, Interoperable and Reusable) concepts. Within this legal framework, Association Soutien Enfants Togo (Stichting Kinderhulp Togo) can thus decide how and under which conditions the data can be shared. Researchers can apply for data sharing by submitting a proposal to Association Soutien Enfants Togo (Stichting Kinderhulp Togo) (https://www.kinderhulp-togo.nl/). Requests should include a study protocol and institutional review board approval. Furthermore, a data-use agreement is required.
Additional information
Funding
References
- Althabe F, Bergel E, Cafferata ML, Gibbons L, Ciapponi A, Alemán A, Colantonio L, Palacios AR. 2008. Strategies for improving the quality of health care in maternal and child health in low- and middle-income countries: an overview of systematic reviews. Paediatr Perinat Epidemiol. 22(Suppl 1):1–10. doi:10.1111/j.1365-3016.2007.00912.x.
- de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. 2007. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 85(9):660–667. doi:10.2471/blt.07.043497.
- Di Giorgio L, Evans DK, Lindelow M, Nguyen SN, Svensson J, Wane W, Welander Tärneberg A. 2020. Analysis of clinical knowledge, absenteeism and availability of resources for maternal and child health: a cross-sectional quality of care study in 10 African countries. BMJ Glob Health. 5(12):e003377. doi:10.1136/bmjgh-2020-003377.
- Dossè Mawussi DJAHINI-AFAWOUBO. 2017. Working Paper 267 – Does Access to Basic Services Matter for Child Health? Evidence From Togo, Working Paper Series 2384, African Development Bank.
- Ekouevi DK, Gbeasor-Komlanvi FA, Yaya I, Zida-Compaore WI, Boko A, Sewu E, Lacle A, Ndibu N, Toke Y, Landoh DE, et al. 2018. Incomplete immunization among children aged 12–23 months in Togo: a multilevel analysis of individual and contextual factors. BMC Public Health. 18(1):952. doi:10.1186/s12889-018-5881-z.
- Ettarh RR, Kimani J. 2012. Determinants of under-five mortality in rural and urban Kenya. Rural Remote Health. 12:1812.
- Ewing IR, Ewing AWG. 1944. The ascertainment of deafness in infancy and early childhood. J Laryngol Otol. 59(9):309–333. doi:10.1017/S0022215100007465.
- FAO. 2019. FAOSTAT. Food and Agriculture Organization of the United Nations. Rome, Italy: FAO.
- Fiori KP, Lauria ME, Singer AW, Jones HE, Belli HM, Aylward PT, Agoro S, Gbeleou S, Sowu E, Grunitzky-Bekele M, et al. 2021. An integrated primary care initiative for child health in Northern Togo. Pediatrics. 148(3):e2020035493. doi:10.1542/peds.2020-035493.
- HBSC. 2020. Health Behaviour in School-Aged Children. World Health Organization collaborative cross-national study [website]. Glasgow: university of Glasgow;
- Ibarra-Coronado EG, Pantaleón-Martínez AM, Velazquéz-Moctezuma J, Prospéro-García O, Méndez-Díaz M, Pérez-Tapia M, Pavón L, Morales-Montor J. 2015. The bidirectional relationship between sleep and immunity against infections. J Immunol Res. 2015:678164–14. doi:10.1155/2015/678164.
- IGME. 2023. United nations inter-agency group per child mortality estimation. [accessed 2023 May 8]. https://childmortality.org/data/Togo.
- Jacob CM, Baird J, Barker M, Cooper C, Hanson M. 2017. The importance of a life-course approach to health: chronic disease risk from preconception through adolescence and adulthood: White paper World Health Organization. p. 41.
- Laurent de Angulo MS, Brouwers-de Jong EA, Bulk A. 2005. Ontwikkelingsonderzoek in de jeugdgezondheidszorg. Het Van Wiechenonderzoek – De Baecke-Fassaert Motoriek test. Assen: van Gorcum.
- Lauritsen J. 1999. EpiData Software EpiData Software. Analysis.
- Petersdorf C. 2023. An analysis of healthcare systems in Togo. [accessed 2023 May 8]. https://borgenproject.org/an-analysis-of-healthcare-systems-in-togo/.
- Présentation générale. 2023. [accessed 2023 May 8]. https://www.has-sante.fr/plugins/ModuleXitiKLEE/types/FileDocument/doXiti.jsp?id=c_2835466.
- R Core Team. R Core Team. 2020. R: a language and environment for statistical computing. Austria: R Found Stat Comput Vienna.
- Sanoussi Y. 2017. Measurement and analysis of inequality of opportunity in access of maternal and child health care in Togo. BMC Health Serv Res. 17(Suppl 2):699. doi:10.1186/s12913-017-2647-8.
- Siderius EJ, Carmiggelt B, Scheenstra-van Rijn C, Heerkens YF. 2016. Preventive child health care within the framework of the dutch health care system. J Pediatr. 177S: S138–S141. doi:10.1016/j.jpeds.2016.04.050.
- Swe KT, Rahman MM, Rahman MS, Teng Y, Abe SK, Hashizume M, Shibuya K. 2021. Impact of poverty reduction on access to water and sanitation in low- and lower-middle-income countries: country-specific Bayesian projections to 2030. Trop Med Int Health. 26(7):760–774. doi:10.1111/tmi.13580.
- The World Bank. 2023. World Development Indicators [accessed 2023 May 8]. https://data.worldbank.org/country/togo.
- TOGO. 2014. République du Togo. Ministère de la santé. Rapport de la troisième enquête démographique et de Santé (EDST-III); p. 124.
- UN. 2023. Inter-agency Group for Child Mortality Estimation. Levels & Trends in Child Mortality. [accessed 2023 May 8]. https://www.unicef.org/media/60561/file/UN-IGME-child-mortality-report-2019.pdf.
- UNICEF Innocenti. 2020. Worlds of Influence: understanding what shapes child well-being in rich countries. Innocenti Report Card 16. Florence: UNICEF Office of Research – Innocenti.
- Unicef. 2023. UNICEF Data: monitoring the situation of children and women. [accessed 2023 May 8]. https://data.unicef.org/resources/immunization-coverage-are-we-losing-ground/.
- Weber AM, Rubio-Codina M, Walker SP, van Buuren S, Eekhout I, Grantham-McGregor SM, Araujo MC, Chang SM, Fernald LC, Hamadani JD, et al. 2019. The D-score: a metric for interpreting the early development of infants and toddlers across global settings. BMJ Glob Health. 4(6):e001724. doi:10.1136/bmjgh-2019-001724.
- WHO Multicentre Growth Reference Study Group. 2006. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 450:76–85. doi:10.1111/j.1651-2227.2006.tb02378.x.
- WHO Multicentre Growth Reference Study Group. 2007. WHO Child Growth Standards: head circumference-for-age, arm circumference-for-age, triceps skinfold-for-age and subscapular skinfold-for-age: methods and development (p. 217). Geneva: World Health Organization.