Abstract
Individuals who require augmentative and alternative communication (AAC) comprise a heterogeneous group, but all need follow-up to assure the appropriateness of implemented interventions. To enable this, outcome measures such as the Family Impact of Assistive Technology Scale for Augmentative and Alternative Communication (FIATS-AAC) may be used. However, instrument must be adapted to the language and culture in which they are to be used. The aim of the study was to therefore to explore the suitability of the Norwegian short-form version (FIATS-AAC-No) by investigating the reliability, validity, and perceived clinical usefulness. The study utilized a mixed-method design, including an online survey and two small group interviews. In total, 47 parents responded to the online survey. The online survey was comprised of three questionnaires, where FIATS-AAC-No was one of the questionnaires. Two group interviews, with two parents and two clinicians, were conducted. Findings show satisfactorily reliability, construct validity and content validity. The interviews revealed a need for specification of key concepts, that there are challenges involved in being parents of a child needing AAC, and that completing questionnaires was perceived as stressful by many parents. The clinicians viewed the FIATS-AAC-No as a potentially useful clinical tool and expressed that it brought to attention the need for follow-up parents have.
Children who require augmentative and alternative communication (AAC) comprise a heterogeneous group with variability in key areas such as motor functioning, comprehension of spoken language, onset and duration of speech impairment, and the environments in which they live. AAC comprises different expressive modalities and a variety of communication systems, including communication books or boards, single-touch communication switches with one prerecorded message, and advanced speech-generating devices where a child may have access to thousands of graphic symbols and the alphabet for spelling, and which may be operated by touch, eye-gaze, or switches (Beukelman & Light, Citation2020). A multidisciplinary assessment is therefore necessary to find the type of AAC intervention that will best fit the child´s needs. Furthermore, follow-up over time is required to ensure that the communication systems and the intervention strategies continue to have the intended effect (Lynch et al., Citation2019; Stadskleiv, Citation2015).
Learning to use AAC is regarded as a form of language development (von Tetzchner, Citation2018). Children develop through interaction and participation with others (Bronfenbrenner, Citation1979; Sameroff, Citation2009), and parents play a vital role providing support to their children’s language development. However, this is more challenging when a child requires AAC. Most parents typically have no experience with AAC until it is recommended for their child. Parents therefore need to be informed, involved and supervised, so they become able to support their child’s communicative development (von Tetzchner & Stadskleiv, Citation2016).
AAC interventions need to be tailored to each child and to also consider how the interventions impact both the child with communication difficulties and their family (Angelo, Citation2000; Bailey et al., Citation2006; Marshall & Goldbart, Citation2008). The professionals need knowledge about what kind of communication systems that a child and the family feel comfortable using and how interventions can be followed up and supported (Johnson, Citation2000; Stadskleiv, Citation2015). A multidisciplinary and family-centered assessment approach is therefore recommended (Coburn et al., Citation2021; Doak, Citation2021; Mandak et al., Citation2017; Moorcroft et al., Citation2019; O'Neill & Wilkinson, Citation2020; Wright & Quinn, Citation2016).
Despite this, it is the design and quality of communication systems that have been the focus of research (Arnott & Alm, Citation2013; Davies et al., Citation2018; Dietz et al., Citation2014; Guasch et al., Citation2022; Light et al., Citation2019; Wisenburn & Higginbotham, Citation2009), with rather few studies examining what impact AAC has on the entire family and how the implemented interventions work (Doak, Citation2021; Erickson et al., Citation2017; McCall et al., Citation1997). Furthermore, few instruments with acceptable levels of reliability and validity are available to measure if the interventions work in a family context (Enderby, Citation2014).
One exception is the Family Impact of Assistive Technology Scale for Augmentative and Alternative Communication (FIATS-AAC), (Ryan & Renzoni, Citation2019), which was developed in Canada to map how aided communication interventions function and how they influence the family situation. It is a questionnaire that is completed by parents of children aged 3–18 years who use aided communication. The FIATS-AAC comprises several dimensions, linked to the framework of the International Classification of Functioning, disability and health for children and youth (ICF-CY) from the World Health Organization (Citation2007). It includes key dimensions of child and family functioning, such as face-to-face communication, the child’s behavior at home and functioning in school, and the child’s self-reliance and need for supervision. The FIATS-AAC is available in two versions, the original full-form version and a short-form version, called FIATS-AAC38 (Ryan & Renzoni, Citation2019). The FIATS-AAC has been found to have satisfactory internal consistency, test-retest reliability, construct validity, and responsiveness (Delarosa et al., Citation2012; Kron et al., Citation2018; Ryan et al., Citation2018).
The language of the FIATS-AAC is English, and thus not suitable in a Norwegian context. However, given the importance of following up on the effectiveness of AAC interventions, using a family-centered approach, we decided to translate the FIATS-AAC into Norwegian. Before introducing a translated version of an instrument designed to measure the outcomes of an intervention, it is important to ensure that it is culturally and linguistically appropriate (Hambleton & Lee, Citation2013). Furthermore, it must be investigated if the translated version of the instrument accurately measures the concept of interest (i.e., the validity of the instrument) and consistently gives the same results (i.e., the reliability of the instrument) (Heale & Twycross, Citation2015).
Therefore, the aim of this study was to investigate whether the Norwegian short-form version of FIATS-AAC, called FIATS-AAC-No, is suitable for use in a Norwegian context. The present study reports the psychometric qualities of the FIATS-AAC-No and how FIATS-AAC-No was perceived by families with children using aided communication and clinicians working with these families. Specifically, the aims of the study were to investigate (a) the internal consistency of the FIATS-AAC-No; (b) the factor structure of FIATS-AAC-No compared to that found in the original version; (c) the validity of the FIATS-AAC-No, and (d) the views of parents and clinicians regarding the usefulness of FIATS-AAC-No.
Method
Research Design
This cross-sectional study applied a mixed-method approach known as a converging parallel design, in which quantitative and qualitative data are collected simultaneously but analyzed separately (Creswell & Clark, Citation2017). To answer the first three research questions, data from an online survey were analyzed using a quantitative approach. To address the fourth research aim, qualitative data from open-ended questions in the online survey as well as information from the small group interviews were analyzed.
The Norwegian Center for Research Data granted ethical approval of the study (2019/#632418). In addition to this approval, it is required in Norway to obtain approval from the Data Manager Officer of a hospital whenever patients are recruited to a study. As the small group interviews involved parents of patients at a University Hospital, ethical approval for the study was therefore also obtained from the Data Manager Officer of the hospital.
Researchers
The first and second author, who at the time of the study were master´s students in Education Science, and the third and the fourth author, both psychologists, participated in the research. In addition to the four authors, two more psychologists were involved in translating the FIATS-AAC into Norwegian. All four psychologists had extensive experience from the fields of neuropsychology, child development, and AAC, and one was bilingual with Norwegian and English as native languages. The first and second author conducted the survey and the small group interviews, analyzed data, and were involved in the writing of the manuscript. the third and fourth author also participated in analyzing data and writing up the manuscript. In addition, a PhD candidate, external to the project but experienced with qualitative research, was paid to transcribe the interviews.
Participants
Participants were parents of children receiving AAC interventions and clinicians working with children using AAC. Two different groups of parents were recruited: one to the online survey and one to the small group interviews. Clinicians were only recruited to participate in the small group interviews.
For parents recruited to the online survey, the inclusion criteria were being a parent of a school-age child receiving AAC interventions. School age was defined as children attending Grades 1–10 (which comprise the mandatory part of the educational system in Norway) and high school (which comprise up to five years following mandatory education). There were no specified exclusion criteria, but because the parents were asked to complete an online survey, they were expected to have sufficient literacy skills in Norwegian do to so.
The parents were recruited to the online survey via three approaches: via e-mails to schools and classes for children with disabilities, via groups on FacebookFootnote1 and via clinicians a University Hospital. First, e-mails were sent in December 2019 to 247 of the 422 municipalities (59%) in Norway, including to all the 180 municipalities with more than 5000 inhabitants. The schools and classes for children with disabilities were located all over Norway. The schools received information about the study, including a link to the online survey itself, and were asked to forward the information and the link to relevant parents. It is not known how many parents the schools contacted, but the recruitment process resulted in 23 replies. In January and February 2020, information about the study and a link to the survey were therefore posted on three Facebook groups for parents of children with disabilities in Norway (Løvemammaene with 9500 members, Alternativ supplerende kommunikasjon with 1700 members and Lillegull Emily’s verden with 5, 000 members). This resulted in a further 19 replies. Finally, parents attending an AAC course at a University Hospital were provided with information about the study from the clinicians giving the course, which resulted in five more respondents. When the survey was closed in February 2020, a total of 47 respondents had completed the online survey, of which 40 were mothers, five fathers, and two other caregivers.
Participants in the small group interviews were parents and clinicians, recruited from the same University Hospital that ran the AAC course. The parents were at the hospital as their children participated in a training program including AAC interventions. The clinicians were recruited from the staff providing the AAC interventions. Two parents and two clinicians gave signed consent to participation.
Measures and materials
The measures comprised the online survey, which was composed of three questionnaires, and the semi-structured interview guide for the small group interviews.
Online Survey questionnaires
The online survey comprised three questionnaires answered by parents (a) a demographic questionnaire designed specifically for this study; (b) the Norwegian version of the short-form of the FIATS-AAC, called the FIATS-AAC-No; and (c) the BAC Communicative Functions questionnaire. The online survey utilized NettskjemaFootnote2, a free web tool for data collection available for students and employees at universities in Norway, which allows for secure storage of sensitive data.
Demographic Questionnaire
This questionnaire was designed for this study and comprised questions about background information, i.e., the child’s age, gender, diagnosis, and use of communication systems. The parents could also answer an open-ended question at the end, asking if they had any further comments.
Fiats-AAC
The FIATS-AAC-No comprise 37 items from seven domains: Behavior (five items), Education (four items), Face-to-face Communication (eight items), Self-reliance (five items), Social versatility (five items), Security (five items), and Supervision (five items) (see ). Each item is a statement that describes the child or family. For example, a statement like “My child tells me what she/he wants” describes the child’s communicative functioning, while the item “I must take my child with me when I go from one room to another” concerns the impact the child’s condition has on the family. Parents use a Likert scale with seven grades to indicate their degree of agreement with each item, ranging from strongly disagree (1) to strongly agree (7).
Table 1. Domains, Definition and Numbers of Items in the Full-form Version (FIATS-AAC), Original Short-form Version (FIATS-AAC38), and the Norwegian Version (FIATS-AAC-No)
In the Norwegian version, FIATS-AAC-No, there are four, not five, questions pertaining to education, thereby resulting in one item less than in the original short-form version, i.e., FIATS-AAC38. The item “My child participates in the classroom” was accidentally omitted in the online survey, which was regrettably only discovered after data collection was completed. However, in another item included in FIATS-AAC-No, the translation into Norwegian ensures that the item covers somewhat more than the original item. In the item “my child participates in community activities”, the Norwegian term “nærmiljøet” is somewhat broader than the original “community activities”, as the term “nærmiljøet” literally translates “the environment close by”. This ensures that also the Norwegian version includes an item covering the child’s participation in activities outside of the home.
BAC Communicative functions
The BAC Communicative Functions is a questionnaire for parents where they evaluate their child’s communicative skills. It was developed as part of the international project, Becoming an aided communicator (von Tetzchner, Citation2018), in which 29 researchers from 16 different countries participated. It consists of 72 items pertaining to the child’s communication, where the parent should evaluate to which degree it is easy for the child to express something. Items include communicative functions such as greeting, confirming, expressing, commenting, and joking.
Small Group interview
In the small group interviews a semi-structured approach was used. The parents and the clinicians were asked about how the FIATS-AAC-No was perceived, whether they found it useful, how they experienced filling out the FIATS-AAC and whether they had any concerns or other comments. The discussions from the small group interviews were audio recorded using the Nettskjema Dictaphone appFootnote3, which allows for secure storage of sensitive information.
Procedures
Adapting FIATS-AAC-No
The adaptation for Norwegian usage followed recommendations from The International Test Commission (Citation2017). The translation process comprised of three phases (a) a translation from English to Norwegian of the long form of FIATS-AAC; (b) a back translation into English of the final version from phase one; (c) minor adjustments after feedback from the original developers. In the first phase, four translations were performed independently and then compared. The intraclass correlation coefficient (ICC) for the four translations was ICC=.59, 95% CI [.44, .72]. There was full consensus between the four reviewers on 13 items and between three reviewers on another 30 items. The main reason for divergence were choice of wording, for example if it was more correct to say “to aid” or “to support.” All items disagreed upon were discussed until 100% agreement was reached. The final version was translated back from Norwegian into English and sent to the developers, and some very minor linguistic corrections were made following their feedback.
Small group interviews
Two interviews were conducted, one with two parents and one with two clinicians. Both interviews were led jointly by the first and second author and were conducted in a quiet room at the University Hospital. Each interview lasted approximately half an hour. Ahead of the interviews, the FIATS-AAC-No was mailed to the participants, as it was not known to either parents or clinicians at the time of the study. The parents were requested to complete the questionnaire with their own child in mind, while the clinicians were asked to familiarize themselves with it, but not requested to fill it out.
Analyses
All statistical analyses were performed using IBM SPSS version 26.0. As the responses from the FIATS-AAC were normally distributed with a non-significant Kolmogorov-Smirnov test of normal distribution, p= .200, parametric tests were chosen.
Reliability
To investigate internal consistency, Cronbach’s alpha (α) was calculated. A Cronbach’s alpha value of ≥.90 is generally regarded as satisfactory for instruments to be used clinically (Bland & Altman, Citation1997).
Validity
Construct validity was explored with a factor analysis, applying a principal components analysis with oblimin rotation. Prior to this, suitability for factor analysis was confirmed using the Kaiser-Mayer-Olkin measure. To investigate content validity, the correlation between FIATS-AAC-No and BAC Communicative Functions was computed. Correlations above .75 are considered acceptable (Koo & Li, Citation2016). As data on the reliability and validity of the BAC Communicative questionnaire is not yet published, the internal consistency of this questionnaire was also investigated. The rationale for choosing to use the BAC Communicative Functions questionnaire despite the lack of psychometric information was that the there are no other measures of aided communication use among school-aged children available in Norwegian, and that the BAC study also included young Norwegian aided communicators.
Inductive Content analysis
The responses to the open-ended question from the demographic questionnaire in the online survey were copied and collected in one document. The two group interviews were transcribed. The responses the parents gave on the survey (PS) and the transcriptions of the interviews with the parents (PI) and clinicians (CI) were then gathered in one document (hereafter referred to as “the transcript”), using line numbering to be able to later identify the source of a citation. The transcript was not translated from Norwegian into English before analyses, so as not lose important details and nuances in the process.
The transcript was explored using the inductive content analysis (Hsieh & Shannon, Citation2005). The analysis involved several steps. First, the transcript was read several times by the first and second author, independently of each other. The transcript was marked to identify central themes and topics, in the first round the explicitly expressed ones and in later readings also the latent content (Miles et al., Citation2020). After several readings, the two readers had each identified text units that contained meaningful content. The content of a text unit was then condensed and coded (see ). All statements concerning the FIATS-AAC-No and how it was perceived were coded, using different colors to be able to keep track of the analyses. For example, a parent said “I think it should be specified what is meant by communication. I was unsure if communication includes body language, gestures and hand guiding.” The condensed meaning of what the parent said was identified as “what is meant by communication?” and it was coded as ‘need for concept definitions’ (see ). All statements pertaining to the need for concept definitions were marked in the same color.
Table 2 Structure of the Content Analysis of Transcripts of Parents and Clinicians’ Reported Experiences of Using FIATS-AAC-No
The codes were then evaluated in light of the purpose of the research question, which was to gain insight into the perceived usefulness of the FIATS-AAC-No. The content, condensed meaning, and codes identified by the first and second author were compared, organized and discussed. The condensed meaning and codes were then discussed with the last author until consensus was reached regarding identified codes. Lastly, they were organized into three main categories. After completion of all analyses, the results were translated into English.
Results
The majority of parents answering the online survey were parents of children in Grades 1–7 with a diagnosis of cerebral palsy, autism spectrum disorder and intellectual disability. They reported that most of the children used a high-tech communication device, either alone or in combination with manual signs, and used AAC both at home and school (see ).
Table 3. Characteristics of Children as Reported by Parents Responding to Online Survey (N = 47)
Research Aim 1
The first research aim focused on the reliability of the FIATS-AAC-No, which was investigated exploring the internal consistency. The Cronbach’s α was .90 for the 37 items included in FIATS-AAC-No. An item analyses showed that all items should be retained, as α ≥ .89 for all individual items. Cronbach’s α was .96. for the BAC Communicative Functions questionnaire.
Research Aims 2 and 3
These research aims addressed the construct and content validity of the FIATS-AAC-No. The construct validity of the FIATS-AAC-No was investigated by examining the factor structure. A four-factor solution fitted the data best. This was determined based on an examination of the scree plot and on number of items with factor loadings >.10. The factors were named Social Competence/Communication, Education, Behavior and Supervision (see ), where Communication was a shortening of the factor named Face-to-face Communication used in the original FIATS-AAC.
Table 4. Factor Structure of the FIATS-AAC-No
Table 5. Correlations Between Factors of FIATS-AAC-No and the BAC Communicative Functions.
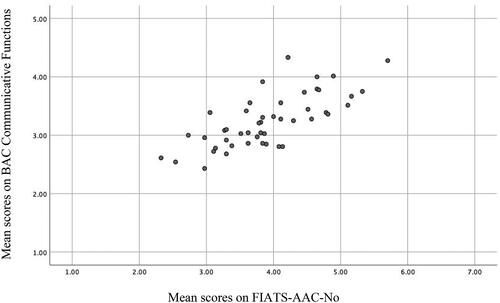
The content validity was investigated by examining the correlation between FIATS-AAC-No and the BAC Communicative Functions questionnaire. The correlation between the instruments was significant, r(46df) = .74, p < .001 (see ). Removing all items from FIATS-AAC-No not directly related to the child’s communication, increased the correlation to r(46df) = .77, p <.001. The correlations between the four identified factors of FIATS-AAC-No and BAC Communicative Functions varied between .31 and .75 (see ).
Research Aim 4
The final research aim concerned how useful the parents and clinicians experienced FIATS-AAC-No to be. Analyzing the transcripts, an initial 14 codes were identified. From these codes emerged three main categories, labeled (a) concept definitions; (b) influence of AAC on the family; and (c) complexity.
Concept Definitions
Parents and clinicians reported that central concepts such as communication, to tell, and family were not defined and that it made them unsure when filling out the scale. For example, parents’ reported that they were unsure if ‘my child communicates’ was to be understood as something else than “my child tells”; specifically, if “to tell” only included expressions involving language in some modality. Some parents seemed to understand “to tell” as any form of verbal and non-verbal communication, others as it involving use of speech. As one parent commented in the survey, “When one has a family member without speech, it is difficult to relate to what is meant by to tell”. For the concept family, it was expressed uncertainty if this referred narrowly to a traditional nuclear family with two parents and siblings, or if it was to be understood as a wider concept also encompassing half- and stepsiblings, stepparents, grandparents, and so forth. Furthermore, some parents reported that the categories on the Likert scale was confusing, as they did not know what it implied to partially agree or disagree. Some parents expressed a wish for a “not relevant” as an answer option.
Influence of AAC on the family
The second category related to the families’ experiences of how AAC influences the family. Parents reported that completing FIATS-AAC-No was challenging. When asked to provide a measure of their child’s functioning, they were reminded of the deficits and this gave rise to a sense of sorrow. The scale also reminded them that having a child using aided communication is stressful. Items that fit poorly with their everyday life was experienced as provocative. However, the parents also stressed that these experiences were not unique to FIATS-AAC-No, but something they often felt when completing questionnaires. In the survey, one parent commented “but we as parents fill out so many questionnaires, and it is quite common that they fit poorly with how our everyday reality is. And it becomes increasingly irritating, I notice.”
Complexity
The third category reflected the complexity involved both in introducing and following-up AAC. Here there was a difference in responses between parents and clinicians. The clinicians were concerned with whether the FIATS-AAC-No would make it possible to determine if a lack of progress was due to the interventions implemented or the child’s developmental potential. The parents focused more on the importance of follow-up of suggested interventions. Clinicians also expressed that this was an important issue, and expressed that parents played a central role related to that. They also expressed concern that there is too little support of parents of children needing AAC, exemplified by the following quote from a clinician:
“I am thinking about sign language for the deaf, which I use. How comprehensive sign language education is, both they and the persons related to them has a right. I have no idea how many hours, but it is not few. And it is not like, that you attend a one-day course, and then you are expected to [pause]… no, now you should be able to develop your child’s language on your own. Go ahead!”
Discussion
The aim of FIATS-AAC, and consequently of FIATS-AAC-No, is to measure if and how AAC interventions affect children using communication systems and their families, and whether the interventions implemented are effective. Children needing AAC is a very heterogeneous group, which implies that it is inherently difficult to develop an instrument that is suitable for everyone and still specific enough to yield useful information.
The results show that the reliability and validity of the FIATS-AAC-No is satisfactory. The expectation of a Cronbach’s α ≥.90 was fulfilled, no items needed to be removed to increase internal consistency, and the correlation with another measure of communicative functioning, the BAC Communicative Functions, was .74. Initially, we had hoped that this correlation would be above .75, but the difference is so small that it is negligible. The BAC Communicative Functions is about parents’ perceptions of their child’s communicative skills, and concerns how parents experience that their child can use aided language to communicate about different topics, for different purposes and in different situations (von Tetzchner, Citation2018). It therefore does not cover all the factors that FIAT-AAC-No does, which in addition to the child’s communicative skills also measures the functional effect of implemented interventions on children and their families. This was supported by finding that the correlations between the factors of FIATS-AAC-No and the BAC Communicative Functions was highest for the factors of FIATS-AAC-No most concerned with interpersonal communication and that the correlation coefficient increased to .77 when removing all items from FIATS-AAC-No not directly related to the child’s communication.
The factor structure of the FIATS-AAC-No was examined, and four factors were found to describe the structure best. The diagnostic groups included in the present study is comparable to those of the original study. The dimensions in the original FIATS-AAC38 were created by reviewing AAC literature, and seven content specialists (five AAC clinicians and two parents) selected the items for each of the seven dimensions or domains using correlational analyses (Delarosa et al., Citation2012; Ryan & Renzoni, Citation2019). In the present study, a factor analytic approach was used. The difference in methodological approach, as well as cultural and linguistic differences between Norway and Canada, explains why there is not a complete overlap between our factors and the original dimension. For example, we found that an item which in Norway was regarded as a measure of communication (i.e., my child tells me when he/she is afraid) was defined as a measure of safety/security in the original version. For the present purpose, it is important that it was possible to identify theoretically meaningful commonalities between the items loading on each of the four factors identified in the FIATS-AAC-No, a finding that gives evidence of a satisfactory construct validity.
Satisfactory psychometric qualities are no guarantee of clinical usefulness. We therefore explored the views of parents and clinicians regarding the use of FIATS-AAC-No. The informants perceived the instrument as potentially clinically meaningful but also identified some barriers that needed to be addressed before launching the FIATS-AAC-No. For example, it should be made clear that unless explicit in the statement that something should be expressed with speech, all modes of expressive communication could be used. Idiosyncratic gestures, signs, symbols, and writing may be included when the question is about whether a child is able to tell something or not. However, telling does not extend to the emotional expression or the body language of a child for items such as my child tells me when she/he feels sick. The importance of this definition is illustrated in some potential inconsistencies found in the answers provided by the parents in the survey. For example, whereas 81% indicated that the child could communicate with family members, only 26% indicated that the child could tell about his/her day. The concept communication therefore seems to be interpreted more broadly than when the word telling is used. This is important to acknowledge when interpreting the results and evaluating a child’s progress. Considering the clinicians expressed need for the FIATS-AAC-No to be more specific, it might be necessary to a priori define precisely what constitutes both telling and communicating in relation to the specific child. Furthermore, the concept of family in this context should be defined, as it could be understood as either those family members that the child is living together with or as family members whom the child encounters on a fairly regular basis, for example uncles or grandparents. Research use requires a clear definition. In clinical use, it is more important that the individual parent/caregiver FIATS-AAC-No use the definition of family in a consistent manner.
In translating the instrument, linguistic and cultural differences were considered to ensure that the adapted version was appropriate for use in Norway (Hambleton & Lee, Citation2013). For example, in Norway questions concerning finances and service provision would need to take into account that all educational and health care services, as well as all communication devices, are provided free of charge. A cultural-linguistic difference between Canada and Norway emerged in relation to the wording on the Likert scale. Very few of the Norwegian respondents used the end points strongly disagree and strongly agree. In the interview with parents, one parent expressed that “if you agree, you cannot agree more”. It is possible that this reflects to the Norwegian sentiment of regarding modesty as a virtue (Bromgard et al., Citation2014). However, a seven-item scale may enable detection of subtle differences from test to retest (Ryan & Renzoni, Citation2010). We rather suggest changing the wording of the answer options in Norwegian from strongly to completely disagree/agree, as that may reflect the Norwegian manner of expressing agreement better. Adding the answer option not relevant might also be considered.
Clinical Implications
Having an instrument that makes it possible to measure of the effects of AAC interventions is very important for clinical practice. However, an important concern that emerged from the study was the stress parents may experience when completing questionnaires such as FIATS-AAC-No. This speaks to the importance of carefully selecting which instruments to ask parents to complete, of carefully considering assessment time points, and of the need for thorough explanations to the parents. Leaving parents with a sense of sorrow over abilities or skills the child is lacking, as well as frustrated about being asked irrelevant questions is clearly not good clinical practice. The clinician should take the time needed to explain that the purpose for FIATS-AAC-No is to identify the child’s achievements, evaluate the interventions and ensure that the intervention strategies are in accord with the child’s progress and in the best interest of the child. Framed in this manner, the FIATS-AAC-No can be viewed as an instrument for promoting the development and mastery of the child.
For the FIATS-AAC-No to function as an instrument measuring the outcome of an intervention, it is important to administer it before or at the very beginning of the intervention, as well as at regular intervals after implementation of the intervention. To ensure reliable results, it is recommended that the FIATS-AAC-No is administered in the same format each time (i.e., as an online questionnaire, a paper-and-pencil format, or as an interview). In a study investigating the responsiveness of the instrument, the interval was 12 weeks after the child received the communication device (Ryan & Renzoni, Citation2019). In a clinical setting, that might be too short a time interval and not feasible due to limited resources (Knudsen et al., Citation2022). For example, in Norway, where it is a stated aim that all children should have equal access to health services and it is detailed when this should happen, we have suggestions for assessment intervals for the largest groups of children needing AAC. For school-aged children with cerebral palsy it is recommended that communication is assessed at least at 5–6, 12–13 and 15–17 years of age (Andersen et al., Citation2022), for school-aged children with Down syndrome it is recommended that communication is assessed at 5–6 and 10–12 years of age (Østby & Halvorsen, Citation2017) and for children with autism spectrum disorder an assessment of language and communication should at the minimum be conducted as part of the diagnostic assessment (Oslo University Hospital, Citation2019). It is obviously too long a time interval to assess effect of an intervention years after implementation, but it might be realistic to assess outcome within the first year following the implementation and then to repeat it when children come for reassessment.
Limitations and future directions
The combination of quantitative and qualitative approaches made it possible to evaluate the psychometric properties of the FIATS-AAC-No and gain insight about how the instrument was perceived by parents and clinicians. The nuances this brought to the discussion are considered a strength. A limitation of the study is the rather low number of participants and the lack of longitudinal data. Even though information about the survey was mailed to schools in 247 municipalities and posted on Facebook groups with more than 16, 000 members, we received only 42 responses via these two recruitment approaches. This probably reflect the demanding everyday life of parents who care for children who use AAC. Furthermore, there is a need for further studies using FIATS-AAC-No to estimate the test-retest reliability of the scale and whether it is able, in a Norwegian context, to reveal the effects of interventions over time. This requires studies applying a longitudinal design.
Conclusion
The aim of the study was to investigate whether the Norwegian short-form version of the outcome measure FIATS-AAC, i.e., FIATS-AAC-No, is suitable for use in a Norwegian context. The findings indicated that FIATS-AAC-No shows promise as a reliable and valid measure of parents’ assessment of AAC interventions. Furthermore, both clinicians and parents agreed that there is a need for a standardized outcome measure based on a family-centered approach, thus strengthening the clinical rationale for initiating the use of FIATS-AAC-No in Norway.
The parents’ responses provide valuable information about how parents may experience having to complete questionnaires, which inevitably illuminates the child’s difficulties as well as achievements. Furthermore, the findings show that key concepts used in a questionnaire need to be defined, as parents and clinicians may apply different interpretations when using the scale.
The FIATS-AAC-No is intended to be used when initiating interventions and when evaluating after some time whether the interventions work as intended, and whether changes are required. A potential benefit of using the FIATS-AAC-No is that the Norwegian welfare system provides children with free access to health care services (The Norwegian Ministry of Health and Care Services, Citation1999), special needs education (The Norwegian Ministry of Education, Citation1998) and communication devices (The Norwegian Ministry of Labor and Social Affairs, Citation1997). This secures follow-up of all families with a child who needs AAC, independent of the family’s economic resources. If the FIATS-AAC-No is utilized widely in the Norwegian context, it may also have the potential to provide large-scale data on the effect of AAC interventions in a national sample, including how the interventions are perceived by the families involved. This information would be beneficial and of interest to researchers and clinicians also in other countries.
Note
The FIATS-AAC (Ryan & Renzoni, Citation2019) was used under license from Holland Bloorview Kids Rehabilitation Hospital, Toronto.
Acknowledgement
The authors thank the participating parents and clinicians, and psychologists Ingvil Okkenhaug and Annette Bondi for assistance with translations.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
1 Facebook is a product of Meta, Menlo Park, CA
2 Nettskjema is offered by TSD (Tjeneste for Sensitive Data), which is owned by the University of Oslo, Norway
3 Nettskjema Dictaphone app is offered by TSD, which is owned by the University of Oslo, Norway
References
- Andersen, G. L., Hollung, S. J., Klevberg, G. L., Kløve, N., Jahnsen, R., & Stadskleiv, K. (2022). Norsk kvalitets- og oppfølgingsregister for cerebral parese (NorCP). [The Norwegian Quality and Follow-up Register for Cerebral Palsy (NorCP.)]. Vestfold Hospital Trust.
- Angelo, D. (2000). Impact of augmentative and alternative communication devices on families. Augmentative and Alternative Communication, 16(1), 37–47. doi:10.1080/07434610012331278894
- Arnott, J. L., & Alm, N. (2013). Towards the improvement of augmentative and alternative communication through the modelling of conversation. Computer Speech and Language, 27(6), 1194–1211. doi:10.1016/j.csl.2012.10.008
- Bailey, R. L., Parette, H. P., Stoner, J. B., Angell, M. E., & Carroll, K. (2006). Family members’ perceptions of augmentative and alternative communication device use. Language, Speech, and Hearing Services in Schools, 37(1), 50–60. doi:10.1044/0161-1461(2006/006)
- Beukelman, D. R., & Light, J. C. (2020). Augmentative and alternative communication: Supporting children and adults with complex communication needs. (Vol. 5). Brookes Publishing Company.
- Bland, J. M., & Altman, D. G. (1997). Cronbach’s alpha. BMJ (Clinical Research Ed.), 314(7080), 572. doi:10.1136/bmj.314.7080.572
- Bromgard, G., Trafimow, D., & Linn, C. (2014). Janteloven and the expression of pride in Norway and the United States. The Journal of Social Psychology, 154(5), 375–378. doi:10.1080/00224545.2014.914884
- Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Harvard University Press.
- Coburn, K. L., Jung, S., Ousley, C. L., Sowers, D. J., Wendelken, M., & Wilkinson, K. M. (2021). Centering the family in their system: A framework to promote family-centered AAC services. Augmentative and Alternative Communication, 37(4), 229–240. doi:10.1080/07434618.2021.1991471
- Creswell, J. W., & Clark, V. L. P. (2017). Designing and conducting mixed methods research. Sage Publications.
- Davies, D. K., Stock, S. E., Herold, R. G., & Wehmeyer, M. L. (2018). GeoTalk: A GPS-enabled portable speech output device for people with intellectual disability. Advances in Neurodevelopmental Disorders, 2(3), 253–261. doi:10.1007/s41252-018-0068-2
- Delarosa, E., Horner, S., Eisenberg, C., Ball, L., Renzoni, A. M., & Ryan, S. E. (2012). Family impact of assistive technology scale: Development of a measurement scale for parents of children with complex communication needs. Augmentative and Alternative Communication, 28(3), 171–180. doi:10.3109/07434618.2012.704525
- Dietz, A., Weissling, K., Griffith, J., McKelvey, M., & Macke, D. (2014). The impact of interface design during an initial high-technology AAC experience: A collective case study of people with aphasia. Augmentative and Alternative Communication, 30(4), 314–328. doi:10.3109/07434618.2014.966207
- Doak, L. (2021). Rethinking family (dis) engagement with augmentative and alternative communication. Journal of Research in Special Educational Needs, 21(3), 198–210. doi:10.1111/1471-3802.12510
- Enderby, P. (2014). Introducing the therapy outcome measure for AAC services in the context of a review of other measures. Disability and Rehabilitation. Assistive Technology, 9(1), 33–40. doi:10.3109/17483107.2013.823576
- Erickson, K., Geist, L., & Hatch, P. (2017). AAC Buy-In at Home: Carefully assessing how a device can meet communication needs is key to promoting its use with a client’s family and friends. The ASHA Leader, 22(2), 46–51. doi:10.1044/leader.FTR1.22022017.46
- Guasch, D., Martín-Escalona, I., Macías, J. A., Francisco, V., Hervás, R., Moreno, L., & Bautista, S. (2022). Design and evaluation of ECO: An augmentative and alternative communication tool. Universal Access in the Information Society, 21, 827–849. doi:10.1007/s10209-021-00819-x
- Hambleton, R. K., & Lee, M. K. (2013). Methods for translating and adapting tests to increase cross-language validity. In D. H. Saklofske, C. R. Reynolds, & V. L. Schwean (Eds.), The Oxford handbook of child psychological assessment. (pp. 172–181). Oxford University Press.
- Heale, R., & Twycross, A. (2015). Validity and reliability in quantitative studies. Evidence-Based Nursing, 18(3), 66–67. doi:10.1136/eb-2015-102129
- Hsieh, H.-F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative health Research, 15(9), 1277–1288. doi:10.1177/1049732305276687
- International Test Commission (2017). The ITC guidelines for translating and adapting tests.
- Johnson, B. H. (2000). Family-centered care: Four decades of progress. Families, Systems, and Health, 18(2), 137–156. doi:10.1037/h0091843
- Knudsen, M., Stadskleiv, K., O'Regan, E., Alriksson-Schmidt, A. I., Andersen, G. L., Hollung, S. J., Korsfelt, Å., & Ödman, P. (2022). The implementation of systematic monitoring of cognition in children with cerebral palsy in Sweden and Norway. Disability and Rehabilitation, 1–10. doi:10.1080/09638288.2022.2094477
- Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155–163. doi:10.1016/j.jcm.2016.02.012
- Kron, A. T., Kingsnorth, S., Wright, F. V., & Ryan, S. E. (2018). Construct validity of the family impact of assistive technology scale for augmentative and alternative communication. Augmentative and Alternative Communication, 34(4), 335–347. doi:10.1080/07434618.2018.1518993
- Light, J., Wilkinson, K. M., Thiessen, A., Beukelman, D. R., & Fager, S. K. (2019). Designing effective AAC displays for individuals with developmental or acquired disabilities: State of the science and future research directions. Augmentative and Alternative Communication, 35(1), 42–55. doi:10.1080/07434618.2018.1558283
- Lynch, Y., Murray, J., Moulam, L., Meredith, S., Goldbart, J., Smith, M., Batorowicz, B., Randall, N., & Judge, S. (2019). Decision-making in communication aid recommendations in the UK: Cultural and contextual influencers. Augmentative and Alternative Communication, 35(3), 180–192. doi:10.1080/07434618.2019.1599066
- Mandak, K., O'Neill, T., Light, J., & Fosco, G. M. (2017). Bridging the gap from values to actions: A family systems framework for family-centered AAC services. Augmentative and Alternative Communication, 33(1), 32–41. doi:10.1080/07434618.2016.1271453
- Marshall, J., & Goldbart, J. (2008). Communication is everything I think.’Parenting a child who needs Augmentative and Alternative Communication (AAC). International journal of Language & Communication Disorders, 43(1), 77–98. doi:10.1080/13682820701267444
- McCall, F., Marková, I., Murphy, J., Moodie, E., & Collins, S. (1997). Perspectives on AAC systems by the users and by their communication partners. International Journal of Language and Communication Disorders, 32(S3), 235–256. doi:10.1080/13682829709177099
- Miles, M. B., Huberman, A. M., & Saldaña, J. (2020). Qualitative data analysis: A methods sourcebook. (Vol. 4). Sage publications.
- Moorcroft, A., Scarinci, N., & Meyer, C. (2019). Speech pathologist perspectives on the acceptance versus rejection or abandonment of AAC systems for children with complex communication needs. Augmentative and Alternative Communication, 35(3), 193–204. doi:10.1080/07434618.2019.1609577
- O'Neill, T., & Wilkinson, K. M. (2020). Preliminary investigation of the perspectives of parents of children with cerebral palsy on the supports, challenges, and realities of integrating augmentative and alternative communication into everyday life. American journal of Speech-Language Pathology, 29(1), 238–254. doi:10.1044/2019_AJSLP-19-00103
- Oslo University Hospital (2019). Regional retningslinje for utredning og diagnostisering av autismespekterforstyrrelse (ASF) [Regional guidelines for assessing and diagnosing autism spectrum disorder (ASD.)]. Oslo University Hospital. https://oslo-universitetssykehus.no/seksjon/regional-kompetansetjeneste-for-autisme-adhd-tourettes-syndrom-og-narkolepsi-helse-sor-ost/Documents/01025_Regional_retningslinje_ASF_A41.pdf
- Ryan, S. E., & Renzoni, A. M. (2010). Family impact of assistive technology scale for AAC (FIATS-AAC). Holland-Bloorview Kids Rehabiliation Hospital.
- Ryan, S. E., & Renzoni, A. M. (2019). Family Impact of Assistive Technology Scale for Augmentative and Alternative Communication (FIATS-AAC) Manual. (Vol. 2.0). Holland-Bloorview Kids Rehabilitation Hospital.
- Ryan, S. E., Shepherd, T. A., Renzoni, A. M., Servais, M., Kingsnorth, S., Laskey, C., Ward, K., & Bradley, K. (2018). Responsiveness of a parent-reported outcome measure to evaluate AAC interventions for children and youth with complex communication needs. Augmentative and Alternative Communication, 34(4), 348–358. doi:10.1080/07434618.2018.1520296
- Sameroff, A. (2009). The transactional model In The transactional model of development: How children and contexts shape each other. (pp. 3–21). American Psychological Association. doi:10.1037/11877-001
- Stadskleiv, K. (2015). Kartlegging [Assessment]. In K.-A. B. Naess & A. V. Karlsen (Eds.), God kommunikasjon med ASK-brukere [Good communication with AAC-users]. (pp. 73–118). Fagbokforlaget.
- The Norwegian Ministry of Education (1998). Law on primary and secondary education. https://lovdata.no/dokument/NL/lov/1998-07-17-61?q=oppl%C3%A6ring
- The Norwegian Ministry of Health and Care Services (1999). Law on patient and user rights. https://lovdata.no/dokument/NL/lov/1999-07-02-63
- The Norwegian Ministry of Labor and Social Affairs (1997). National Insurancey Act. https://lovdata.no/dokument/NL/lov/1997-02-28-19
- von Tetzchner, S. (2018). Introduction to the special issue on aided language processes, development, and use: An international perspective. Augmentative and Alternative Communication, 34(1), 1–15. doi:10.1080/07434618.2017.1422020
- von Tetzchner, S., & Stadskleiv, K. (2016). Constructing a language in alternative forms. In M. M. Smith & J. Murray (Eds.), The silent partner. (pp. 17–34). J&R Press Ltd.
- Wisenburn, B., & Higginbotham, D. J. (2009). Participant evaluations of rate and communication efficacy of an AAC application using natural language processing. Augmentative and Alternative Communication, 25(2), 78–89. doi:10.1080/07434610902739876
- World Health Organization (2007). International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY. World Health Organization.
- Wright, C. A., & Quinn, E. D. (2016). Family-centered implementation of Augmentative and Alternative Communication systems in early intervention. Perspectives of the ASHA Special Interest Groups, 1(1), 168–174. doi:10.1044/persp1.SIG1.168
- Østby, M., & Halvorsen, B. (2017). Retningslinje for oppfølging av barn og unge med Down syndrom [Guideline for follow-up of children and adolescents with Down syndrome]. Oslo University Hospital. https://oslo-universitetssykehus.no/seksjon/regionsenter-for-habiliteringstjenesten-for-barn-og-unge-rhabu/Documents/Retningslinje%20Down%20Syndrom%20versjon%20030217.pdf