ABSTRACT
Sleep and light education (SLE) combined with relaxation is a potential method of addressing sleep and affective problems in older people. 47 participants took part in a four-week sleep education program. SLE was conducted once a week for 60–90 minutes. Participants were instructed on sleep and light hygiene, sleep processes, and practiced relaxation techniques. Participants were wearing actigraphs for 6 weeks, completed daily sleep diaries, and wore blue light-blocking glasses 120 minutes before bedtime. Measures included scores of the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), Insomnia Severity Index (ISS), Beck Depression Inventory-II (BDI-II), State-Trait Anxiety Inventory (STAI) and actigraphy measurements of sleep latency, sleep efficiency, and sleep fragmentation. Sleep quality increased after SLE based on the subjective assessment and in the objective measurement with actigraphy. PSQI scores were statistically reduced indicating better sleep. Scores after the intervention significantly decreased in ESS and ISS. Sleep latency significantly decreased, whereas sleep efficiency and fragmentation index (%), did not improve. Mood significantly improved after SLE, with lower scores on the BDI-II and STAI. SLE combined with relaxation proved to be an effective method to reduce sleep problems and the incidence of depressive and anxiety symptoms.
Introduction
Sleep is one of the fundamental needs and is the cornerstone for both physical and mental health. According to research conducted before the COVID-19 pandemic, almost 1/3 of older adults in Europe suffered from sleep problems (van de Straat and Bracke Citation2015). The number increased to 3/4 in individuals after the COVID-19 disease (Dvořáková et al. Citation2022). However, it is important to distinguish between sleep problems and natural age-related sleep changes, as there is no causality between older age and sleep disturbance (Rodriguez et al. Citation2015). Most studies agree on the following natural changes in sleep architecture caused by aging: reduction in sleep efficiency (SE), increase in NREM phase 1 and reduction in NREM phase 3, reduction in REM phase, as well as REM latency in the first cycle (Feinsilver Citation2021). There are also changes in circadian rhythms in old age, where older adults tend to phase advance (Duffy et al. Citation2015). Sleep quality, expressed as sleep efficiency and calculated as the ratio of total sleep time (TST) to total bedtime (TIB), tends to be reduced to less than 85% (Feinsilver Citation2021). Decreased sleep efficiency with increasing age is also associated with increased sleep fragmentation, defined as waking during the night for more than 15 s, respiratory difficulties, and others (Carskadon et al. Citation1982). Sleep latency also increases with aging (Feinsilver Citation2021).
Mild to moderate sleep disturbances (specified as Pittsburgh Sleep Quality Index (PSQI) > 5 points; maximum score is 21) are already associated with deficits in daytime function and dementia, and are strongly associated with mood disorders such as depression and anxiety in older adults (Black et al. Citation2015). Based on WHO projections, more than 22% of the elderly population will suffer from mental health problems in the coming years, and insomnia contributes to a 2-fold higher risk of depression pathogenesis. Late-life depression is a risk factor for cognitive decline, comorbid illnesses, and death, and according to cohort studies, it is a risk factor for suicidality in older adults (Tseng et al. Citation2019). In older adults, however, depression is not often diagnosed and treated, and with treatment, about 1/3 of those treated achieve remission (Irwin et al. Citation2022). Depressive disorders have also been linked to lifestyle (activity, diet, and adequate sleep) (Riera-Sampol et al. Citation2021). After depression is successfully treated, patients also show improvements in sleep (Franzen and Buysse Citation2008), demonstrating the bidirectional and complex relationship between sleep and depression. Programs focusing on lifestyle education, including sufficient sleep, may reduce the risk of depression and anxiety and could serve as general prevention in mental and physical health care (Baglioni et al. Citation2011).
The primary treatment of choice for insomnia is most often pharmacotherapy, which is associated with side effects such as confusion, impaired motor skills, and coordination in the elderly (Gould et al. Citation2014). The use of hypnotics is associated with decreased attention, memory impairment, rebound insomnia, obstructive sleep apnoea, and increased risk of suicide attempts (Edinoff et al. Citation2021). In addition, hypnotic use is only appropriate for a short period, i.e., a few weeks, due to the risk of addiction and the need to increase the dose (Petit et al. Citation2003). Possible alternatives include a several of non-pharmacological methods. Cognitive behavioral therapy for insomnia (CBT-I) is effective and has been shown to achieve long-term improvements over medication (Siebern et al. Citation2012), but is only used in individuals with sleep disturbance. Many people do not address their sleep problems, or too late, so CBT-I is often combined with pharmacotherapy instead of being used as primary prevention (Koffel et al. Citation2018). As another non-pharmacological method, sleep hygiene education (SHE) can be used as a primary prevention. However, according to the American Academy of Sleep Medicine (AASM), it is more effective to combine SHE with other methods for sufficient results (Schutte-Rodin et al. Citation2008), e.g.: stimulus control (such as getting up and going to bed regularly, using bed only for sleep and sex, etc.), cognitive restructuring (changing thinking about sleep, especially feelings of guilt and anxiety about sleep), or therapies based on relaxation and mindfulness (Ebben Citation2021). Relaxation, e.g. Jacobson’s Progressive Muscle Relaxation (PMR) is primarily designed to reduce anxiety and musculoskeletal tension, however, PMR has positive effects on sleep as it relieves anxiety and feelings of acute stress, it also relieves pain, resulting in an increase in subjective well-being, which is important for falling asleep more easily (Sun et al. Citation2013). These facts again point to the importance of simultaneously addressing sleep disorders together with psychological problems such as depression or anxiety. In recent years, the rules of sleep hygiene have been enriched with the rules of light hygiene, thanks to the proven influence of light on circadian rhythm (Czeisler and Gooley Citation2007). Despite this knowledge, the emphasis on light education is not mentioned in studies of non-pharmacological methods. In the field of light hygiene (part of light education), the effect of blue light-blocking glasses, which reduce melatonin suppression and increase subjective sleep quality, has been investigated in the last decade (Ayaki et al. Citation2016). The use of blue light-blocking glasses reduces the risk of circadian dysregulation and improves neuropsychological function (Zimmerman et al. Citation2019). However, studies comparing the effects of blue light between young adults and the elderly have shown a lower sensitivity to the effects of blue light in the elderly, and therefore the individuality of aging must be taken into account (Daneault et al. Citation2016).
Based on the aforementioned AASM recommendation, we decided to use a combination of interventions. One of the main interventions was sleep and light education (SLE). The education also focused on lifestyle (diet, exercise, sleep, smoking, stress), which affects mental health and sleep (Moudi et al. Citation2018) that also feedback on each other. With light and lifestyle education, a more comprehensive impact on the individual and a change in habits may be achieved.
This study aimed to determine the impact of SLE interventions, wearing blue light-blocking glasses, and relaxation in older adults. We hypothesized that when one component, i.e., sleep, is affected, the others, i.e., depression and anxiety, would also be affected. Specifically, both subjective and objective indicators of sleep quality would improve in participants at the end of the study. Furthermore, we hypothesized a reduction in depressive and anxiety symptoms after the education.
Participants and methods
Inclusion criteria for the study: Sleep problems (no diagnosed sleep disorder), age 60–80 years, no diagnosed psychiatric or neurological disease or other serious physical illness.
Recruitment and eligibility of participants
Part of the participants were recruited from a pre-existing research database. Additional participants were recruited via leaflets. Printed leaflets were distributed in doctors´ offices and senior homes, while electronic leaflets were promoted on the National Institute of Mental Health (NIMH) website and shared on social media. More detailed information is shown in . The research was approved by the Ethics Committee of the NIMH and ran from August 2020 to October 2021. On entry, participants completed an entry questionnaire and signed an informed consent form.
Self – report questionnaires and actigraphy
Before entering the study, participants completed a baseline questionnaire containing anamnestic data to rule out diseases that could have affected sleep. Furthermore, the Morningness and Eveningness Questionnaire (MEQ) was used to determine the chronotype of the individual. Subjective sleep quality and ratings of sleep, anxiety, and depressive symptoms were measured using the most commonly used questionnaires in older adults at the beginning (i.e, at the beginning of the first meeting) and at the end of the study (i.e, at the end of the fifth meeting): the Pittsburgh Sleep Quality Index (PSQI), the Insomnia Severity Index (ISI), the Epworth Sleepiness Scale (ESS), the Stress and Anxiety Questionnaire, Part X1 (STAI), the Beck Depression Inventory (BDI-II) (Fabbri et al. Citation2021). Before every meeting participants filled out the following questionnaires: ISI, ESS, STAI, and BDI-II. Participants’ physical activity was continuously monitored using Camntech MotionWatch 8 actigraphs and sleep diaries to supplement the actigraph data. The following data were recorded with the actigraph: total sleep time, sleep efficiency (% sleep time relative to the time in bed), sleep latency (time between getting into bed and falling asleep), and sleep fragmentation (% expression of the sum of time defined as mobile during expected sleep time) (Lujan and Grandner Citation2020).
Participants documented the following information in their sleep diaries each day during the study: the time they went to bed; the time they decided to sleep; the number of times they woke up; the time they woke up (last morning wake-up); the time they got out of bed. They also recorded any daytime naps and the times they took their actigraph off. Data from the sleep diaries were used to complement and validate the actigraphy data.
Participants started using UVEX 1933X blue light-blocking glasses from the second week. They were instructed to wear them two hours before bedtime every day. The reason was to eliminate the negative effect of blue light on circadian rhythm and the consequent reduction of melatonin (Ayaki et al. Citation2016). Participants were educated that it is not only the color of the light that has an effect but also the intensity of the light and the time of exposure (Brown et al. Citation2020). The practice of relaxation techniques was taught at the beginning of week 4: Jacobson’s progressive muscle relaxation and body scan, which was proven to reduce stress and anxiety symptoms (Sun et al. Citation2013). Participants were provided with a recording of the relaxation and with the steps written on paper. At the end of the study, the questionnaire data were compared as before (i.e., at the beginning of the first meeting) vs after education (i.e., at the last meeting). The data from actigraphs and sleep diaries were compared as records obtained during the second and sixth weeks of the study. A comparison of data obtained before and after education has been used in other studies (Blunden et al. Citation2012). To maintain consistency and mitigate the potential for overestimation of results in the absence of a placebo group for comparison, we implemented standardized measures that included filling out the same set of questionnaires during each meeting. This approach ensured uniformity across assessments and minimized any potential biases in the interpretation of outcomes.
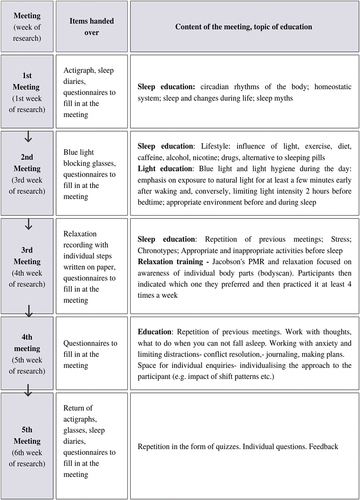
Course and intervention
The schedule and flow of the meetings are shown in . Five group sessions of 60–90 minutes each were conducted throughout the 6-week study. There were 4–6 participants in each group. There was a time interval of two weeks between the first and the second session for familiarization with the actigraph and correct completion of sleep diaries. There was a time interval of one week between the remaining sessions. Initially, the meetings took place at the NIMH in Klecany and later the meetings were held online on the Zoom platform due to the COVID-19 pandemic. In the case of online meetings, actigraphs, glasses, and sleep diaries were sent by post. Questionnaires were always sent online one hour before the meeting and completed by the time the meeting started. The schedule and methods were retained, only converted to an online format.
Statistical analysis
Data from 32 participants, specifically data from 30 actigraphs (reason for excluding analysis: actigraph malfunction, not worn properly throughout the study), and 32 questionnaires were analyzed. Data were compared as before education and at the end of education, week two with week six. Data from questionnaires, actigraphs, and sleep diaries were compared. The actigraphy data sampled in 30s epoch intervals were first processed in the CamNtech software, converted to Excel, and subsequently analyzed in JASP 0.16 using a paired t-test. Mean differences and effect sizes (Cohen’s d) were estimated with 95% confidence interval levels. We used the Mann-Whitney test to compare data from daylight saving time and winter groups, because of the duration of the research over the whole year and the possible influence of seasonality due to changes in light intensity and time shift. A significance level was set for all analyses as p < 0.05.
Results
Comparisons of the results before and after SLE are shown in , Table S1, and described in the following paragraphs. 108 participants were enrolled in the study. 47 participants started the study, and data from 15 of them were not analyzed for the following reasons: 7 participants were excluded from the analysis (reasons in ) and 8 participants did not complete the study. In total, data from 32 participants were analyzed. As shown in , the study participants were mainly women, whose mean age did not differ from that of men. Participants tended to be more of the morning type, but the morning chronotype did not prevail. Body scan was the predominant relaxation method, chosen by 28 of the 32 participants. Mann-Whitney test showed no difference between the daylight saving time and winter time groups, details are shown in Table S2.
Figure 3. Comparison of questionnaire results before and after education.
Figure 4. Comparison of actigraphy-derived metrics before and after education.
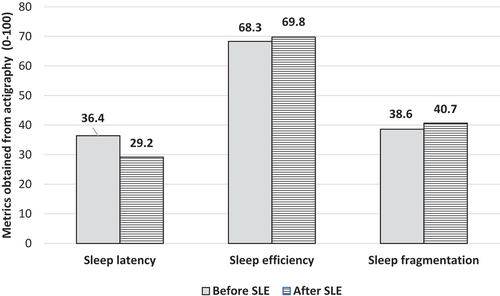
Table 1. Demographic and clinical characteristics of the participants. Data are presented as means. BMI = body mass index; PMR = progressive muscle relaxation.
Changes in subjective questionnaires
shows the results of the pre- and post-intervention questionnaires. Subjective sleep quality statistically increased at the end of the education, as the PSQI scores were reduced (t (31) = 6.04; p < 0.001; Cohen’s d = 1.1). After the education, there was a significant reduction in ISS test scores, indicating a reduction in perceived insomnia symptoms (t (29) = 4.35; p < . 001; Cohen’s d = 0.8). There was also a significant reduction in ESS scores, showing a reduction in perceived daytime sleepiness at the end of education (t (29) = 2.74; p = 0.005; Cohen’s d = 0.5). Results showed a significant reduction in depressive symptoms on the BDI-II after education (t (30) = 3.17; p = 0.002; Cohen’s d = 0.6). There was a significant reduction in scores on the STAI-XI questionnaire at the end of education, i.e., a reduction in perceived anxiety (t (31) = 2.31; p = 0.014; Cohen’s d = 0.4).
Changes in objective assessment of sleep using actigraphy
Actigraphy results are shown in . There was a statistically significant reduction in sleep latency at the end of education compared to before education (t (29) = 1.92; p = 0.032; Cohen’s d = 0.4). Sleep efficiency was higher after education, but not at a statistically significant level. (t (29) = −1.39; p = 0.09; Cohen’s d = −0.3). There was a non-significant increase in sleep fragmentation (%) after education compared to before education (t (29) = −1.93; p = 0.970; Cohen’s d = −0.4).
Discussion
Although sleep and mood disorders cause health and socioeconomic consequences, the problems often go untreated and unnoticed in older adults. Individuals with moderate disorders can experience the onset of clinical difficulties of insomnia and the possibility of onset and worsening of depression or anxiety (Black et al. Citation2015). Consistent with our hypothesis, we confirmed that SLE has a positive effect on aspects of sleep quality and depressive and anxiety symptoms. The results of the questionnaires showed a significant reduction in anxiety and depressive symptoms and an increase in subjective sleep quality. Education was combined with relaxation, specifically Jacobson’s progressive muscle relaxation (PMR) and body scan, as both methods have been shown to be very effective in reducing anxiety, and body scan in reducing depressive symptoms (Corbett et al. Citation2019). In contrast, PMR has been shown to relax muscles and relieve pain (Sun et al. Citation2013). These two choices promoted an individual approach and allowed the individual to choose the more appropriate method, which is essential for the regular practice of relaxation. Similar results, higher subjective sleep quality scores, and reduced depressive symptoms in the elderly were also reached by Reid et al. (Citation2010) using sleep education and aerobic exercise (Reid et al. Citation2010). The combination of education with PMR also occurred in the study of Duman and Taşhan (Citation2018) in postmenopausal women suffering from insomnia. Their results showed a significant decrease in insomnia symptoms after completing the program and the improvement persisted even three months after the program. After completing the SLE, participants rated their insomnia as less severe (ISI) and felt less sleepy according to the ESS, which is reflected in the results of the research by Tanjani et al. (Citation2019).
In terms of actigraphy data, the analysis showed a significant reduction in sleep latency after education in our study. The results of similar studies also clearly show a significant reduction in sleep latency in older adults using sleep education (Chung et al. Citation2018; Drake et al. Citation2019; Elmoneem and Fouad Citation2017). Sleep quality is influenced by various subjective perceptions, including beliefs about sleep and mood, which may not always align with objective measurements. There was no decrease in the sleep fragmentation index, but rather a nonsignificant increase. One reason for this could be the COVID-19 pandemic, as increases in sleep fragmentation were also observed in other studies during this period (Conte et al. Citation2022). During this period, loneliness and feelings of isolation were increased, which has been shown to increase sleep fragmentation as well as increase the incidence of other symptoms of insomnia (Kurina et al. Citation2011).
Many studies show that general group education of seniors improves their psychological health, especially reduces the feeling of loneliness, increases self-esteem, and perception of quality of life (Hung and Lu Citation2014), increases the sense of integrity and enjoyment of the activity (Escuder-Mollon et al. Citation2014). Improvements in subjective sleep quality due to SLE have been shown not only in healthy seniors, but also in individuals who suffer from more serious health problems such as cancer (Zengin and Aylaz Citation2019), diabetes (Pereira et al. Citation2019) or are undergoing dialysis. During the COVID-19 pandemic, there was an enormous increase in isolation and feelings of loneliness, which have been shown to result in poorer sleep quality and an increase in anxiety and depressive symptoms (Escobar-Córdoba et al. Citation2021). SLE achieves significant positive effects on sleep and psychological well-being even in such a stressful period as the COVID-19 pandemic.
The current lifestyle medicine perspective on sleep impairment is based on evidence and links to other lifestyle problems, including obesity, lack of exercise, psychological problems, and health-threatening habits (Terre Citation2014). To alleviate sleep difficulties, a more comprehensive focus is needed than simply addressing the symptoms, as is often the case with drug therapy. However, according to Montazeri Lemrasky et al. (Citation2019), 20% of seniors cope with sleeping problems with medication only (analgesics, anxiolytics, or hypnotics) and according to the European OECD data collection, this is a growing trend not only in the Czech Republic. The benefits of pharmacological treatment often diminish after discontinuation of medication and there is a risk of residual daytime effects (Petit et al. Citation2003). SLE can be considered a simple non-invasive prevention for insomnia and mental health, where psychiatric symptoms are reduced just by treating insomnia (Freeman et al. Citation2017). A significant advantage over pharmacological methods is the possibility of repetition without serious negative effects and the development of dependence (Kwon et al. Citation2021). While other groups that combined SE with other methods focused only on SE without a special emphasis on light education (Duman and Taşhan Citation2018; Reid et al. Citation2010), in our study we enriched the SE with an in-depth education about light and its effect on chronobiology and physiology, as has been done before (Semsarian et al. Citation2021). Based on our results, SLE in combination with other methods thus appears to be one of the suitable methods for the treatment of sleep difficulties. It is also suitable for people with mild and moderate sleep problems and may prevent the onset of clinical insomnia and also serve as primary prevention. Our results are also consistent with those of recent similar research focused on the prevention of depression based on a feedback mechanism of mood and sleep using CBT-I (Irwin and Olmstead Citation2022). In extending this research, the key would be to investigate whether sleep education can be used to achieve increased sleep quality in the long term, while also reducing the risk of depression in older adults.
In addition to the positive results of this study, further benefits can be seen in combining subjective methods with objective ones. SLE is a non-invasive method, that does not require expensive equipment in everyday life and can be performed online. This makes the use of SLE in practice accessible to clients who are unable to commute for whatever reason.
Limits and future recommendations
The main limitation of this study is the smaller sample size. Of the 108 enrolled in the study, 47 entered the study, and almost 1/5 of the enrolled did not meet the entry criteria. Due to the long-term pandemic, the study lasted throughout the year, and our study was not limited to the winter season only. Thus, circadian rhythm may have been affected by changes in light intensity. Therefore, we verified that there was no difference between the summer and winter time groups.
The study’s exclusion criteria, which precluded the inclusion of participants with insomnia or sleep problems comorbid with psychiatric and neurological disorders, present a limitation. This limitation restricts the applicability of the findings to broader populations, as these excluded individuals may possess unique physiological and psychological factors influencing their sleep patterns and responses to interventions.
A comparison of the efficacy of the separate interventions with each other (glasses, relaxation) compared to all interventions combined would also be in place to see which one influenced the measured sleep and mood attributes the most. For example, the practice of relaxation alone achieves improvements in sleep and even cognitive function in older adults (Sun et al. Citation2013). However, it must be kept in mind that the AASM does not recommend SE as a stand-alone method, as mentioned in the introduction.
In the future, to rule out a placebo effect or natural resolution of problems, it is advisable to add a control group that will not undergo education. It is also necessary to examine the long-term effect of SLE over a time frame, (e.g., 1–3 months after education, to verify the longer-term impact of education on the seniors’ sleep, anxiety levels, and depressive symptoms). Based on previous research, it appears that the effects of education remain even three months after completing a similar program (Duman and Taşhan Citation2018). If a long-term effect is demonstrated with our arrangement, SLE could be considered for the prevention of depressive illness in older adults.
Conclusion
This study has shown that a reduction in sleep problems and a reduction in the incidence of depressive and anxiety symptoms can be achieved with simple education and relaxation training. The improvement in subjective sleep quality, along with the reduction in depressive and anxiety symptoms, highlights the interconnectedness of these areas of emotion and sleep and the need to address both issues simultaneously. SLE in combination with relaxation and wearing blue light-blocking glasses proved to be an effective approach that is a low-cost, effective, and readily available solution that can be used not only by psychotherapists and psychologists but also by health or social care staff. SLE could also serve as a prevention tool for sleep and mental health disorders in older adults, and as one possible solution to reduce the use of psychopharmaceuticals and their subsequent dependence in older age.
Ethical statement
This study was approved by the ethics committee of the National Institute of Mental Health. Upon entry into the study, participants were informed of the purpose and duration of the study and the expectations of the study, and their written informed consents were obtained in accordance with the principle of voluntariness.
Supplemental Material
Download PDF (537.8 KB)Acknowledgments
We would like to thank the participants who participated in this research work and the clinical psychologist Mgr. Karolína Janků, Ph.D., who helped us with the educational content. This work was supported by a grant from Charles University Grant Agency, grant no. 355322 and program of Ministry of Health, Czech Republic – conceptual development of research organization (FNKV, 00064173).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/07420528.2024.2337007.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Ayaki M, Hattori A, Maruyama Y, Nakano M, Yoshimura M, Kitazawa M, Negishi K, Tsubota K. 2016. Protective effect of blue-light shield eyewear for adults against light pollution from self-luminous devices used at night. Chronobiol Int. 33:134–139. doi: 10.3109/07420528.2015.1119158.
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, Lombardo C, Riemann D. 2011. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 135:10–19. doi: 10.1016/j.jad.2011.01.011.
- Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR. 2015. Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbance: a randomized clinical trial. JAMA Internal Medicine. 175:494–501. doi: 10.1001/jamainternmed.2014.8081.
- Blunden SL, Chapman J, Rigney GA. 2012. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Med Rev. 16:355–370. doi: 10.1016/j.smrv.2011.08.002.
- Brown TM, Brainard GC, Cajochen C, Czeisler CA, Hanifin JP, Lockley SW, Lucas RJ, Münch M, O’Hagan JB, Peirson SN, et al. 2020. https://Preprints (www.Preprints.org) | NOT PEER-REVIEWED | posted. doi: 10.20944/preprints202012.0037.v1.
- Carskadon MA, Brown ED, Dement WC. 1982. Sleep fragmentation in the elderly: relationship to daytime sleep tendency. Neurobiol Aging. 3:321–327. doi: 10.1016/0197-4580(82)90020-3.
- Chung KF, Lee CT, Yeung WF, Chan MS, Chung EWY, Lin WL. 2018. Sleep hygiene education as a treatment of insomnia: a systematic review and meta-analysis. Fam Pract. 35:365–375. doi: 10.1093/fampra/cmx122.
- Conte F, de Rosa O, Rescott ML, Arabia TP, D’Onofrio P, Lustro A, Malloggi S, Molinaro D, Spagnoli P, Giganti F, et al. 2022. High sleep fragmentation parallels poor subjective sleep quality during the third wave of the COVID-19 pandemic: an actigraphic study. J Sleep Res. 31. doi: 10.1111/jsr.13519.
- Corbett C, Egan J, Pilch M. 2019. A randomised comparison of two ‘stress control’ programmes: progressive muscle relaxation versus mindfulness body scan. Ment Health Prev. 15:200163. doi: 10.1016/J.MPH.2019.200163.
- Czeisler CA, Gooley JJ. 2007. Sleep and circadian rhythms in humans. Cold Spring Harb Symp Quant Biol. 72:579–597. doi: 10.1101/sqb.2007.72.064.
- Daneault V, Dumont M, Massé E, Vandewalle G, Carrier J. 2016. Light-sensitive brain pathways and aging. J Physiol Anthropol. 35. doi: 10.1186/s40101-016-0091-9.
- Drake CL, Kalmbach DA, Arnedt JT, Cheng P, Tonnu CV, Cuamatzi-Castelan A, Fellman-Couture C. 2019. Treating chronic insomnia in postmenopausal women: a randomized clinical trial comparing cognitive-behavioral therapy for insomnia, sleep restriction therapy, and sleep hygiene education. Sleep. 42. doi: 10.1093/sleep/zsy217.
- Duffy JF, Zitting KM, Chinoy ED. 2015. Aging and circadian rhythms. Sleep Med Clin. 10:423–434. W.B. Saunders. doi: 10.1016/j.jsmc.2015.08.002.
- Duman M, Taşhan ST. 2018. The effect of sleep hygiene education and relaxation exercises on insomnia among postmenopausal women: a randomized clinical trial. Int J Nurs Pract. 24. doi: 10.1111/ijn.12650.
- Dvořáková T, Bušková J, Bartoš A. 2022. Neurological symptoms associated with COVID-19 based on a nation-wide online survey [Article in Czech Neurologické příznaky asociované s onemocněním COVID-19 podle celostátního online průzkumu]. Cesk Slov Neurol N. 85:220–227. doi: 10.48095/cccsnn2022220.
- Ebben MR. 2021. Insomnia: behavioral treatment in the Elderl. Clin Geriatr Med. 37:387–399. W.B. Saunders. doi: 10.1016/j.cger.2021.04.002.
- Edinoff AN, Wu N, Ghaffar YT, Prejean R, Gremillion R, Cogburn M, Chami AA, Kaye AM, Kaye AD, Shreveport H. 2021. Zolpidem: efficacy and side effects for insomnia purpose of review. Health Psychol Res. 9. doi: 10.52965/001c.24927.
- Elmoneem HA, Fouad AI. 2017. The effect of a sleep hygiene program on older adults. IOSR J Nurs Health Sci. 6:40–51. doi: 10.9790/1959-0601054051.
- Escobar-Córdoba F, Ramírez-Ortiz J, Fontecha-Hernández J. 2021. Effects of social isolation on sleep during the COVID-19 pandemic. Sleep Sci. 14:86–93. Brazilian Association of Sleep and Latin American Federation of Sleep Societies. doi: 10.5935/1984-0063.20200097.
- Escuder-Mollon P, Esteller-Curto R, Ochoa L, Bardus M. 2014. Impact on senior learners’ quality of life through lifelong learning. Procedia Soc Behav Sci. 131:510–516. doi: 10.1016/j.sbspro.2014.04.157.
- Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. 2021. Measuring subjective sleep quality: a review. Int J Environ Res Public Health. 18:1–57. MDPI AG. doi: 10.3390/ijerph18031082.
- Feinsilver SH. 2021. Normal and abnormal sleep in the elderly. Clin Geriatr Med. 37:377–386. W.B. Saunders. doi: 10.1016/j.cger.2021.04.001.
- Franzen PL, Buysse DJ. 2008. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 10:473–481. doi: 10.31887/dcns.2008.10.4/plfranzen.
- Freeman D, Sheaves B, Goodwin GM, Yu LM, Nickless A, Harrison PJ, Emsley R, Luik AI, Foster RG, Wadekar V, et al. 2017. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. 4:749–758. doi: 10.1016/S2215-0366(17)30328-0.
- Gould RL, Coulson MC, Patel N, Highton-Williamson E, Howard RJ. 2014. Interventions for reducing benzodiazepine use in older people: meta-analysis of randomised controlled trials. Br J Psychiatry. 204:98–107. doi: 10.1192/bjp.bp.113.126003.
- Hung JY, Lu KS. 2014. Research on the healthy lifestyle model, active ageing, and loneliness of senior learners. Educ Gerontol. 40:353–362. doi: 10.1080/03601277.2013.822200.
- Irwin MR, Carrillo C, Sadeghi N, Bjurstrom MF, Breen EC, Olmstead R. 2022. Prevention of incident and recurrent major depression in older adults with insomnia: a randomized clinical trial. JAMA Psychiarty. 79:33–41. doi: 10.1001/jamapsychiatry.2021.3422.
- Irwin MR, Olmstead R. 2022. The direct effect of cognitive behavioral therapy for insomnia on depression prevention and the mediation effect via insomnia remission—reply. JAMA Psychiarty. 79:515. doi: 10.1001/jamapsychiatry.2022.0152.
- Koffel E, Bramoweth AD, Ulmer CS. 2018. Increasing access to and utilization of cognitive behavioral therapy for insomnia (CBT-I): A narrative review. J Gener Inter Med. 33:955–962. doi: 10.1007/s11606-018-4390-1.
- Kurina LM, Knutson KL, Hawkley LC, Cacioppo JT, Lauderdale DS, Ober C. 2011. Loneliness is associated with sleep fragmentation in a communal society. Sleep. 34:1519–1526. doi: 10.5665/sleep.1390.
- Kwon CY, Lee B, Cheong MJ, Kim TH, Jang BH, Chung SY, Kim JW. 2021. Non-pharmacological treatment for elderly individuals with insomnia: a systematic review and network meta-analysis. Front Psychiatry. 11. Frontiers Media S.A. doi: 10.3389/fpsyt.2020.608896.
- Lujan MR, Grandner MA. 2020. Sleep science edited by Hawley Montgomery-Downs. Sleep Vigil. 4:253–254. doi: 10.1007/s41782-020-00116-2.
- Montazeri Lemrasky M, Shamsalinia A, Nasiri M, Hajiahmadi M. 2019. The effect of sleep hygiene education on the quality of sleep of elderly women. Aging Med Healthcare. 10:32–38. doi: 10.33879/amh.2019.1830.
- Moudi A, Dashtgard A, Salehiniya H, Sadat Katebi M, Reza Razmara M, Reza Jani M. 2018. The relationship between health-promoting lifestyle and sleep quality in postmenopausal women. BioMedicine (France). 8(2). doi: 10.1051/bmdcn/2018080211.
- Pereira FH, Trevisan DD, Lourenço DS, Da Silva JB, De Melo Lima MH. 2019. Effect of educational strategies on the sleep quality of people with diabetes: randomized clinical trial. Aquichan. 19:1–13. doi: 10.5294/aqui.2019.19.3.2.
- Petit L, Azad N, Byszewski A, Sarazan FFA, Power B. 2003. Non-pharmacological management of primary and secondary insomnia among older people: review of assessment tools and treatments. Age and Ageing. 32:19–25. doi: 10.1093/ageing/32.1.19.
- Reid KJ, Baron KG, Lu B, Naylor E, Wolfe L, Zee PC. 2010. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. 11:934–940. doi: 10.1016/j.sleep.2010.04.014.
- Riera-Sampol A, Bennasar-Veny M, Tauler P, Nafría M, Colom M, Aguilo A. 2021. Association between depression, lifestyles, sleep quality and sense of coherence in a population with cardiovascular risk. Nutrients. 13:585. doi: 10.3390/nu13020585.
- Rodriguez JC, Dzierzewski JM, Alessi CA. 2015. Sleep problems in the elderly. Med Clin North Am. 99:431–439. W.B. Saunders. doi: 10.1016/j.mcna.2014.11.013.
- Schutte-Rodin SL, Broch L, Buysee D, Dorsey C, Sateia M. 2008. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 4:487–504. doi: 10.5664/jcsm.27286.
- Semsarian CR, Rigney G, Cistulli PA, Bin YS. 2021. Impact of an online sleep and circadian education program on university students’ sleep knowledge, attitudes, and behaviours. Int J Environ Res Public Health. 18:10180. doi: 10.3390/ijerph181910180.
- Siebern AT, Suh S, Nowakowski S. 2012. Non-pharmacological treatment of insomnia. Neurotherapeutics. 9:717–727. doi: 10.1007/s13311-012-0142-9.
- Sun J, Kang J, Wang P, Zeng H. 2013. Self-relaxation training can improve sleep quality and cognitive functions in the older: A one-year randomised controlled trial. J Clin Nurs. 22:1270–1280. doi: 10.1111/jocn.12096.
- Tanjani PT, Khodabakhshi H, Etemad K, Mohammadi M. 2019. Effect of sleep hygiene education on sleep quality and general health of elderly women with sleep disorders living in Birjand City, Iran, in 2016. Iran J Ageing. 14:248–259. doi: 10.32598/sija.13.10.290.
- Terre L. 2014. Clinical implications of impaired sleep. Am J Lifestyle Med. 8:352–370. doi: 10.1177/1559827614521955.
- Tseng TJ, Wu YS, Tang JH, Chiu YH, Lee YT, Fan IC, Chan TC. 2019. Association between health behaviors and mood disorders among the elderly: a community-based cohort study. BMC Geriatr. 19. doi: 10.1186/s12877-019-1079-1.
- van de Straat V, Bracke P. 2015. How well does Europe sleep? A cross-national study of sleep problems in European older adults. Int J Public Health. 60:643–650. doi: 10.1007/s00038-015-0682-y.
- Zengin L, Aylaz R. 2019. The effects of sleep hygiene education and reflexology on sleep quality and fatigue in patients receiving chemotherapy. Eur J Cancer Care (Engl). 28. doi: 10.1111/ecc.13020.
- Zimmerman ME, Kim MB, Hale C, Westwood AJ, Brickman AM, Shechter A. 2019. Neuropsychological function response to nocturnal blue light blockage in individuals with symptoms of insomnia: a pilot randomized controlled study. J Int Neuropsychol Soc. 25:668–677. doi: 10.1017/S1355617719000055.