Abstract
Background: Reported associations between shiftwork and health have largely been based on occupation-specific, or single sex studies that might not be generalizable to the entire working population. The objective of this study was to investigate whether shiftwork was independently associated with obesity, diabetes, poor sleep, and well-being in a large, UK general population cohort.
Methods: Participants of the UK Biobank study who were employed at the time of assessment were included. Exposure variables were self-reported shiftwork (any shiftwork and night shiftwork); and outcomes were objectively measured obesity, inflammation and physical activity and self-reported lifestyle, sleep and well-being variables, including mental health.
Results: Shiftwork was reported by 17% of the 277,168 employed participants. Shiftworkers were more likely to be male, socioeconomically deprived and smokers, and to have higher levels of physical activity. Univariately, and following adjustment for lifestyle and work-related confounders, shiftworkers were more likely to be obese, depressed, to report disturbed sleep, and to have neurotic traits.
Conclusions: Shiftwork was independently associated with multiple indicators of poor health and wellbeing, despite higher physical activity, and even in shiftworkers that did not work nights. Shiftwork is an emerging social factor that contributes to disease in the urban environment across the working population.
Studies have linked shiftwork to obesity and diabetes in nurses and industry workers, but little is known about the implications of shiftwork for the general workforce
In this large cross sectional study of UK workers, shiftwork was associated with obesity, depression and sleep disturbance, despite higher levels of physical activity.
Shiftwork was associated with multiple indicators of compromised health and wellbeing and were more likely to report neurotic traits and evening preference
Key messages
Background
Shiftwork is associated with detrimental effects on health and wellbeing, including increased risk of diabetes (Citation1–5) and sleep problems (Citation6–8), higher body mass index (BMI) (Citation1,Citation9–12), and increased signs of anxiety and depression (Citation8,Citation13,Citation14). Shiftworkers were once predominantly male, manufacturing sector workers, but this is no longer the case; a recent government survey reported that security services, transport, and communications industries were the most common occupation of shiftworkers in the United Kingdom (Citation15). The effects of shiftwork on metabolic and mental health have been studied predominantly in female nurses in hospitals, and male shiftworkers in industrial plants. These studies have utility in avoiding some confounding or effect modification due to sex, work environment, and shift patterns, but also generate data that might not be applicable to the general population (Citation1,Citation2). Large population-based studies of the general workforce that adjust for multiple lifestyle and work-related confounding factors are required to address these challenges of studying the effects of shiftwork on health.
The objective of this study is to investigate whether shiftwork and night shiftwork are associated with adverse effects on metabolic and mental health and well-being that are independent of confounding factors, in shiftworkers representing diverse occupations from the UK Biobank, a large population-based study.
Methods
Study sample
UK Biobank recruited over 500,000 participants (5.5% response rate) aged 40–69 years, and baseline information (questionnaires, interviews, and physical measurements) was collected at 21 assessment centers across the UK between 2006–2010 (Citation16,Citation17). The 277,168 participants who were employed at the time of recruitment were included in this study.
Exposures and outcomes
Shiftwork was defined by UK Biobank as a work schedule outside usual working hours (9am–5pm weekdays), and night shift as working through normal sleeping hours (12 midnight to 6am). The outcomes of interest were adiposity, diabetes, sleep disturbance, and depressed mood in the 2 weeks preceding assessment. Height, weight, body mass index, and waist circumference, and % body fat (bioelectric impedance), were measured by using standardized methods and instruments ((Citation18) supplementary data). The ratio of neutrophils to lymphocytes (NLR (Citation19) was calculated from analysis of a blood sample collected from each participant at the time of attending the UK Biobank assessment center, and used as a marker of immune activation, that could be suggestive of higher inflammation. Immune activation is thought to contribute to the pathophysiology of diabetes, and the NLR have been previously been specifically associated with metabolic disease (Citation20,Citation21). Self-reported diabetes and cardiovascular disease were recorded by questionnaire, as well as family history of diabetes, hypertension or depression (Supplementary methods).
Sleep duration was self-reported and categorized into: short (<6h), long (>9h) and normal (6–8h). Insomnia was defined as self-report of difficulty falling asleep or waking in the middle of the night. Tiredness was the frequency of fatigue in the last 2 weeks. Daytime sleepiness was unintentionally falling asleep during the daytime and participants classified themselves into morning or evening chronotype.
Neuroticism was assessed using the Eysenck Personality Questionnaire (Revised Short Form) which provided a score from 0 (least) to 12 (most) (Citation22). Current mood was assessed using two questions relating to the preceding 2 weeks: one on depressed mood and another on anhedonia (lacking enthusiasm for life). Participants were also asked whether they had ever consulted a GP in the past for “nerves, anxiety, tension, or depression?” Mood instability was assessed using the question “Does your mood often go up and down?”
Lifestyle and work-related confounding factors
The following covariates were included in the multivariable analyses: age, sex, ethnicity (White, Black, Mixed, Chinese, Asian, Other), Townsend area-deprivation score which is derived from census data on housing, employment, social class and car availability (Citation18), physical activity and sedentary behavior, alcohol intake, fruit and vegetable intake, smoking status, chronotype, sleep duration, diabetes, depression, and hours worked per week. The self-reported level and duration of usual physical activity was used to derive total physical activity measured as metabolic equivalents (MET-hours/week), as previously described (Citation23,Citation24), and physical activity was also measured objectively by a wrist accelerometer worn for 7 days by a subset of participants (n = 103,711) (supplementary methods). A proxy of sedentary behavior was derived by summing the number of self-reported hours spent driving, using a computer and watching television per day (Citation24). Smoking status (never, current, former), the frequency and volume of alcohol intake, and the number of portions of fruit and vegetables ingested per day were assessed by questionnaire.
Statistical analyses
The associations between shiftwork and body composition, prevalent disease, sleep and mood parameters were investigated using regression models; logistic regression for dichotomous outcomes presented as odds ratios (OR) and 95% confidence intervals (95%CI), continuous variables as point estimates and standard errors, and negative binomial regression for count outcome variables as incidence rate ratios and 95%CI, all calculated using Stata14 software. Participants were categorized as:
Nonshiftworkers, those that did not work shifts at all (referent group)
Shiftworkers – those that worked day and/or night shifts
Night shiftworkers – a subset of shiftworkers that usually or always worked nights
Day shiftworkers – a subset of shiftworkers that usually or always worked days
We first compared group (i) and (ii), and then in separate analyses, (i), (iii), and (iv). The relationship between shiftwork and the outcome measures were further investigated by testing for interactions with sex, chronotype, and sleep duration.
Results
The characteristics of the 277,168 participants of this study are summarized in and S1; 49 572 (17.3%) were shiftworkers, with more men in the shiftwork category (55%). Of those reporting shiftwork, 22.3% (n = 11,090) usually or always worked at night, with men again overrepresented. The occupations most commonly reporting shiftwork are shown in Table S1; associate professional occupations (e.g., nurses, technicians) had the highest percentage of shiftworkers (23%), followed by personal services (e.g., bar staff, security guards), (12%). Shiftwork was associated with age, with older workers less likely to report shift work, and participants in Black, Chinese, Mixed, and Asian ethnic groups were more likely to be shiftworkers compared to Whites (). Shiftworkers were also over-represented in the more deprived quintiles of the Townsend score.
Table 1. Characteristics of study participants.
Shiftworkers had higher BMI, waist circumference, and % body fat than nonshiftworkers (), and nightshift workers had a higher BMI and were more likely to be obese than shiftworkers who did not work nights (, Table S5-6). Shiftworkers were more likely to have diabetes, hypertension and angina, but these associations were of borderline significance after adjustment for BMI (; Table S5). The association between shiftwork and BMI varied by sex (p < .001 for interaction term), with shiftwork more strongly associated with BMI in women compared to men (). There were no differences in total fruit and vegetable intake per day. Shiftworkers, and especially night shiftworkers had higher neutrophil to lymphocyte ratio (), even after adjustment for confounding factors, and after exclusion of participants with chronic disease.
Figure 1. Probability of health and lifestyle differences between night/day shiftworkers and all workers in the UK Biobank. The odds ratios in the lower panel are plotted on a different scale to illustrate the higher levels of work-related physical activity reported by the shiftworkers.
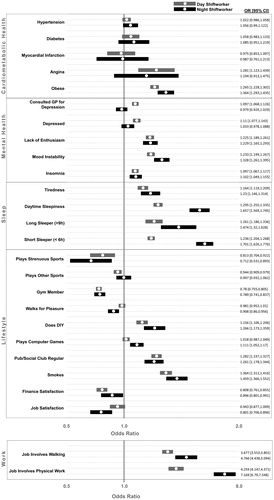
Figure 2. Shiftwork was more strongly associated with BMI in women, particularly for the night shift. Female shiftworkers had increased BMI compared to day workers following adjustment for confounding factors compared to male shiftworkers.
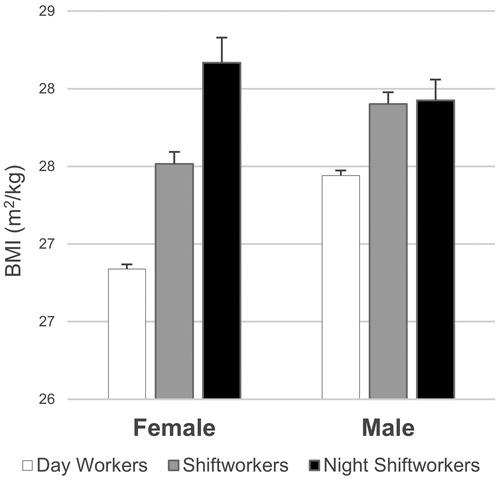
Table 2. Association between shiftwork and metabolic, mental health, and sleep parameters, comparing shiftworkers to those who did not work shifts.
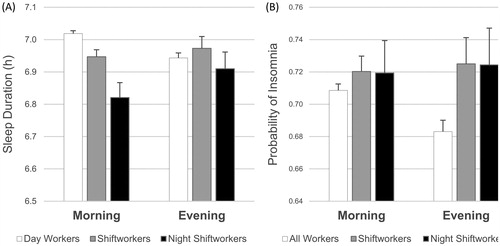
Shiftwork was associated with fewer self-reported hours sleep per day (), and shiftworkers were more likely to report extremely short (<6h) or long (>9h) sleep (; Table S4) as well as poor quality sleep including insomnia, daytime sleepiness, and tiredness in the last 2 weeks (Table S4; ). Night shiftworkers were more likely to report sleep disruption (short- or long-duration, insomnia, daytime sleepiness, and tiredness) compared to nonshiftworkers, and shiftworkers that did not usually work nights (Table S5; )
Figure 3. The effects of shiftwork on sleep were dependent on chronotype. Morning-type shiftworkers reported reduced sleep duration compared to morning day workers, while evening types reported a smaller decrease in sleep duration associated with (A) shiftwork. Shiftwork was associated with increased probability of reporting insomnia in (B) evening types.
Shiftworkers were more likely to report having consulted a general practitioner for depression in the past, mood instability, and to report feeling depressed or lacking in enthusiasm (anhedonic) in the last 2 weeks (; Table S5), but night shiftworkers were less likely to report feeling depressed than other shiftworkers (; Table S6). Neuroticism scores were higher in shiftworkers even after adjusting for depression, smoking, alcohol, and multiple other potential confounding factors, but there was no difference in neuroticism score between day shiftworkers and nightshift workers (Table S6).
Shiftworkers were more likely to report dissatisfaction with their finances in spite of working longer hours, and were more likely to be dissatisfied overall with their job; these associations remained significant following adjustment for confounding factors including depression. Night shiftworkers were more likely to report low job satisfaction compared to shiftworkers that did not work nights (; Table S6). The shiftworkers were more likely to have jobs that involved physical activity compared to the nonshiftworkers (Table S4-5; ), with those working night shifts most likely to have active jobs (Table S4; ).
Shiftworkers, and particularly night shiftworkers, were more likely to report an evening chronotype (). The strength of the association between shiftwork and sleep duration varied by chronotype (p < .001); morning types were more likely to report reduced sleep duration associated with shiftwork compared to evening types (). The odds of reporting sleep disruption were also related to chronotype, with evening types more likely to report daytime sleepiness and insomnia, compared to morning types, especially for the nightshift (p < .01 for interaction term; ).
Shiftworkers and night shiftworkers reported higher levels of both sedentary behavior and physical activity compared to nonshiftworkers, a finding confirmed by accelerometry in subgroup analysis (, , Table S4). Despite this, they were more likely to report sedentary lifestyles; for example, they were more likely to play computer games and to spend time in pubs and social clubs, and less likely to belong to a gym or sports club, compared with nonshiftworkers (). They were however, more likely to report work-related physical activity and to engage in DIY than nonshiftworkers. Nightshift workers were even more likely to report sedentary behavior and physical activity and had increased odds of being a smoker compared to shiftworkers that did not work during nights (; Table S6).
Discussion
Shiftwork was independently associated with obesity in this UK population-based study, extending previous highly selective studies on shiftwork and metabolic health to a wider range of outcomes in a sample of the general population (Citation4,Citation5). The shiftworkers in UK Biobank presented a different personality profile to nonshiftworkers, they had higher neuroticism scores, they were more likely to be evening chronotypes, and to report disrupted sleep, reduced job satisfaction and feeling tired, depressed and lacking enthusiasm. Shiftwork was associated with obesity and with increased inflammation, particularly in nightshift workers, supporting the suggestion that night work might potentiate the effects of shiftwork on metabolic health. These findings were independent of multiple confounding factors, and suggest that shiftwork and especially night shiftwork, affects overall well-being in addition to comprising metabolic health.
The associations between shiftwork and BMI were sex-dependent, with female shiftworkers more likely to be affected, a finding in contrast to previous reports of increased susceptibility of men (Citation4,Citation6). This discrepancy is probably related to the paucity of studies that included both sexes, as well as occupation-related factors that might differentially affect the implications of shiftwork for men and women. Also in contrast to previous work, we did not find strong evidence that the associations between shiftwork and BMI were dependent on chronotype, ethnicity or sleep duration. Shiftworkers were more likely to report diabetes and hypertension, but these associations were largely attenuated by adjustment for BMI.
A striking paradox of this analysis is that shiftworkers reported higher levels of overall physical activity, but still had higher BMI and waist circumference and were more likely to be depressed compared to the nonshiftworkers. Interestingly, however, previous studies consistently report little or no difference between the dietary intake of shiftworkers and nonshiftworkers (Citation1,Citation9,Citation25,Citation26) although the frequency and timing of meals is very potently disturbed (Citation26), and the risk of shiftworkers having metabolic syndrome was associated with the timing of meals but not with overall energy intake (Citation25). Human circadian rhythms in glucose and insulin sensitivity are optimized toward ingestion of food in daytime, yet shiftwork often necessitates that food is ingested at night when these endogenous metabolic rhythms are not prepared for food. Experimental studies in humans and animals have shown that this metabolic mismatch can disrupt blood glucose and triglyceride rhythmicity (Citation27), dampen liver transcriptional rhythms (Citation28), and ultimately lead to compromised pancreatic beta cell function, decreased energy expenditure, leptin resistance, and diabetes (Citation28–30). These mechanisms might underlie the epidemiological associations between BMI and diabetes and shiftwork that are identified in this study and others, and the effects of shiftwork on circadian rhythms in metabolic function require further investigation.
Interestingly, shiftwork was associated with increased ratio of neutrophils to lymphocytes, a marker of low grade inflammation that has been previously associated with metabolic disease (Citation19–21). This association persisted even when participants with chronic disease were excluded, and after adjustment for multiple confounding factors, supporting that shiftwork might independently contribute to systemic inflammation. Previous studies have also reported higher systemic inflammation in shiftworkers (Citation31,Citation32), and this might be one mechanism through which shiftwork could contribute to the risk of cardiometabolic disease.
The shiftworkers in the UK Biobank were more likely to report an evening preference, which may be important as this phenotype is associated with susceptibility to metabolic disease including increased BMI (Citation33–35), metabolic syndrome (Citation33), type 2 diabetes and hypertension (Citation35), as well as all-cause mortality (Citation36), and might contribute to the increased prevalence of metabolic disease in shiftworkers. Shiftwork might be attractive to those with evening chronotypes, facilitating their late night preference, while morning chronotypes might be less tolerant to shiftwork causing them to drop out, or not to consider occupations where shiftwork is a requirement. The association between sleep and shiftwork was strongly dependent on chronotype with morning-types reporting shorter shiftwork-associated sleep times, while the sleep time of the evening-type shiftworker was minimally affected. Despite this smaller effect of shiftwork on sleep duration, evening chronotype shiftworkers were still more likely to report insomnia and daytime sleepiness. Morning chronotypes might be less able to acquire adequate sleep in daytime after shiftwork, causing them to self-select out of shiftwork. Prospective studies are warranted to establish if shiftwork encourages development of an evening preference, or if evening types are more likely to undertake, and to remain in, shiftwork. In support of the latter, shiftworkers also had higher neuroticism scores which might be another example of self-selection of shiftwork by people with specific behavioral phenotypes. Neuroticism is a personality trait that is thought to be stable throughout life, and although neuroticism score is related to depression (Citation37), neuroticism remained associated with shiftwork in this study even after adjustment for self-reported depression, suggesting that people with these personality traits self-select shiftwork. Neuroticism has been previously associated with metabolic disease, and high neuroticism scores were predictive of having metabolic syndrome in a cross-sectional study (Citation38). The high prevalence of personality traits that might predispose to metabolic disease (evening chronotype, neuroticism) that we report in the shiftworkers participating in UK Biobank might contribute to their increased risk of metabolic disease.
Shiftworkers were more likely to report mood instability and depression in this study, which concurs with previous work reporting a higher prevalence of depressive symptoms in nurses that worked shifts (Citation39). Shiftworkers were also more likely to smoke, to regularly use nonprescription analgesic and gastroesophageal reflux medication, to report unhappiness with their finances and their jobs, fatigue and lack of enthusiasm. These indicators of reduced well-being were independent of confounding factors, and suggest that shiftwork had extensive negative effects on overall quality of life. Multiple aspects of shiftwork could mediate these effects. For example, disruption of circadian rhythms is associated with mood disorder in humans, and causes depressive behavior and neurobiological changes in animals (Citation40). Lack of exposure to sunlight, isolation and reduced opportunities to engage in social activity and family life could also contribute to negative effects of shiftwork on mood. Mood and metabolic disorders are frequent co-morbidities (Citation41,Citation42), with overlapping pathophysiology (e.g., inflammation, insulin resistance, neurocognitive deficits), and animal studies link central insulin resistance to behavioral changes (Citation43). It should be considered if the effects of shiftwork on mental health might contribute to the increased metabolic disease already associated with these work schedules.
Implications
The implications of shiftwork for health and well-being are an important consideration as society edges further toward a 24/7 lifestyle. The data presented here associate shiftwork with compromised metabolic health, sleep, mood and job dissatisfaction, even in shiftworkers that do not regularly work nights. Causality is not inferred, and prospective studies are required to establish the nature of the associations between shiftwork and metabolic and mental health. Shiftworkers were more likely to have higher BMI despite higher physical activity, yet there is little evidence that they eat more than nonshiftworkers (Citation4,Citation25). It may be more beneficial to modulate the timing and frequency of their meals and activity rather than volume. However, even if this were possible, it will not address the fundamental uncoupling of physiological and environmental timing that most likely underlies the effects of shiftwork on metabolism and behavior.
Strengths and limitations
The greatest strength of this study is that it was population-based; recruitment to UK Biobank was completely independent of employment status, so the participants represented an unbiased sample of the whole UK workforce. This is the largest study of the association between shiftwork and health across diverse occupations that served to minimize the potential work-related confounding effects of studying shiftworkers in hospitals and factories. However, the response rate of UK Biobank was low (5.5%) so the data might not be representative of either the general population or the shiftworking population in terms of age, sex, ethnicity, and socioeconomic deprivation (Citation17). A strength of this study is that we were able to provide objectively measured activity data from accelerometers to confirm our findings using self-reported data that activity levels were higher in shiftworkers. The accelerometer data were also used to quantify circadian rhythmicity and sleep patterns in shiftworkers, but these data are beyond the scope of this manuscript. Shiftwork encompasses all possible work patterns outside of normal working hours, and it is a limitation that we were unable to categorize these data any further than to discriminate between day and night shiftwork, and that we were not able to account for the duration of shiftwork from the data in UK Biobank. We cannot be certain that the comparison group of nonshiftworkers did not include some people that had been shiftworkers in the past. The self-reported nature of some of the data is a potential limitation, but this was minimized by trimming unlikely observations, and by the large sample size. The quantitative and objective measures of body composition, inflammation, and physical activity are strengths, but there is a limitation that quantitative measures of dietary intake were not available for the whole UK Biobank sample. However, many previous studies have addressed the issue of diet in shiftworkers, but none have shown differences in food intake that could account for their increased obesity and diabetes risk.
Conclusions
Shiftwork should be considered as a factor contributing to the effects of the urban environment on health and well-being across diverse occupations.
suppl_tables_261116.docx
Download MS Word (113.3 KB)Acknowledgements
CW was supported by a Lord Kelvin Adam Smith Fellowship from the University of Glasgow This research has been conducted using the UK Biobank resource. UK Biobank was established by the Wellcome Trust, Medical Research Council, Department of Health, Scottish Government and the Northwest Regional Development Agency. It has also had funding from the Welsh Assembly Government and the British Heart Foundation.
Disclosure statement
The authors report no declarations of interest.
Additional information
Funding
References
- Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Medicine. 2011; 8:e1001141.
- Suwazono Y, Dochi M, Sakata K, Okubo Y, Oishi M, Tanaka K, et al. A longitudinal study on the effect of shift work on weight gain in male Japanese workers. Obesity (Silver Spring, Md). 2008;16:1887.
- Morikawa Y, Nakagawa H, Miura K, Soyama Y, Ishizaki M, Kido T, et al. Shift work and the risk of diabetes mellitus among Japanese male factory workers. Scand J Work Environ Health. 2005;31:179.
- Gan Y, Yang C, Tong X, Sun H, Cong Y, Yin X, et al. Shift work and diabetes mellitus: a meta-analysis of observational studies. Occup Environ Med. 2015;72:72–8.
- Proper KI, van de Langenberg D, Rodenburg W, Vermeulen RC, van der Beek AJ, van Steeg H, van Kerkhof LW. The relationship between shift work and metabolic risk factors: a systematic review of longitudinal studies. Am J Prev Med. 2016;50:e147–57.
- Puttonen S, Viitasalo K, Härmä M. The relationship between current and former shift work and the metabolic syndrome. Scand J Work Environ Health. 2012; 38:343–8.
- Vallières A, Azaiez A, Moreau V, LeBlanc M, Morin CM. Insomnia in shift work. Sleep Med. 2014;15:1440–8.
- Øyane NM, Pallesen S, Moen BE, Akerstedt T, Bjorvatn B. Associations between night work and anxiety, depression, insomnia, sleepiness and fatigue in a sample of Norwegian nurses. PLoS One. 2013;8:e70228.
- Guo Y, Rong Y, Huang X, Lai H, Luo X, Zhang Z, et al. Shift work and the relationship with metabolic syndrome in Chinese aged workers. PLoS One. 2015; 10:e0120632.
- De Bacquer D, Van Risseghem M, Clays E, Kittel F, De Backer G, Braeckman L. Rotating shift work and the metabolic syndrome: a prospective study. Int J Epidemiol. 2009; 38:848.
- Givens ML, Malecki KC, Peppard PE, Palta M, Said A, Engelman CD, et al. Shiftwork, Sleep Habits, and Metabolic Disparities: Results from the Survey of the Health of Wisconsin. Sleep Health. 2015; 1:115–20.
- Marqueze EC, Ulhôa MA, Moreno CR. Irregular working times and metabolic disorders among truck drivers: a review. Work. 2012; 41:3718–25.
- Bara AC, Arber S. Working shifts and mental health–findings from the British Household Panel Survey (1995–2005). Scand J Work Environ Health. 2009; 35:361–7.
- Driesen K, Jansen NW, van Amelsvoort LG, Kant I. The mutual relationship between shift work and depressive complaints–a prospective cohort study. Scand J Work Environ Health. 2011; 37:402–10.
- Health Survey for England. 2013. [cited 2017 Feb 16]. Available from: www.hscic.gov.uk/pubs/hse2014trend.
- Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015; 12:e1001779.
- Swanson JM. The UK Biobank and selection bias. Lancet. 2012; 380:110.
- UK Biobank: Protocol for a large-scale prospective epidemiological resource. Protocol No: UKBB-P. UK Biobank, 2007.
- Shiny A, Bibin YS, Shanthirani CS, Regin BS, Anjana RM, Balasubramanyam M, et al. Association of neutrophil-lymphocyte ratio with glucose intolerance: an indicator of systemic inflammation in patients with type 2 diabetes. Diabetes Technol Ther. 2014; 16:524–30.
- Liu X, Zhang Q, Wu H, Du H, Liu L, Shi H, et al. Blood neutrophil to lymphocyte ratio as a predictor of hypertension. Am J Hypertens. 2015; 28:1339–46.
- Guo X, Zhang S, Zhang Q, Liu L, Wu H, Du H, et al. Neutrophil:lymphocyte ratio is positively related to type 2 diabetes in a large-scale adult population: a Tianjin Chronic Low-Grade Systemic Inflammation and Health cohort study. Eur J Endocrinol. 2015; 173:217–25.
- Smith DJ, Escott-Price V, Davies G, Bailey ME, Colodro-Conde L, Ward J, et al. Genome-wide analysis of over 106 000 individuals identifies 9 neuroticism-associated loci. Mol Psychiatry. 2016;21:749–57.
- Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003; 35:1381–95.
- Celis-Morales CA, Lyall DM, Anderson J, Iliodromiti S, Fan Y, Ntuk UE, et al. The association between physical activity and risk of mortality is modulated by grip strength and cardiorespiratory fitness: evidence from 498 135 UK-Biobank participants. Eur Heart J. 2017; 38:116-22.
- Esquirol Y, Bongard V, Mabile L, Jonnier B, Soulat JM, Perret B. Shift work and metabolic syndrome: respective impacts of job strain, physical activity, and dietary rhythms. Chronobiol Int. 2009; 26:544–59.
- de Assis MA, Kupek E, Nahas MV, Bellisle F. Food intake and circadian rhythms in shift workers with a high workload. Appetite. 2003; 40:175–83.
- Morris CJ, Purvis TE, Mistretta J, Scheer FA. Effects of the Internal Circadian System and Circadian Misalignment on Glucose Tolerance in Chronic Shift Workers. J Clin Endocrinol Metab. 2016; 101:1066–74.
- McHill AW, Melanson EL, Higgins J, Connick E, Moehlman TM, Stothard ER, et al. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc Natl Acad Sci USA. 2014; 111:17302–7.
- Leproult R, Holmbäck U, Van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014; 63:1860–9.
- Salgado-Delgado R, Angeles-Castellanos M, Buijs MR, Escobar C. Internal desynchronization in a model of night-work by forced activity in rats. Neuroscience. 2008; 154:922–31.
- Sookoian S, Gemma C, Fernández Gianotti T, Burgueño A, Alvarez A, González CD, et al. Effects of rotating shift work on biomarkers of metabolic syndrome and inflammation. J Intern Med. 2007; 261:285–92.
- Kim SW, Jang EC, Kwon SC, Han W, Kang MS, Nam YH, et al. Night shift work and inflammatory markers in male workers aged 20-39 in a display manufacturing company. Ann Occup Environ Med. 2016; 28:48.
- Yu JH, Yun CH, Ahn JH, Suh S, Cho HJ, Lee SK, et al. Evening chronotype is associated with metabolic disorders and body composition in middle-aged adults. J Clin Endocrinol Metab. 2015; 100:1494–502.
- Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012; 22:939–43.
- Merikanto I, Lahti T, Puolijoki H, Vanhala M, Peltonen M, Laatikainen T, et al. Associations of chronotype and sleep with cardiovascular diseases and type 2 diabetes. Chronobiol Int. 2013; 30:470–7.
- Broms U, Pitkäniemi J, Bäckmand H, Heikkilä K, Koskenvuo M, Peltonen M, et al. Long-term consistency of diurnal-type preferences among men. Chronobiol Int. 2014; 31:182–8.
- Smith DJ, Nicholl BI, Cullen B, Martin D, Ul-Haq Z, Evans J, et al. Prevalence and characteristics of probable major depression and bipolar disorder within UK biobank: cross-sectional study of 172,751 participants. PLoS One. 2013; 8:e75362.
- Phillips AC, Batty GD, Weiss A, Deary I, Gale CR, Thomas GN, et al. Neuroticism, cognitive ability, and the metabolic syndrome: The Vietnam experience study. J Psychosom Res. 2010; 69:193–201.
- Lee HY, Kim MS, Kim O, Lee IH, Kim HK. Association between shift work and severity of depressive symptoms among female nurses: the Korea Nurses' Health Study. J Nurs Manag. 2016; 24:192–200.
- Bedrosian TA, Fonken LK, Walton JC, Haim A, Nelson RJ. Dim light at night provokes depression-like behaviors and reduces CA1 dendritic spine density in female hamsters. Psychoneuroendocrinology. 2011; 36:1062.
- Pan A, Keum N, Okereke OI, Sun Q, Kivimaki M, Rubin RR, et al. Bidirectional association between depression and metabolic syndrome: a systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012; 35:1171–80.
- Kan C, Silva N, Golden SH, Rajala U, Timonen M, Stahl D, et al. A systematic review and meta-analysis of the association between depression and insulin resistance. Diabetes Care. 2013; 36:480–9.
- Kleinridders A, Cai W, Cappellucci L, Ghazarian A, Collins WR, Vienberg SG, et al. Insulin resistance in brain alters dopamine turnover and causes behavioral disorders. Proc. Natl Acad Sci USA. 2015; 112:3463–8.

