Abstract
Objective
Delayed extubation was commonly associated with increased adverse outcomes. This study aimed to explore the incidence and predictors and to construct a nomogram for delayed extubation after thoracoscopic lung cancer surgery.
Methods
We reviewed medical records of 8716 consecutive patients undergoing this surgical treatment from January 2016 to December 2017. Using potential predictors to develop a nomogram and using a bootstrap-resampling approach to conduct internal validation. For external validation, we additionally pooled 3676 consecutive patients who underwent this procedure between January 2018 and June 2018. Extubation performed outside the operating room was defined as delayed extubation.
Results
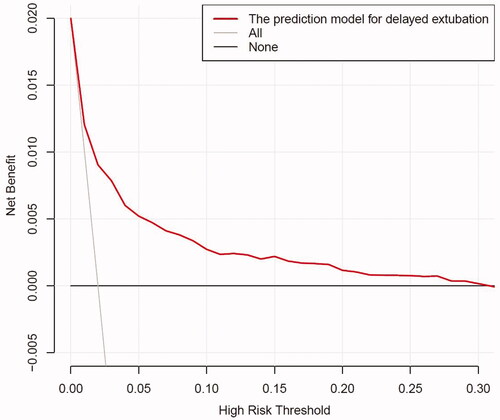
The rate of delayed extubation was 1.60%. Multivariate analysis identified age, BMI, FEV1/FVC, lymph nodes calcification, thoracic paravertebral blockade (TPVB) usage, intraoperative transfusion, operative time and operation later than 6 p.m. as independent predictors for delayed extubation. Using these eight candidates to develop a nomogram, with a concordance statistic (C-statistic) value of 0.798 and good calibration. After internal validation, similarly good calibration and discrimination (C-statistic, 0.789; 95%CI, 0.748 to 0.830) were observed. The decision curve analysis (DCA) indicated the positive net benefit with the threshold risk range of 0 to 30%. Goodness-of-fit test and discrimination in the external validation were 0.113 and 0.785, respectively.
Conclusion
The proposed nomogram can reliably identify patients at high risk for the decision to delayed extubation after thoracoscopic lung cancer surgery. Optimizing four modifiable factors including BMI, FEV1/FVC, TPVB usage, and operation later than 6 p.m. may reduce the risk of delayed extubation.
This study identified eight independent predictors for delayed extubation, among which lymph node calcification and anaesthesia type were not commonly reported.
Using these eight candidates to develop a nomogram, we could reliably identify high-risk patients for the decision to delayed extubation.
Optimizing four modifiable factors, including BMI, FEV1/FVC, TPVB usage, and operation later than 6 p.m. may reduce the risk of delayed extubation.
Key Messages:
Introduction
Tracheal extubation after surgery is a critical step in a patient’s recovery from general anaesthesia (GA). And more than 20% of major complications associated with airway management occur around the time of extubation, with severe consequences such as hypoxemia and death [Citation1,Citation2]. Although many guidelines focus on endotracheal intubation, the literature on tracheal extubation at the end of operation is limited [Citation3,Citation4]. Prolonged endotracheal intubation is not a beneficial process, which may result in related airway complications regarding pneumonia, laryngeal injury, glottic stenosis and dysphagia [Citation5–8]. Also, it takes up the limited medical resource, greatly reducing the transition efficiency in post-anaesthesia care unit (PACU) and intensive care unit (ICU) [Citation9]. Thus, it is of great clinical significance to identify high-risk patients and adjust predictors of delayed extubation in order to reduce its incidence and related complications.
With the ageing of the population and the promotion of low-dose computed tomography (LDCT) screening for lung cancer [Citation10], there will be an increasing number of patients and accompanied with severity of comorbidities in thoracic surgery. In addition, the specific attributes of thoracic surgery, such as unique physiology of one-lung ventilation (OLV) including hypoperfusion or reperfusion, atelectasis or reinflation, and increased inflammatory mediators and postoperative incisional chest wall pain, all increase the uncertainty of postoperative extubation [Citation11,Citation12]. Currently, underlying predictors for delayed extubation have been explored in several fields such as cardiac, thoracotomy, neurosurgical, liver transplantation and spine populations [Citation9,Citation13–17]. However, to date, no document has researched predictors for delayed extubation after thoracoscopic lung cancer surgery. Besides, many of the published factors associated with delayed extubation cannot be modified [Citation18]. Further, no effective and well-performing model was established for predicting the possibility of delayed extubation.
Therefore, by reviewing a large number of medical records, this study aims to explore the incidence and potential predictors and to construct a nomogram to predict the decision to delayed extubation after this surgery. Moreover, considering the reported influence of timing of operation and attending handoff on delayed extubation in other surgical specialties [Citation9,Citation18,Citation19], this study also attempts to investigate the interaction of the two factors on delayed extubation.
Materials and methods
Ethics
This single-centre retrospective study was performed following the approval of the Institutional Review Board (IRB) of Shanghai Chest Hospital (Chair: Dr. Zheng Ning, permission NO.IS22039) on 7 June 2022, with informed consent waived. This article adheres to STROBE guidelines [Citation20].
Study design and patients
Between January 2016 to December 2017, we reviewed medical records of 8716 consecutive patients undergoing thoracoscopic lung cancer surgery to identify predictors and to construct a nomogram for the decision to delayed extubation. For the external validation of the proposed model, we additionally pooled 3676 consecutive patients who underwent this surgical treatment between January 2018 and June 2018. Excluded patients were described in the flow diagram (Supplementary Figure 1).
Data collection, outcomes and definition
Perioperative clinical data were prospectively extracted from our institution’s electronic medical records, including patient’s preoperative characteristics and intraoperative variables such as tumour size, advanced tumour stage (T ≥ 2), hypoxemia, lymph nodes calcification and involvement, type of resection, approach, anaesthesia type, location of resection and so on. Hypoxemia was defined as SPO2≤90% lasting for 5 min. Based on previously published document, 6 p.m. was used as the watershed for the timing of the operation, considering that the onset of thoracoscopic lung surgery later than 6 p.m. developed an increased risk of intraoperative complications [Citation21]. Extubation performed outside the operating room was defined as delayed extubation, which was determined by the anaesthesiologist and thoracic chief surgeon in view of the patient’s preoperative status and intraoperative adverse events [Citation5,Citation9,Citation15,Citation19].
Statistical analysis
Statistical power calculations were not performed prior to this study since the sample size was based on available data in our dataset. Statistics and data analysis plans were defined before accessing the data and were completed after the data were accessed. Continuous variables were compared using Two independent sample t-test or Mann-Whitney U test based on the occurrence of delayed extubation. Categorical variables were compared with Chi-square test or Fisher exact test, depending on the sample size. Univariate analysis showed that all factors significantly correlated with delayed extubation (p < .2) were inserted into the multivariate logistic regression model using the forward selection strategy.
The predictive model was presented with a nomogram to provide a visual point system to estimate the probability of delayed extubation. Hosmer-Lemeshow (H-L) goodness-of-fit test was used to evaluate the model’s fit. Discrimination (concordance statistic, C-statistic) and calibration (calibration curves) were used to evaluate the performance of the prediction model. To reduce overfitting and quantify optimism, the nomogram was internally validated with an approach to 1000 bootstrapped resampling and calculating an optimism-corrected C-statistic. Decision curve analysis (DCA) was used to assess the clinical validity and net benefit of the nomogram [Citation22].
For external calibration, the differences between the mean predicted and observed probability were compared by using a H-L type χ2 statistic. And a large p value (>.05) indicates good calibration. The area under the receiver operating characteristic curve (AUROC) and the optimal cutoff values were calculated to assess model’s discrimination. Statistical analysis was performed using the SPSS 26.0 software (IBM Corp., Armonk, NY, USA). R version 4.1.2 was used with the packages of rms, rmda, forestplot, tidyr, dplyr, pROC, ResourceSelection and PredictABEL. p Value < .05 was considered statistically significant.
Results
Study cohort
From January 2016 to June 2018, 12,392 patients underwent thoracoscopic lung cancer surgery, of which 21.3% (2645 out of 12,392) underwent segmentectomy resection and 78.7% (9747 out of 12,392) underwent lobectomy resection, 1.60% (139 out of 8716) and 1.40% (50 out of 3676) occurred delayed extubation in the development and validation cohorts. The rate of thoracic paravertebral blockade (TPVB) usage in the development and validation cohorts was 11.2% and 22.8%, respectively.
Model development
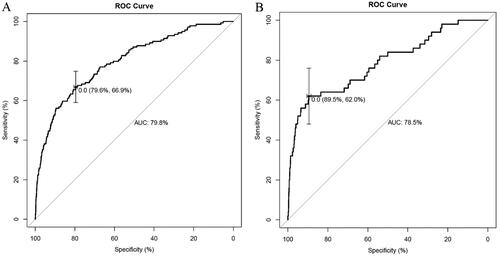
Univariate analysis identified that fifteen variables were significantly associated with delayed extubation in the development cohort (). Multivariate analysis identified that older age (Odds ratio (OR)=1.035, 95%CI, 1.016 to 1.054, p < .001), elevated BMI (OR = 1.066, 95%CI, 1.009 to 1.127, p = .023), increased FEV1/FVC (OR = 0.971, 95%CI, 0.953 to 0.989, p = .002), lymph nodes calcification (OR = 2.032, 95%CI, 1.161 to 3.556, p = .013), GA plus TPVB (vs GA alone, OR = 0.174, 95%CI, 0.055 to 0.552, p = .003), intraoperative transfusion (OR = 3.646, 95%CI, 1.567 to 8.485, p = .003), prolonged operative time (OR = 1.008, 95%CI, 1.004 to 1.011, p < .001), and operation later than 6 p.m. (OR = 11.925, 95%CI, 8.079 to 17.603, p < .001) were independent predictors for delayed extubation (). Using these eight candidates to develop a nomogram to predict the probability of delayed extubation ().
Figure 1. Forest plot of independent predictors of delayed extubation. BMI: body mass index; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; TPVB: thoracic paravertebral blockade.
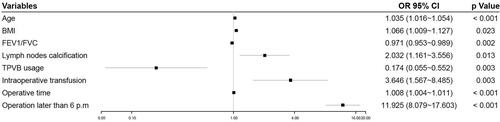
Figure 2. A novel nomogram to predict delayed extubation. The nomogram provides a visual point system based on the combination of patient characteristics (age, BMI, FEV1/FVC, lymph nodes calcification, combined with TPVB, intraoperative transfusion, operative time and operation later than 6 p.m.) to estimate the probability of delayed extubation. To calculate the probability of delayed extubation, the points of eight variables determined on the scale were added to obtain the total points. Draw a vertical line from the total points scale to the last axis to obtain the corresponding probability of delayed extubation. BMI: body mass index; FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; TPVB: thoracic paravertebral blockade.
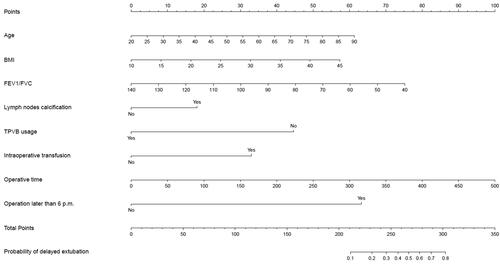
Table 1. Preoperative and intraoperative patient characteristics.
Model performance and internal validation
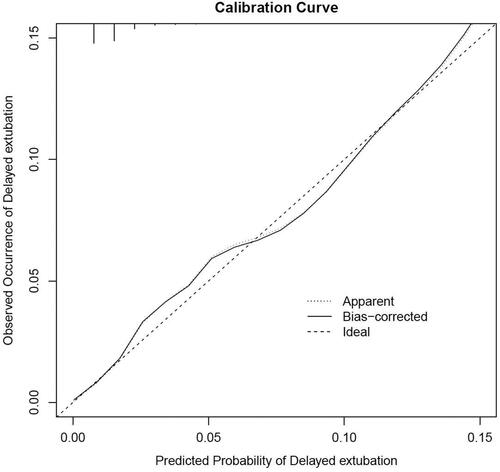
H-L goodness-of-fit test value was 0.527. The C-statistic value of the prediction model was 0.798 (95%CI, 0.758 to 0.838), which showed good discrimination. The sensitivity and specificity based on AUROC curve were 66.9% and 79.6%, respectively (). The apparent calibration curve was close to the 45° ideal line, indicating that the observed probability was consistent with predicted probability in the development cohort (). To reduce the optimism of the model, internal validation with 1000 bootstrap approach was conducted, which reflect good discrimination with optimism-corrected C-statistic of 0.789 (95%CI, 0.748 to 0.830). And the bias-corrected calibration curve also demonstrated that the prediction model was well calibrated when the actual observed probability of delayed extubation was less than 15% ().
Figure 4. Internal calibration curves. A completely accurate prediction model will generate a plot where the probability of the actual observed and predicted corresponding completely and fall along the 45°line (dashed line). The apparent calibration curve (dotted line) represents the calibration of the model in the development data set, while the bias-corrected curve (solid line) is the calibration result after correcting the optimism with the 1000 bootstrap-resampling.
DCA for the development prediction model
The depicted DCA was used to determine whether decisions based on the predictive model had clinical applicability compared to the default strategy. Such analyses provide insight into the range of predicted risk for which the model has a high net benefit than simply either treating all (slope line) patients versus treating no (horizontal line) patient, that is to say, a prediction model is only useful at the threshold risk. The graphically DCA indicated the expected net benefit (red curve) per patient for predicting the risk of delayed extubation. Within the threshold risk range of 0%∼30%, intervention decisions based on the predictive model are clearly beneficial ().
Figure 5. The DCA shows the clinical usefulness of the nomogram. The Y-axis represents net benefit. The bold solid black line is a nomogram predicting the risk of delayed extubation. The solid grey line indicates that all patients occurred delayed extubation, while the fine solid black line indicates that no patient occurred delayed extubation. This DCA could provide a larger net benefit, with ranges of 0% to 30%. DCA: decision curve analysis .
External validation
The pre- and intraoperative characteristics in the validation cohort were described in . The prediction model indicated good discrimination in estimating the risk of delayed extubation, with a C-statistic value of 0.785 in validation cohort. The sensitivity and specificity based on AUROC curve were 89.5% and 62.0%, respectively (). Calibration plot with H-L type χ2 statistic value of 0.113 also showed good calibration in validation cohort (Supplementary Figure 2).
Discussion
The incidence of delayed extubation after thoracoscopic lung cancer surgery was 1.52%. This study identified eight independent predictors for delayed extubation. Using these eight candidates to construct a novel nomogram to estimate the decision to delayed extubation, with good C-statistic and calibration both in internal and external validation. The DCA indicated the clinical usefulness of the nomogram, suggesting that intervention decisions based on the predictive model were clearly beneficial when the threshold risk range of 0%∼30%.
Previous studies have identified some underlying predictors for delayed extubation [Citation9,Citation13–18], including age, ASA grade, body mass index (BMI), baseline lung function, operative time, case end time, extent of resection, volume of crystalloid and transfusion. By comparison, this study also demonstrated that age, BMI, FEV1/FVC, lymph nodes calcification, anaesthesia type, intraoperative transfusion, prolonged operative time and operation later than 6 p.m. were independent predictors for delayed extubation. Among these factors, lymph node calcification and anaesthesia type were rarely reported in the literature, and the latter may be an important adjustable factor to reduce the incidence of delayed extubation.
The higher rate of delayed extubation due to lymph node calcification may be possibly explained by the increased difficulty of tissue separation and dissection when thoracoscopic procedure is applied [Citation23], as well as the associated prolonged operative time and increased intraoperative complications [Citation24]. An important finding of this study was that preoperative application of TPVB, administered with 15 mL 0.5% ropivacaine through T4-T5 under ultrasound guidance, could reduce the risk of delayed extubation. The probably reason may be due to reduced intraoperative opioid dosage and improved postoperative pain control [Citation25,Citation26], thereby increasing patient tolerance to tracheal and chest tube [Citation27]. Similar to our findings, epidural analgesia usage has been established to reduce the odds of mechanical ventilation and associated delayed extubation after thoracotomy [Citation15,Citation28].
Moreover, the combination of the predictive ability of operation later than 6 P.M. as well as the lack of predictive ability of attending handoff implicated that the timing of the operation weighs more than attending handoff and may be a direct cause for delayed extubation. This is consistent with purported statements that the timing of the operation, rather than attending handoff, has an impact on postoperative complications [Citation9,Citation29,Citation30]. Adversely, Anastasian et al. reviewed the data of 37,824 patients who underwent general anaesthesia with an endotracheal tube for surgery and concluded that attending handoff was an independent risk factor for delayed extubation [Citation19]. The differences among the two studies lie in the inclusion of the population and the fact that this study did not categorize the specific time of attending handoff.
For model construction, this study was the first paper to predict delayed extubation, and all variables inserted in the predictive model were quantifiable predictors readily available to the thoracic clinicians. Besides, the nomogram can provide a visual point system to estimate the probability of delayed extubation with good discriminations after internal and external validation. Bias-corrected calibration curve showed that the model could accurately predict the occurrence of delayed extubation when the observed probability of delayed extubation was less than 15%. In the external validation cohort, this prediction model showed good calibration. Also, the depicted DCA showed that, within the threshold risk range of 0%∼30%, intervention decisions based on the predictive model are clearly beneficial.
Several limitations are among our research. First, as a monocentric retrospective study based on prospectively collected data, it has the inherent design biases. Second, although the prediction model demonstrated good efficacy in both internal and external validation in this study, external validation in a multicentre setting was still needed. Third, whether the four adjustable predictors identified in this study, especially the usage of TPVB, can reduce the occurrence of delayed extubation after surgery still needs to be verified by prospective randomized trials.
Conclusions
By reviewing 12,392 patients who underwent thoracoscopic lung cancer surgery, this cohort study identified eight independent predictors for delayed extubation, among which lymph node calcification and anaesthesia type were not commonly reported. Using these eight candidates, we constructed a novel nomogram, which can reliably identify patients at high risk for the decision to delayed extubation, with good performance in both internal and external validation. Optimizing four modifiable factors including BMI, FEV1/FVC, TPVB usage and operation later than 6 p.m. may reduce the risk of delayed extubation.
Author contributions
CY Tong performed a literature review and the statistical analysis. JJ Zheng and JX Wu were responsible for the conception and design of the study. CY Tong and Q Miao performed data collection and database management. CY Tong drafted the manuscript. CY Tong, JJ Zheng and JX Wu contributed significantly to manuscript correction and finalization. All authors contributed to the article and approved the submitted version.
Supplemental Material
Download MS Word (160.3 KB)Acknowledgements
Our research team would like to thank Professor Liu for Statistical Analysis in Shanghai Chest Hospital, Shanghai, China, for their involvement and support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Our research team could provide original data under reasonable request and with permission from Shanghai Chest Hospital.
Additional information
Funding
References
- Cook TM, Scott S, Mihai R. Litigation related to airway and respiratory complications of anaesthesia: an analysis of claims against the NHS in England 1995-2007. Anaesthesia. 2010;65(6):556–563.
- Cook TM, Woodall N, Frerk C. Fourth national audit project. Major complications of airway management in the UK: results of the fourth national audit project of the royal college of anaesthetists and the difficult airway society. Part 1: anaesthesia. Br J Anaesth. 2011;106(5):617–631.
- Popat M, Mitchell V, Dravid R, et al. Difficult airway society guidelines for the management of tracheal extubation. Anaesthesia. 2012;67(3):318–340.
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists task force on management of the difficult airway. Anesthesiology. 2013;118(2):251–270.
- Anastasian ZH, Gaudet JG, Levitt LC, et al. Factors that correlate with the decision to delay extubation after multilevel prone spine surgery. J Neurosurg Anesthesiol. 2014;26(2):167–171.
- Hawkins DB. Glottic and subglottic stenosis from endotracheal intubation. Laryngoscope. 1977;87(3):339–346.
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388–416.
- Barker J, Martino R, Reichardt B, et al. Incidence and impact of dysphagia in patients receiving prolonged endotracheal intubation after cardiac surgery. Can J Surg. 2009;52(2):119–124.
- Gal J, Hunter S, Reich D, et al. Delayed extubation in spine surgery is associated with increased postoperative complications and hospital episode-based resource utilization. J Clin Anesth. 2022;77:110636.
- Krist AH, Davidson KW, Mangione CM, et al. Screening for lung cancer: US preventive services task force recommendation statement. JAMA. 2021;325(10):962–970.
- Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg. 2015;121(2):302–318.
- Kwon ST, Zhao L, Reddy RM, et al. Evaluation of acute and chronic pain outcomes after robotic, video-assisted thoracoscopic surgery, or open anatomic pulmonary resection. J Thorac Cardiovasc Surg. 2017;154(2):652.e1–659.e1.
- Cislaghi F, Condemi AM, Corona A. Predictors of prolonged mechanical ventilation in a cohort of 5123 cardiac surgical patients. Eur J Anaesthesiol. 2009;26(5):396–403.
- Varghese J, Kutty S, Abdullah I, et al. Preoperative and intraoperative predictive factors of immediate extubation after neonatal cardiac surgery. Ann Thorac Surg. 2016;102(5):1588–1595.
- Cywinski JB, Xu M, Sessler DI, et al. Predictors of prolonged postoperative endotracheal intubation in patients undergoing thoracotomy for lung resection. J Cardiothorac Vasc Anesth. 2009;23(6):766–769.
- Buhl LK, Mueller AL, Boone MD, et al. Risk factors for delayed extubation following high posterior cervical and occipital fusion. J Neurosurg Anesthesiol. 2022;34(1):64–68.
- Xu Y, Zuo Y, Zhou L, et al. Extubation in the operating room results in fewer composite mechanical ventilation-related adverse outcomes in patients after liver transplantation: a retrospective cohort study. BMC Anesthesiol. 2021;21(1):286.
- Vannucci A, Riordan IR, Prifti K, et al. Prolonged time to extubation after general anesthesia is associated with early escalation of care: a retrospective observational study. Eur J Anaesthesiol. 2021;38(5):494–504.
- Anastasian ZH, Kim M, Heyer EJ, et al. Attending handoff is correlated with the decision to delay extubation after surgery. Anesth Analg. 2016;122(3):758–764.
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800–804.
- Chen C, Zhang X, Gu C, et al. Surgery performed at night by continuously working surgeons contributes to a higher incidence of intraoperative complications in video-assisted thoracoscopic pulmonary resection: a large monocentric retrospective study. Eur J Cardiothorac Surg. 2020;57(3):447–454.
- Van Calster B, Wynants L, Verbeek JFM, et al. Reporting and interpreting decision curve analysis: a guide for investigators. Eur Urol. 2018;74(6):796–804.
- Li Y, Wang J. Analysis of lymph node impact on conversion of complete thoracoscopic lobectomy to open thoracotomy. Thorac Cancer. 2015;6(6):704–708.
- Tong C, Li T, Huang C, et al. Risk factors and impact of conversion to thoracotomy from 20,565 cases of thoracoscopic lung surgery. Ann Thorac Surg. 2020;109(5):1522–1529.
- Albi-Feldzer A, Dureau S, Ghimouz A, et al. Preoperative paravertebral block and chronic pain after breast cancer surgery: a double-blind randomized trial. Anesthesiology. 2021;135(6):1091–1103.
- Jakuscheit A, Weth J, Lichtner G, et al. Intraoperative monitoring of analgesia using nociceptive reflexes correlates with delayed extubation and immediate postoperative pain: a prospective observational study. Eur J Anaesthesiol. 2017;34(5):297–305.
- Zhang W, Cong X, Zhang L, et al. Effects of thoracic nerve block on perioperative lung injury, immune function, and recovery after thoracic surgery. Clin Transl Med. 2020;10(3):e38.
- Elmiro GS, Souza AH, Loyola SO, et al. Spinal anesthesia increases the frequency of extubation in the operating room and decreases the time of mechanical ventilation after cardiac surgery. Braz J Cardiovasc Surg. 2021;36(1):32–38.
- Cortegiani A, Gregoretti C, Neto AS, et al. Association between night-time surgery and occurrence of intraoperative adverse events and postoperative pulmonary complications. Br J Anaesth. 2019;122(3):361–369.
- Terekhov MA, Ehrenfeld JM, Dutton RP, et al. Intraoperative care transitions are not associated with postoperative adverse outcomes. Anesthesiology. 2016;125(4):690–699.