ABSTRACT
Individual preferred timing of sleep and activity patterns, known as circadian preference, ranges from definitely morning types to definitely evening types. Being an evening type has been linked to adverse sleep and mental health outcomes. This study aimed to explore the associations between circadian preference and self-reported sleep, depression, anxiety, quality of life, loneliness, and self-harm/suicidal thoughts. Data stem from a national survey of students in higher education in Norway (the SHoT-study). All 169,572 students in Norway were invited to participate, and 59,554 students (66.5% women) accepted (response rate = 35.1%). Circadian preference was associated with sleep and mental health outcomes in a dose–response manner. For both genders, being an evening type (either definitely evening or more evening than morning) was associated with an increase in age-adjusted relative risk (RR-adjusted; range = 1.44 to 2.52 vs. 1.15 to 1.90, respectively) across all outcomes compared with definitely morning types. Overall, the present study provides further evidence that evening circadian preference is associated with adverse sleep and mental health outcomes in young adults. As such, future efforts to improve sleep and mental health in young adults should consider their circadian preferences.
Introduction
Circadian preference refers to individual differences in preferred sleep and activity patterns. On a spectrum, circadian preference (or chronotype) ranges from definitely morning type (“early birds”), who prefer waking early and going early to bed, to definitely evening type (“night owls”), who tend to rise late and stay up late. The remainder of the population typically falls in between as intermediate types (being either rather more a morning than an evening type or rather more an evening than a morning type). Humans are sensitive to variations in sunlight tied to differences in latitude, resulting in an increase in evening-type preference towards higher latitudes (Leocadio-Miguel et al. Citation2017). While young men tend to be more evening oriented than young women, this gender difference diminishes with age and is reversed in old age (Randler and Engelke Citation2019). Further, there is a general biological tendency for a delay in the circadian rhythm during adolescence and early adulthood compared to childhood and later adulthood (Randler and Engelke Citation2019), which consequently for the former age groups implies a later circadian preference. Considering that early rise times are often required due to various daytime obligations, such early morning obligations might – particularly for evening types – curtail sleep duration. If, for example, individuals find themselves unable to fall asleep early enough at night due to a delayed rhythm, they may risk their sleep to be too short, especially if they are not naturally short sleepers (Monk et al. Citation2001; Saxvig et al. Citation2021a).
Evening preference has been linked to higher severity of impaired mental health compared to the other circadian preferences (Adan et al. Citation2012), which has led to speculation on whether circadian preference could be a transdiagnostic risk factor for mental health problems (Taylor and Hasler Citation2018). Specifically, there is evidence of a small, yet significant, association between being an evening type and depressive symptomatology (Norbury Citation2021), while support for a link with anxiety disorders is more contentious (Kivelä et al. Citation2018). A meta-analysis suggested that evening-type preference is associated with schizophrenia and bipolar I disorder (Linke and Jankowski Citation2021). In terms of possible gender differences, several studies have suggested that being an evening type may have a large impact on health outcomes of women compared with men (Fabbian et al. Citation2016), but few studies have examined this in detail across outcomes using large samples.
Data from a survey of Canadian university students (n = 3160, ages 18 to 35) showed that evening types reported the lowest levels of all types of social support (Walsh et al. Citation2022). Further, there is evidence of a link between chronotype and suicidal ideation in adolescents and young adults (Bradford et al. Citation2021; Chan et al. Citation2020), but not between chronotype and suicide attempt among undergraduate students without a psychiatric diagnosis (Lester Citation2015). Further, a study on German university students (n = 164) showed that being an evening type is associated with lower quality of life (Randler Citation2008). The same association was demonstrated to be independent of age in a sample of Polish residents (n = 349; ages 13–59 years) (Jankowski Citation2012).
The recent COVID-19 pandemic has impacted on the quality of life and health of adolescents (Burdzovic Andreas and Brunborg Citation2021; Genta et al. Citation2021), with a shift toward the evening observed in the daily rhythms of both adolescents (Genta et al. Citation2021; Leone et al. Citation2020) and in the general population where there is an increased prevalence of sleep problems (Algahtani et al. Citation2021; Jahrami et al. Citation2021). Taken together, there is substantial evidence that circadian preference impacts on the well-being and quality of life of individuals and that it is particularly important to consider the association between circadian preference, sleep, and a wide range of mental health outcomes in young adults as they tend to be more inclined to have late bedtimes, which is associated with, for example, impaired school performance and motivation (Merikanto et al. Citation2013). As such, there is a need to investigate the associations between circadian preferences, sleep, and mental health in the post-COVID-19 era. The main aim of the present study was to investigate the associations between circadian preferences, sleep, and mental health outcomes using recent data from a large, nationally representative sample of adolescents.
Materials and methods
Procedure
The SHoT study (Students’ Health and Wellbeing Study) is a large survey of students in Norwegian higher education, conducted by three large student welfare associations. Four surveys have been completed since 2010. This report is based on the most recent wave, conducted in 2022. Detailed information of the SHoT study has been described in a previous publication (Sivertsen et al. Citation2019). Data from SHoT2022 were collected from February to April 2022 and included full-time students undertaking higher education in Norway. All 169,572 students enrolled in higher education in Norway received an invitation to participate, of whom 59,554 students completed the web-based questionnaires (response rate: 35.1%).
Ethics
The SHoT2022 study was approved by the Regional Committee for Medical and Health Research Ethics in Western Norway (no. 2022/326437). Informed consent was obtained electronically after the participants had received detailed information about the study.
Instruments
Circadian preference
Circadian preference was assessed according to the following item from the Morningness Eveningness Questionnaire (Horne and Ostberg Citation1976): “One hears about “morning” and “evening” types of people. Which one of these types do you consider yourself to be? 1) Definitely a morning type, 2) Rather more a morning than an evening type, 3) Rather more an evening than a morning type, or 4) Definitely an evening type”.
Sociodemographic and lifestyle information
Data about the participants’ age and gender were extracted from their social identification number, and all participants were asked about their relationship status. Participants were categorized as non-Norwegian if either the student or one or both of their parents were born outside Norway. They also indicated the educational level of their parents as having completed either primary education, secondary education, or college/university.
Sleep variables
The participants’ self-reported usual bedtime and rise time were indicated in hours and minutes. Time in bed (TIB) was calculated as the difference between bedtime and rise time. Sleep onset latency (SOL; “How long does it usually take you to fall asleep (after turning off the lights)?”) and wake after sleep onset (WASO; “How long are you awake during the night (after you first have fallen asleep)?”) were indicated in hours and minutes. Sleep duration was defined as TIB minus SOL and WASO. Sleep efficiency was defined as the ratio of sleep duration to TIB, multiplied by 100 to yield percentage. Oversleeping was measured with one question (“How often do you oversleep?”) and scored on a 5-point scale (“never,” “several times per year,” “several times per month,” “several times per week,” and “every day”). Students who responded “several times per week” or “every day” were categorized as frequently oversleeping.
Mental health problems, anxiety, and depression
Mental health symptoms were assessed using the Hopkins Symptoms Checklist (HSCL-25) (Derogatis et al. Citation1974), derived from the 90-item Symptom Checklist (SCL-90), which is a screening tool designed to detect symptoms of anxiety and depression. It is composed of a 10-item subscale for anxiety and a 15-item subscale for depression, with each item scored on a 4-point scale ranging from “not at all” (1) to “extremely” (4). The period of reference is the prior two weeks. An investigation of the factor structure based on the SHoT2014 dataset showed that an unidimensional model, in contrast to the original subscales of anxiety and depression, has optimal psychometric properties for application to student populations (Skogen et al. Citation2017). As in previous publications, an average score on the HSCL-25 of >2 was used as a cut-off value for identifying high levels of mental health problems.
Quality of life
Quality of life was assessed by the Satisfaction with Life Scale (SWLS) (Diener et al. Citation1985). The SWLS is a 5-item scale designed to measure global cognitive judgments of one’s life satisfaction and is not a measure of either positive or negative feelings. Participants indicate how much they agree or disagree with each of the five items using a 7-point scale ranging from “strongly agree” (7) to “strongly disagree” (1). In the current study, the SWLS was analyzed in two ways: 1) as a continuous total score (range 5–35), and 2) dichotomously, using a total SWLS total score of <19 as the cut-off value for indicating poor life satisfaction.
Loneliness
Loneliness was assessed using an abbreviated version of the widely used UCLA Loneliness Scale, the “Three-Item Loneliness Scale (T-ILS)” (Hughes et al. Citation2004). The T-ILS items (lack of companionship, feeling left out, and isolation) were each rated along a 5-point scale (“never,” “seldom,” “sometimes,” “often,” and “very often”). Students who responded “often” or “very often” on all three items were categorized as having high loneliness. The T-ILS displays satisfactory reliability and both concurrent and discriminant validity (Hughes et al. Citation2004).
Self-harm and suicidal thoughts
Self-harm was assessed according to one item drawn from the Adult Psychiatric Morbidity Survey (APMS) (McManus et al. Citation2016): “Have you ever deliberately harmed yourself in any way but not with the intention of killing yourself?” (yes/no). The question about thoughts of self-harm was adapted from the Child and Adolescent Self-harm in Europe study (CASE) (Madge et al. Citation2008): “Have you ever seriously thought about trying to deliberately harm yourself but not with the intention of killing yourself but not actually done so?” (yes/no). If respondents answered yes to any item, timing of the latest episode was assessed and categorized as recent if it occurred within the last year.
Statistics
IBM SPSS version 28 (SPSS Inc., Chicago, IL, USA) for Windows was used for all analyses. Differences between circadian preference were separately examined across all continuous outcome measures (HSCL-25, SWLS, T-ILS, and sleep parameters) for male and female students by calculating estimated marginal means (EMM) and adjusting for age. We also conducted a log-link binomial regression analysis to calculate effect-sizes for the dichotomous outcomes (mental health problems, anxiety, depression, quality of life, loneliness, self-harm, and suicidal thoughts), adjusting for age. Results are presented as risk ratios (RRs) with 95% confidence intervals. The normality of the data was examined using skewness and kurtosis, and all continuous measures were well within the recommended ranges (±2) (George and Mallery Citation2010). There was generally very little missing data (n < 0.5%); hence, missing values were handled using listwise deletion. As the SHoT2022 study had several objectives and was not designed to specifically study circadian preference, no a priori power calculations were conducted to ensure that the sample size had sufficient statistical power to detect differences in outcomes. Still, it should be noted that the sample comprised nearly 60,000 respondents.
Results
Descriptive statistics
describes the key sociodemographic and clinical characteristics of the full-time students who responded to the SHoT2022 survey. The sample had a mean age of 26.1 years (SD = 7.3 years) and was predominantly female (66.5%), and about half (48.1%) of constituents reported being single.
Table 1. Sociodemographic characteristics of the SHOT 2022 study.
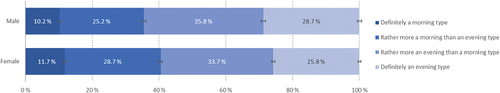
shows the response patterns of circadian preferences of the students (separately for women and men). Approximately 1 in 3 (~30%) reported being definitely an evening type and 1 in 10 reported (~10%) being definitely a morning type. Hence, the remainder (~60%) fell in between as intermediate types (being rather more a morning than an evening type or rather more an evening than a morning type).
Circadian preference and sleep
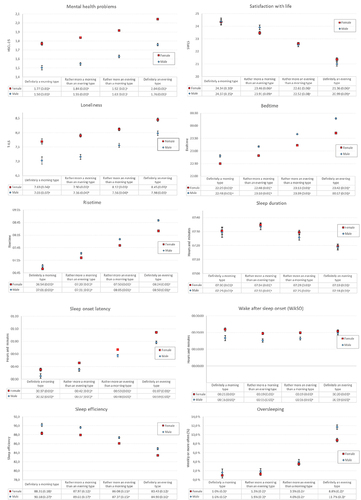
Analyses of the sleep variables (illustrated in ) showed that there was a graded association between circadian preference and several of the sleep variables. Those who reported preferences toward being an evening type tended to stay up later and rise later than individuals with earlier circadian preferences. Further, being more of an evening type was associated with shorter sleep duration, longer SOL, lower SE, and a higher incidence of oversleeping. There were no differences in time spent awake during the night (WASO) depending on circadian preference.
Figure 2. Chronotype and mental health and sleep indicators (Y axis) in male and female college and university students. Values represent age-adjusted estimated marginal means (EMM) and standard errors in parentheses. Error bars represent 95% confidence intervals. Significant chronotype differences are indicated for each row in the table using superscript letters, calculated at the .05 significance level.
Circadian preference and mental health outcomes
In , the associations between circadian preference and mental health and sleep indicators are separately illustrated for women and men. Across all outcomes, there is a graded association between circadian preference and negative outcomes for both genders, implying that the more the evening type, the poorer the outcomes.
As shown in , the analysis of circadian preference and associated health outcomes indicated that being definitely an evening type or more evening than morning type were both associated with a significant increase in age-adjusted relative risk across all dichotomous outcome measures compared with being definitely a morning type and more so for the definitely evening type compared with the more evening than morning type (RR-adjusted range across all outcome measures 1.44–2.52 vs. 1.15–1.90). The strongest associations were found between definitely evening types and depressive symptoms in women (RR-adjusted = 2.17; 95% CI 1.96–2.40) and for anxiety symptoms (RR-adjusted = 2.52; 95% CI 1.97–3.21) and depression (RR-adjusted = 2.41; 95% CI 1.99–2.92) in men. Recent self-harm and suicidal thoughts were each also associated with being definitely an evening type in both women (RR-adjusted = 1.67; 95% CI 1.40–1.98 and 1.76; 95% CI 1.55–2.00, respectively) and men (RR-adjusted = 1.92; 95% CI 1.30–2.83 and 1.76; 95% CI 1.44–2.16, respectively) in stark contrast to being definitely a morning type. There are also some indications that being more a morning than evening type compared with being definitely a morning type was associated with a slightly increased relative risk for depression, poorer quality of life, and recent suicidal thoughts in women (RR-adjusted range 1.09–1.20) and anxiety in men (RR-adjusted = 1.38; 95% CI 1.06–1.78).
Table 2. Chronotype and risk for poor mental health in female and male college and university students.
Further, although having an evening circadian preference compared with a morning circadian preference appeared to put men at higher risk for adverse outcomes compared with women when looking at the data categorically (i.e., RR-adjusted), there was no significant interaction between gender and circadian types on outcomes when the latter were analyzed as continuous variables (as shown in ).
Discussion
This large national survey from 2022 among full-time students at Norwegian universities and colleges shows that circadian preferences toward being an evening type, compared with identifying more with being a morning type, is associated with increased risk of adverse sleep and mental health outcomes. Specifically, identifying as being definitely an evening type is associated with an approximately twofold increase in the risk of reporting symptoms of depression and anxiety. Similarly, those who reported circadian preference toward being an evening type also had poorer quality of life, more loneliness and recent self-harm and suicidal thoughts, as well as overall poorer sleep outcomes compared with those with other circadian preferences. As such, a dose–response relationship was observed between circadian preference and adverse outcomes – the later the circadian preference, the higher the risk for mental health problems.
In the present study, ~10% of participants identified as being definitely morning types, ~60% as intermediate types, and ~30% as definitely evening types. This distribution is comparable to another recent study in a Canadian student population (Walsh et al. Citation2022). Compared with other (pre-pandemic) studies in student populations (BaHammam et al. Citation2011; Jankowski Citation2012), fewer individuals in our sample of Norwegian students (and the sample of Canadian students) report being morning types. Although the different studies are not directly comparable, the distribution of circadian types (with fewer definitely morning types) observed in the present study might reflect a continuation of the increase in a population-wide eveningness preference that has been observed in recent decades, reflecting lasting changes in sleep habits and chronotype preferences (Broms et al. Citation2014; Merikanto and Partonen Citation2020). However, the divergences could also reflect subtle differences between the samples (i.e., nationally representative sample of students vs. nationally representative samples of adults) or method of circadian preference assessment (i.e., based on a single item or a scale). Young adults will have a tendency to exhibit a slightly delayed sleep and activity pattern and, accordingly, it may be reasonable to expect more young adults to report evening-type preferences than morning-type preferences (Roenneberg et al. Citation2004).
As expected, the results of the present study showed that being an evening type was associated with later bedtimes and rise times. There was a dose–response relationship between circadian preference and worse sleep outcomes, in which individuals with later circadian preference took longer to fall asleep and had a lower sleep efficiency, shorter sleep duration, and higher incidence of oversleeping. These observations are supported by previous studies (Roenneberg et al. Citation2019; Saxvig et al. Citation2021b; Vollmer et al. Citation2017). It is possible that, in an attempt to obtain enough sleep, individuals with a later circadian preference will try to fall asleep before feeling sufficiently sleepy (at night). As such, they inevitably will spend more time trying to fall asleep (which also results in lower sleep efficiency) and have a higher risk for oversleeping because they have not slept enough or are not ready to wake up in time for their daytime responsibilities. Another explanation may be that poor sleep in evening types is caused by mental health problems, as these two phenomena are highly correlated (Scott et al. Citation2021). There were, however, no differences in time spent awake during the night after falling asleep depending on circadian preference, possibly indicating that there are no differences between individuals with different circadian preferences with regard to sleep quality after one has fallen asleep.
Our results with regard to evening types more frequently reporting symptoms of depression and anxiety are in line with previous studies in terms of the association with depressive symptoms (Norbury Citation2021) and also support evidence that evening types have higher rates of anxiety symptoms (Silva et al. Citation2020; Walsh et al. Citation2022). A study on chronotype and depressive symptoms in Turkish students (n = 339) found that the relationship between evening type and depressive symptoms is mediated by hopelessness (Üzer and Yücens Citation2020), whereas a study of chronotype and suicidality in Korean university students (n = 5632) found that depressive symptoms also mediate the relationship between chronotype and suicidality (Park et al. Citation2018). It is also conceivable that being an evening type implies that one has difficulty keeping up with or adapting to the rhythm of school and working life, which in turn is a risk factor for other mental health problems (von Schantz et al. Citation2021).
Further, we found that being an evening type (either definitely an evening type or more evening than morning type) is also associated with poorer quality of life and loneliness as well as an increase in the risk for reporting episodes of self-harm and/or suicidal thoughts in the last year. This is in line with findings from previous studies (e.g., Walsh et al. Citation2022), and considering that social support can help improve sleep quality (and wellbeing) during difficult times by reducing anxiety and stress (Xiao et al. Citation2020), it is worrying that evening types, in addition to having a higher risk for developing, for example, depression, possibly experience more loneliness compared with morning and intermediate types. One study in adolescents (n = 280; ages 14–16 years) showed that the association between an evening chronotype and poorer quality of life could be predicted by sleep-related dysfunctional cognitions and mediated by insomnia symptoms (Roeser et al. Citation2012).
Although categorical analysis of the data appeared to indicate that men are at higher risk for adverse outcomes compared with women, there were no significant differences between gender and outcomes when analyzing the data continuously. As such, the present study does not support previous studies (e.g., Fabbian et al. Citation2016) indicating that being an evening type may more greatly impact the health outcomes of women compared with men. Rather, our results suggest that a later circadian preference is associated with an increased risk of adverse sleep and mental health outcomes independently of gender. One possible explanation for the contrary finding compared with previous studies, with regard to gender, is that we controlled for age, and although gender differences in chronotype diminish with age (Randler and Engelke Citation2019), the same is not true for the lifetime prevalence of mental health and sleep problems (Afifi Citation2007).
Public health and clinical implications
Considering the consistent associations between being more of an evening type and adverse outcomes, it is important (independent of the exact distribution of circadian types) that students who are absent from lectures or show signs of not being able to follow mandatory course work (e.g., due to oversleeping, which is associated with evening chronotypes) are provided with a low-effort, readily available intervention aimed at shifting their circadian rhythm. As it is possible to impact the timing of sleep and improve health outcomes for evening-type youths (ages 10–18 years) (Harvey et al. Citation2015) or young adults (Facer-Childs et al. Citation2019) through interventions and that parental factors such as rule setting and parental sleep behaviors are associated with better sleep quality for adolescents (Khor et al. Citation2021), mental health should be evaluated concurrently with circadian preferences (Park et al. Citation2018) and related sleep behaviors. Availability of such help is important considering that later circadian preferences are associated with poorer academic performance (Harvey et al. Citation2018) and, consequently, that even a slight shift toward an earlier circadian rhythm could possibly reduce the incidence of adverse outcomes, for which there is an increased risk due to their association with later circadian preferences. Further, as evening types are more at risk for experiencing mental health problems, low social support, and poorer quality of life, the impact of a general shift toward later bedtimes and rise times, continuing through the COVID-19 pandemic, could also have an overall negative population-wide impact on sleep problems and mental health. Whether there are real population-based changes in circadian preferences following the pandemic should however be studied with greater scrutiny and using appropriate (e.g., longitudinal) study designs. Student welfare organizations and clinicians should be available to assess both mental health symptoms and circadian preference or chronotype upon individual requests, although the mechanisms underlying the association between these symptoms and circadian preference remain unclear (Papaconstantinou et al. Citation2019). Alternatively, the results from this study may be interpreted in terms of lending support to previous research suggesting that adolescent or young adult students will often obtain more sleep if, for example, morning lectures were scheduled to later start times (Albakri et al. Citation2021).
Methodological considerations
Strengths of the present study include the large and heterogeneous sample, the use of validated instruments, and controlling for the impact of age on all outcomes. Additionally, the study presents updated data on the associations between circadian preference (or chronotype), sleep, and mental health in a nationally representative sample of students in higher education after the COVID-19 pandemic. However, the cross-sectional design of the present study represents an important limitation, as it precludes both inference of causality and determining the direction of significant associations. To address this, it would be beneficial to employ designs (e.g., cohort studies) that allow researchers to deduce the direction and nature of the relationship between circadian preferences/rhythms and health outcomes with higher certainty. Another important limitation is the modest response rate (35.1%), with little information about the characteristics of nonparticipants beyond age and sex distribution. Selective participation could bias the strength of the observed relative risks. On the one hand, nonparticipants of health surveys usually have poorer general health than participants (Knudsen et al. Citation2010). On the other hand, people are generally more inclined to participate in a survey if the topic is personally relevant (Edwards et al. Citation2009). Furthermore, while the sample is nationally representative of full-time students, the large sample size precluded the use of objective measures of chronotype or circadian timing of sleep, such as dim light melatonin onset, which would have allowed disentangling the behavioral effects of chronotype from the physiological. Additionally, circadian preference was measured using only one question from the Morningness Eveningness Questionnaire (Horne and Ostberg Citation1976), and we did not differentiate between sleep during the week and on weekends. Further, it should be noted that for all participants, sleep onset latency was longer than 30 minutes, which suggests that all groups have sleep onset latencies above common clinical thresholds. Still, it cannot be ruled out that the finding reflects the poor validity of this measure. For some analyses, continuous variables were categorized/dichotomized, which might have impacted the findings.
Conclusions
Overall, the present study supports the established associations between evening circadian preferences and adverse sleep and mental health outcomes. This is important from a public health perspective as well as for student welfare organizations considering that the availability of interventions aiming to shift the timing of sleep could benefit a large number of students, possibly improving sleep and mental health as well as academic performance. However, there is a need for further research, preferably registry linkage studies and randomized controlled trials, to investigate the direction of the associations and to assess the effects of interventions aimed at shifting the circadian rhythms of young adult evening types who experience mental health problems.
Acknowledgements
We wish to thank all students participating in the study as well as the three largest student associations in Norway (SiO, Sammen, and SiT), who initiated and designed the SHoT study.
Disclosure statement
IWS is currently working for Wonderland AS. The other authors report no potential conflicts of interest.
Data availability statement
The SHoT2022 dataset is administrated by the National Institute of Public Health. Approval from a Norwegian regional committee for medical and health research ethics [https://helseforskning.etikkom.no] is a prerequisite. Guidelines for access to SHoT2022 data are found at [https://www.fhi.no/en/more/access-to-data].
Additional information
Funding
References
- Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V, Randler C. 2012. Circadian typology: A comprehensive review. Chronobiol Int. 29:1153–75. doi:10.3109/07420528.2012.719971
- Afifi M. 2007. Gender differences in mental health. Singapore Med J. 48:385–91.
- Albakri U, Drotos E, Meertens R. 2021. Sleep health promotion interventions and their effectiveness: An umbrella review. Int J Environ Res Public Health. 18:5533. doi:10.3390/ijerph18115533
- Algahtani FD, Hassan S-N, Alsaif B, Zrieq R. 2021. Assessment of the quality of life during COVID-19 pandemic: A cross-sectional survey from the Kingdom of Saudi Arabia. Int J Environ Res Public Health. 18:847. doi:10.3390/ijerph18030847
- BaHammam AS, Almestehi W, Albatli A, AlShaya S. 2011. Distribution of chronotypes in a large sample of young adult Saudis. Ann Saudi Med. 31:183–86. doi:10.4103/0256-4947.78207
- Bradford DRR, Biello SM, Russell K. 2021. Insomnia symptoms mediate the association between eveningness and suicidal ideation, defeat, entrapment, and psychological distress in students. Chronobiol Int. 38:1397–408. doi:10.1080/07420528.2021.1931274
- Broms U, Pitkäniemi J, Bäckmand H, Heikkilä K, Koskenvuo M, Peltonen M, Sarna S, Vartiainen E, Kaprio J, Partonen T. 2014. Long-term consistency of diurnal-type preferences among men. Chronobiol Int. 31:182–88. doi:10.3109/07420528.2013.836534
- Burdzovic Andreas J, Brunborg GS. 2021. Self-reported mental and physical health among Norwegian adolescents before and during the COVID-19 pandemic. JAMA Netw Open. 4:e2121934. doi:10.1001/jamanetworkopen.2021.21934
- Chan NY, Zhang J, Tsang CC, Li AM, Chan JWY, Wing YK, Li SX. 2020. The associations of insomnia symptoms and chronotype with daytime sleepiness, mood symptoms and suicide risk in adolescents. Sleep Med. 74:124–31. doi:10.1016/j.sleep.2020.05.035
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. 1974. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behav Sci. 19:1–15. doi:10.1002/bs.3830190102
- Diener E, Emmons RA, Larsen RJ, Griffin S. 1985. The satisfaction with life scale. J Pers Assess. 49:71–75. doi:10.1207/s15327752jpa4901_13
- Edwards PJ, Roberts I, Clarke MJ, DiGuiseppi C, Wentz R, Kwan I, Cooper R, Felix LM, Pratap S. 2009. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2010. doi:10.1002/14651858.MR000008.pub4
- Fabbian F, Zucchi B, Giorgi AD, Tiseo R, Salmi R, Cappadona R, Gianesini G, Bassi E, Signani F, Raparelli V, et al. 2016. Chronotype, gender and general health. Chronobiol Int. 33:863–82. doi:10.1080/07420528.2016.1176927
- Facer-Childs ER, Middleton B, Skene DJ, Bagshaw AP. 2019. Resetting the late timing of ‘night owls’ has a positive impact on mental health and performance. Sleep Med. 60:236–47. doi:10.1016/j.sleep.2019.05.001
- Genta FD, Rodrigues Neto GB, Sunfeld JPV, Porto JF, Xavier AD, Moreno CRC, Lorenzi-Filho G, Genta PR. 2021. COVID-19 pandemic impact on sleep habits, chronotype, and health-related quality of life among high school students: A longitudinal study. J Clin Sleep Med. 17:1371–77. doi:10.5664/jcsm.9196
- George D, Mallery P. 2010. SPSS for windows step by step: A Simple Guide and Reference, 17.0 Update, 10th Edition, Pearson, Boston.
- Harvey AG, Hein K, Dolsen EA, Dong L, Rabe-Hesketh S, Gumport NB, Kanady J, Wyatt JK, Hinshaw SP, Silk JS, et al. 2018. Modifying the impact of eveningness chronotype (“Night-Owls”) in youth: A randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 57:742–54. doi:10.1016/j.jaac.2018.04.020
- Harvey AG, Soehner AM, Kaplan KA, Hein K, Lee J, Kanady J, Li D, Rabe-Hesketh S, Ketter TA, Neylan TC, et al. 2015. Treating insomnia improves mood state, sleep, and functioning in bipolar disorder: A pilot randomized controlled trial. J Consult Clin Psychol. 83:564–77. doi:10.1037/a0038655
- Horne JA, Ostberg O. 1976. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 4:97–110.
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. 2004. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res Aging. 26:655–72. doi:10.1177/0164027504268574
- Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. 2021. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J Clin Sleep Med. 17:299–313. doi:10.5664/jcsm.8930
- Jankowski KS. 2012. Morningness/eveningness and satisfaction with life in a polish sample. Chronobiol Int. 29:780–85. doi:10.3109/07420528.2012.685671
- Khor SPH, McClure A, Aldridge G, Bei B, Yap MBH. 2021. Modifiable parental factors in adolescent sleep: A systematic review and meta-analysis. Sleep Med Rev. 56:101408. doi:10.1016/j.smrv.2020.101408
- Kivelä L, Papadopoulos MR, Antypa N. 2018. Chronotype and psychiatric disorders. Curr Sleep Med Rep. 4:94–103. doi:10.1007/s40675-018-0113-8
- Knudsen AK, Hotopf M, Skogen JC, Overland S, Mykletun A. 2010. The health status of nonparticipants in a population-based health study: The Hordaland health study. Am J Epidemiol. 172:1306–14. doi:10.1093/aje/kwq257
- Leocadio-Miguel MA, Louzada FM, Duarte LL, Areas RP, Alam M, Freire MV, Fontenele-Araujo J, Menna-Barreto L, Pedrazzoli M. 2017. Latitudinal cline of chronotype. Sci Rep. 7:5437. doi:10.1038/s41598-017-05797-w
- Leone MJ, Sigman M, Golombek DA. 2020. Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic. Curr Biol. 30:R930–R931. doi:10.1016/j.cub.2020.07.015
- Lester D. 2015. Morningness—Eveningness, current depression, and past suicidality. Psychol Rep. 116:331–36. doi:10.2466/16.02.PR0.116k18w5
- Linke M, Jankowski KS. 2021. Chronotype in individuals with schizophrenia: A meta-analysis. Schizophr Res. 235:74–79. doi:10.1016/j.schres.2021.07.020
- Madge N, Hewitt A, Hawton K, Wilde EJD, Corcoran P, Fekete S, Heeringen KV, Leo DD, Ystgaard M. 2008. Deliberate self-harm within an international community sample of young people: Comparative findings from the Child & Adolescent Self-harm in Europe (CASE) study. J Child Psychol Psychiatry. 49:667–77. doi:10.1111/j.1469-7610.2008.01879.x
- McManus S, Bebbington P, Jenkins R, Brugha T, Digital NHS; UK Statistics Authority. 2016. Mental health and wellbeing in England: Adult psychiatric morbidity survey 2014 : A survey carried out for NHS digital by NatCen Social Research and the Department of Health Sciences. University of Leicester. Leed, UK: NHS Digital.
- Merikanto I, Lahti T, Puusniekka R, Partonen T. 2013. Late bedtimes weaken school performance and predispose adolescents to health hazards. Sleep Med. 14:1105–11. doi:10.1016/j.sleep.2013.06.009
- Merikanto I, Partonen T. 2020. Increase in eveningness and insufficient sleep among adults in population-based cross-sections from 2007 to 2017. Sleep Med. 75:368–79. doi:10.1016/j.sleep.2020.07.046
- Monk TH, Buysse DJ, Welsh DK, Kennedy KS, Rose LR. 2001. A sleep diary and questionnaire study of naturally short sleepers. J Sleep Res. 10:173–79. doi:10.1046/j.1365-2869.2001.00254.x
- Norbury R. 2021. Diurnal preference and depressive symptomatology: A meta-analysis. Sci Rep. 11:12003. doi:10.1038/s41598-021-91205-3
- Papaconstantinou EA, Shearer H, Fynn-Sackey N, Smith K, Taylor-Vaisey A, Côté P. 2019. The association between chronotype and mental health problems in a university population: A systematic review of the literature. Int J Ment Health Addict. 17:716–30. doi:10.1007/s11469-018-0006-6
- Park H, Lee H-K, Lee K. 2018. Chronotype and suicide: The mediating effect of depressive symptoms. Psychiatry Res. 269:316–20. doi:10.1016/j.psychres.2018.08.046
- Randler C. 2008. Morningness–eveningness and satisfaction with life. Soc Indic Res. 86:297–302. doi:10.1007/s11205-007-9139-x
- Randler C, Engelke J. 2019. Gender differences in chronotype diminish with age: A meta-analysis based on morningness/chronotype questionnaires. Chronobiol Int. 36:888–905. doi:10.1080/07420528.2019.1585867
- Roenneberg T, Kuehnle T, Pramstaller PP, Ricken J, Havel M, Guth A, Merrow M. 2004. A marker for the end of adolescence. Current Biology. 14:R1038–R1039. doi:10.1016/j.cub.2004.11.039
- Roenneberg T, Pilz LK, Zerbini G, Winnebeck EC. 2019. Chronotype and social jetlag: A (Self-) critical review. Biology. 8:54. doi:10.3390/biology8030054
- Roeser K, Brückner D, Schwerdtle B, Schlarb AA, Kübler A. 2012. Health-related quality of life in adolescent chronotypes—A model for the effects of sleep problems, sleep-related cognitions, and self-efficacy. Chronobiol Int. 29:1358–65. doi:10.3109/07420528.2012.728664
- Saxvig IW, Bjorvatn B, Hysing M, Sivertsen B, Gradisar M, Pallesen S. 2021a. Sleep in older adolescents. Results from a large cross‐sectional, population‐based study. J Sleep Res. 30. doi:10.1111/jsr.13263
- Saxvig IW, Evanger LN, Pallesen S, Hysing M, Sivertsen B, Gradisar M, Bjorvatn B. 2021b. Circadian typology and implications for adolescent sleep health. Results from a large, cross-sectional, school-based study. Sleep Med. 83:63–70. doi:10.1016/j.sleep.2021.04.020
- Scott J, Kallestad H, Vedaa O, Sivertsen B, Etain B. 2021. Sleep disturbances and first onset of major mental disorders in adolescence and early adulthood: A systematic review and meta-analysis. Sleep Med Rev. 57:101429. doi:10.1016/j.smrv.2021.101429
- Silva VM, Magalhaes JEDM, Duarte LL, Kavushansky A. 2020. Quality of sleep and anxiety are related to circadian preference in university students. PLOS ONE. 15:e0238514. doi:10.1371/journal.pone.0238514
- Sivertsen B, Råkil H, Munkvik E, Lønning KJ. 2019. Cohort profile: The SHoT-study, a national health and well-being survey of Norwegian university students. Open Access. 1–8. doi: 10.1136/bmjopen-2018-025200
- Skogen JC, Øverland S, Smith ORF, Aarø LE. 2017. The factor structure of the Hopkins Symptoms Checklist (HSCL-25) in a student population: A cautionary tale. Scand J Public Health. 45:357–65. doi:10.1177/1403494817700287
- Taylor BJ, Hasler BP. 2018. Chronotype and mental health: Recent advances. Curr Psychiatry Rep. 20:59. doi:10.1007/s11920-018-0925-8
- Üzer A, Yücens B. 2020. Chronotype and depressive symptoms in healthy subjects: The mediating role of hopelessness and subjective sleep quality. Chronobiol Int. 37:1173–80. doi:10.1080/07420528.2020.1775629
- Vollmer C, Jankowski KS, Díaz-Morales JF, Itzek-Greulich H, Wüst-Ackermann P, Randler C. 2017. Morningness–eveningness correlates with sleep time, quality, and hygiene in secondary school students: A multilevel analysis. Sleep Med. 30:151–59. doi:10.1016/j.sleep.2016.09.022
- von Schantz M, Leocadio-Miguel MA, McCarthy MJ, Papiol S, Landgraf D. (2021). Genomic perspectives on the circadian clock hypothesis of psychiatric disorders. In: Advances in genetics. Vol. 107. Elsevier. p. 153–91. doi:10.1016/bs.adgen.2020.11.005.
- Walsh NA, Repa LM, Garland SN. 2022. Mindful larks and lonely owls: The relationship between chronotype, mental health, sleep quality, and social support in young adults. J Sleep Res. 31. doi:10.1111/jsr.13442
- Xiao H, Zhang Y, Kong D, Li S, Yang N. 2020. The effects of social support on sleep quality of medical staff treating patients with Coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 26. doi:10.12659/MSM.923549