Abstract
Background
Obesity is associated with an increased risk of fracture in adults, but is unclear in postmenopausal women. We aim to determine the association of obesity with the risk of fracture in postmenopausal women.
Methods
PubMed, EMBASE, Cochrane Library and Web of Science were searched up to 11 April 2022 for cohort studies. And the included studies regarding the relationship between obesity with all cause of fracture in postmenopausal women were included in our meta-analysis. Data were screened and extracted independently by two reviewers. The relative risks (RR) were estimated using a random-effects model. Between-study heterogeneity was assessed using Cochran’s Q and I2 statistics.
Results
Eight cohort studies comprising 671,532 postmenopausal women and 40,172 fractures were included. Overall, the pooling analysis shows that obesity in postmenopausal women is associated with an increased risk of all-cause fracture (relative ratio (RR) = 1.18; 95% confidence interval (CI):1.09–1.28, I2 = 86.3%, p = .000). Sub-analyses for each site of fracture indicate that obesity was associated with an increased risk of vertebral fracture in postmenopausal women (RR = 1.154, 95% CI: 1.020–1.305, I2 = 94.5%, p = .023), but reduced the risk of pelvic fracture (RR = 0.575, 95% CI:0.470–0.702, I2 = 0.0%, p = .000). There is no statistically significant difference in the risk of hip and humerus fractures associated with obesity in postmenopausal women.
Conclusion
Obesity is associated with an increased risk of all-cause and vertebral fractures in postmenopausal women, but is a protective factor for pelvic fractures. Our findings suggest that postmenopausal women who regulate their weight might lower their risk of fractures.Registration: (PROSPERO: CRD42022324973)
Obesity is associated with an increased risk of all-cause and vertebral fractures in postmenopausal women.
Obesity maybe a protective factor for pelvic fractures in postmenopausal women.
Postmenopausal women should regulate their weight to prevent fractures.
KEY MESSAGES
Introduction
Obesity is a complex chronic condition that increases the risk of long-term medical complications and shortens life expectancy [Citation1]. Over the past 30 years, the worldwide prevalence of obesity has steadily increased [Citation2], becoming a major public health problem, increasing health care costs, negatively affecting physical and mental health, and being an independent risk factor for other diseases [Citation3–7]. Obesity is a risk factor for fractures at different sites in both children and adults [Citation8–12]. Overall, the relationship between obesity, bone mass, and fracture risk in different populations is a complex and rather contradictory topic, depending on many factors such as the type of fracture suffered, population, age, and obesity level [Citation13]. Especially in postmenopausal women, both obesity and weight loss are at risk of fractures, which have been reported in different observational studies, but with certain contradictions [Citation14,Citation15]. Studies have shown that obese women have higher rates of certain fracture types, such as ankle and thigh fractures, and lower rates of wrist and hip fractures, than normal-weight postmenopausal women [Citation16]. Other studies have shown that factors such as body composition, bone quality, lifestyle, daily activities and comorbidities all influence the risk of fracture in postmenopausal women [Citation17]. Obese postmenopausal women may have the higher bone density to some extent, which indicates that the association between obesity and fracture risk is more complex [Citation18]. Recently, a meta-analysis including observational studies of fracture risk for an adult with obesity was done by Turcotte et al. and published in 2021 [Citation19]. However, it is a pity that only 2 literatures were included in this meta-analysis to explore the risk of ankle fracture in obese postmenopausal women, which failed to comprehensively analyze the association of fracture in obese postmenopausal women and failed to distinguish the risk of different fracture sites. Moreover, several large prospective cohort studies [Citation20–27] have explored the risk of fracture in obese postmenopausal women, and new findings may be forthcoming. Therefore, we conducted a cohort-based meta-analysis to clarify the risk of fracture in obese postmenopausal women and subgroup the risk at different fracture sites, so as to provide prevention suggestions for clinical practice.
Methods
This study was conducted in accordance with the guidelines for the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) [Citation28]. The protocol was registered in PROSPERO (No. CRD42022324973; available at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022324973, April 20, 2022).
Search strategy
PubMed, EMBASE, Web of science, and Cochrane Library were searched without any restrictions from the databases inception to April 11, 2022. We combined the Medical Subject Headings (MESH) terms and key words in the search strategy. The brief search strategy is as follows: (‘Obesity’ OR ‘Obese’) AND (‘Fractures, Bone’ OR ‘Broken*’ OR ‘Fracture*’) AND (‘Postmenopause’ OR ‘Postmenopausal*’ OR ‘Post-Menopause’ OR ‘Post Menopause’). References of included studies and existing meta-analyses were hand-searched to avoid missing relevant studies. The detail of the search strategy is included in Appendix A.
Eligibility criteria
Included studies were required to meet the following criteria: (1) cohort studies, whether prospective or retrospective; (2) the exposed group could be patients with any type of obesity, and the control group consisted of patients without obesity. Body mass index (BMI) is the most commonly used measure of overweight and obesity in adults. World Health Organization (WHO) defines ‘overweight’ as having a BMI equal to or greater than 25, and ‘obesity’ as having a BMI equal to or greater than 30. According to the standards formulated by the WHO, patients with BMI ≥ 30 are defined as obesity in this review. (3) the risk of fractures as the outcome that expressed as an adjusted odds ratio (OR), relative risk (RR), or hazard ratio (HR). Because the adjusted RR, OR, HR can reduce the influence of confounders and the observation bias. In addition, the inclusion criteria for postmenopausal women are based on the International Classification of Diseases − 10 and are based on age and participant claims. (4) fractures should be a risk occurring naturally under observation.
Exclusion criteria
(1) conference abstracts or erratum; (2) duplicate published studies based on the same observation population; (3) incomplete data or no interested outcome.
Research selection
First, we excluded repetitive and irrelevant studies according to the title and abstract, and then read each potentially eligible full text independently to determine the study that meets the inclusion criteria. And give sufficient reasons for the excluded studies. Two reviewers (Dong-fang Meng and Peng Yu) independently screened these studies. If there is any objection, discuss with the third reviewer (Hui-ying Li) until a consensus is reached.
Data extraction
Two reviewers (Hong-fei Liu and Ji-cao De) independently performed data extraction using predesigned forms based on the guideline for data extraction for systematic reviews and meta-analysis [Citation29] and the content of the extracted data drew on previous high-quality meta-analyses [Citation30,Citation31], including the following information: first author, publication year, country, sample size, fracture number, mean follow-up years, diagnostic criteria, baseline BMI, age, obesity type, fracture type, and confounders adjusted.
Risk-of-bias assessment
We used the Newcastle Ottawa Quality Assessment Scale (NOS) to evaluate the methodological quality of the included cohort studies. NOS assessed the quality of the included studies from three dimensions: selection, comparison and results. The score ranges from 0 to 9, and the higher the score, the higher the quality. NOS score equals or higher than 7, 4–6 and 0–3 represent high, medium and low quality respectively.
Statistical analysis
The Stata 14.0 software was used to conduct the data analysis. We expressed results as RRs with 95% confidence intervals (CIs) and we chose each study’s most fully adjusted results for analysis. If a study provided HR instead of RR, we used the formula (RR = (1 – eHR * ln (1 − r))/r; r: the fracture rate) to covert HR to RR [Citation32]. If the included studies provided OR instead of RR, if the risk of fracture was less than 20%, we interpreted the OR as RR; otherwise, we used generic inverse variance to calculate pooled RR [Citation33]. The incidence of fracture in the original trial included in this study is less than 20%, so these data are not converted. We assessed heterogeneity using the chi-square test and the I2 value, p < .1 or I2>50% was considered that heterogeneity was great and a random-effects model was adopted. Otherwise, a fixed-effect model was employed. The sensitivity analysis was performed to verify the robustness of the overall results and to explore sources of heterogeneity. Subgroup analysis was conducted for the location of fractures in obesity. Finally, funnel plots and egger’s regression test were used to assess the publication bias.
Results
Literature search
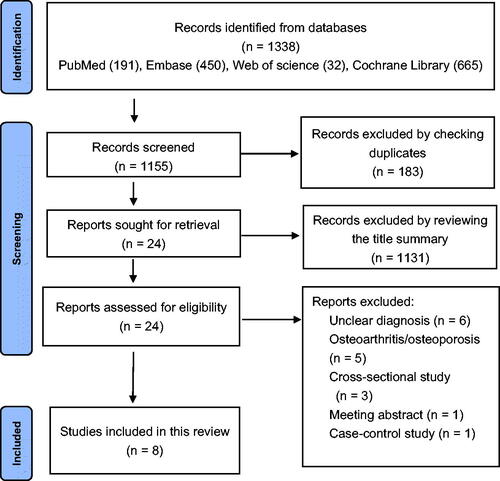
A total of 1338 records were found through electronic search, and 1155 records remained after adjusting duplicates. After that, 1131 records were discarded because, after reviewing the title and abstract, these studies clearly did not meet the inclusion criteria. The full texts of the remaining 24 records were reviewed in more detail. Finally, eight cohort studies were included in this meta-analysis [Citation20–27]. The detail of the selection process is presented in .
Study characteristics
The included cohort studies [Citation20–27] were published between 2009 and 2022 from 7 countries, involving Europe, and Asia, with the largest number of studies from Asia. A total of 671,532 postmenopausal women were enrolled, with a maximum sample size of 383,498 [Citation22] and a minimum sample size of 362 [Citation26], and a total of 40,172 fractures were diagnosed. The mean follow-up time ranged from 2.7 to 25 years. The diagnosis of obesity mainly refers to WHO BMI categories, and the diagnosis of fracture site mainly refers to the International Classification of Diseases (ICD) and confounding factors such as age, bone mineral density, and type of treatment were well controlled. The main characteristics of the included trials are shown in .
Table 1. Basic characteristics of the included cohorts.
Quality assessment
The NOS scale was used to assess the quality of the included studies, and the scores are shown in . 3 cohorts had a score of ≥ 7 and were classified as high quality, 4 cohorts had a score of 6 and 1 cohort had a score of 5 were classified as moderate quality.
Obesity and risk of all-cause fracture in postmenopausal women
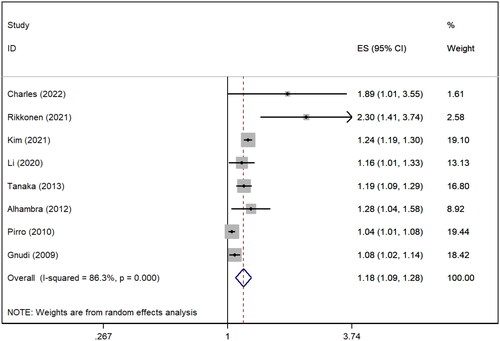
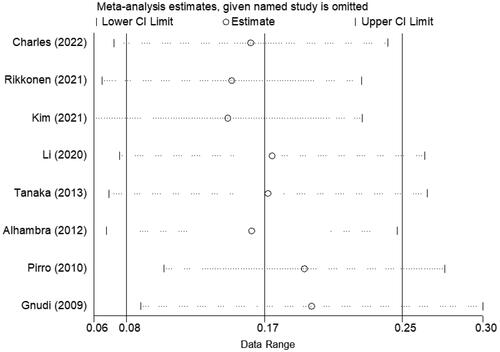
All included studies [Citation20–27] explored the relationship between obesity and the risk of all-cause fracture. The pooling analysis shows that obesity disorder in postmenopausal women is associated with an increased risk of all-cause fracture (RR = 1.18; 95% CI:1.09–1.28; I2 = 86.3%, Z = 3.89, p = .000). Since I2 was greater than 50%, the random effect model was used for meta-analysis, and sensitivity analysis was conducted to explore the source of heterogeneity. The result of the sensitivity analysis showed that none of the included cohort studies had reversed the pooled-effect size, which means that the results of this meta-analysis is robust ( and ).
Subgroup analysis
Subgroup analysis was performed according to different fracture sites, the most clinically concerned fracture sites included hip fracture, vertebral fracture, pelvic fractures, humerus fracture. Three cohort studies reported the risk of hip fractures due to obesity in postmenopausal women (RR = 1.031; 95% CI:0.780–1.363; I2 = 91.0%, p = .830), but the differences were not statistically significant. Three cohort studies have reported the risk of vertebral fracture caused by obesity in postmenopausal women (RR = 1.154; 95% CI:1.020–1.305; I2 = 94.5%, p = .023), suggesting that obesity is an important risk factor of vertebral fracture in postmenopausal women. The risk of pelvic fractures for postmenopausal women was reported in two cohort studies (RR = 0.575; 95% CI:0.470–0.702; I2 = 0.0%, p = .000), suggesting that obesity was an important protective factor for pelvic fractures in postmenopausal women. Two cohort studies reported the risk of humerus fracture due to obesity in postmenopausal women (RR = 1.139; 95% CI:0.972–1.334; I2 = 58.9%, p = .107), but the differences were not statistically significant. The details and the included trials are shown in .
Table 2. Subgroup analysis for the risk of fracture caused by obesity.
Discussion
This meta-analysis comprehensively reviewed the risk fracture in postmenopausal women with obesity compared with non-obesity from cohort studies. We found that obesity is associated with an increased risk of all-cause and vertebral fractures in postmenopausal women, but is a protective factor for pelvic fractures. There is no statistically significant difference in the risk of hip and humerus fractures associated with obesity in postmenopausal women.
Several previous meta-analyses on a similar topic have been published since 2013 to 2021 [Citation12,Citation19,Citation34,Citation35]. Two of them evaluated the association between obesity and the risk of fracture in adults [Citation19,Citation34]. These meta-analyses consistently found adults with obesity compared with the reference group had a significantly decreased risk of hip fracture. In particular, obese women had a 25%–30% lower risk of hip fracture, but our meta-analysis, which included three high-quality cohort studies [Citation21,Citation25,Citation27], found no statistical difference in the risk of hip fracture in obese postmenopausal women compared with normal-weight women. This may be related to the fact that our meta-analysis only focused on postmenopausal women, a special population. In addition, two meta-analyses [Citation12,Citation34] explored the relationship between abdominal obesity (defined by various waist-to-hip ratios) and the risk of hip fracture in patients over 40 years old and found that abdominal obesity was positively correlated with the risk of hip fracture. However, it is a small pity that the risk of hip fracture in obese postmenopausal women was not investigated separately. Previous reviews have focused on the relationship between adult obesity and the risk of hip fracture, but there are few studies on the risk of all-cause fracture in obese postmenopausal women. The meta-analysis conducted by Turcotte et al. summarized the results of two observational studies and found that postmenopausal obese women had a 60% higher risk of ankle fracture than non-obese women. This is consistent with our findings that obese postmenopausal women are associated with an increased risk of all-cause fractures. A recent cross-sectional study [Citation36] investigated the relationship between body mass index and fracture in postmenopausal women. After adjusting for many confounding factors, it was found that the risk of all-cause fracture in obese postmenopausal women was 3.33 times higher than that in normal controls, which was consistent with our findings. In summary, our meta-analysis further confirmed that obesity is the risk of all-cause fractures in postmenopausal women, but some differences should also be noted. Firstly, our meta-analysis also focused on several fracture types most concerned in the clinic, including hip fracture, vertebral fracture, pelvic fracture and humerus fracture. In addition to hip fracture, previous studies paid little attention to the risk of vertebral fracture, pelvic fracture and humerus fracture. However, our results suggest that obese postmenopausal women will increase the risk of vertebral fractures and reduce the risk of pelvic fractures, which may provide a new perspective for clinical prevention and treatment. Secondly, in order to reduce heterogeneity and provide more reliable conclusions, we analyzed the results of prospective cohort studies. Through the summary analysis of 671,532 postmenopausal women and 40,172 fracture cases in 8 cohorts, the results of large samples and high-quality evidence further confirmed the conclusion of previous studies that obesity is the risk of fracture in postmenopausal women.
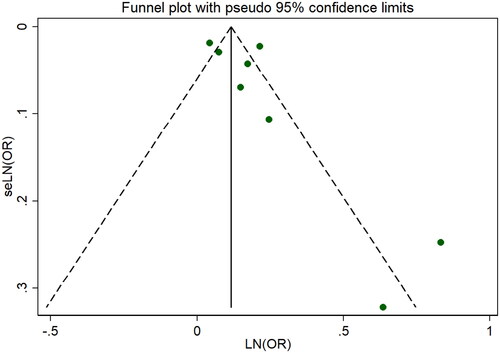
The advantage of this meta-analysis is that it conforms to the latest PRISMA 2020 statement, carries out prospective protocol registration on PROSPERO, and includes the largest sample size focusing on the risk of fracture in obese postmenopausal women. These scientific steps and feasible programs provide a reliable basis for clinical prevention to a certain extent. Our meta-analysis also has some limitations that may affect the generalization of the results. Firstly, it is difficult to rule out publication bias because our meta-analysis included only eight cohort studies. But fortunately, it passed egger’s test and there was no statistical bias. Secondly, due to the diversity of fracture sites, the number of all caused fractures and the number of specify types fracture in postmenopausal women clinically, it is difficult to completely and comprehensively summarize all fracture types and location characteristics only through the summary and analysis of cohort studies, which needs further observation and exploration.
Conclusion
The findings of this systematic review and meta-analysis suggest that obesity is associated with an increased risk of all-cause and vertebral fractures in postmenopausal women, and is a protective factor for pelvic fractures. Further studies are needed to assess the risk of other fracture sites in menopausal women with obesity.
Author contributions
Hong-fei Liu and Hui-ying Li are responsible for the study concept and design. Literature searching: Dong-fang Meng. Selection of studies: Hong-fei Liu, Peng Yu, Ji-cao De. Extraction of data: Hong-fei Liu, Dong-fang Meng, Hui-ying Li. Quality assessment: Peng Yu, Ji-cao De, Hui-ying Li. Analysed the data: Hong-fei Liu, Dong-fang Meng. Wrote the first draft of the manuscript: Hong-fei Liu, Dong-fang Meng. All authors read and approved the final manuscript.
Acknowledgments
We would like to thank the associate editor and the reviewers for their useful feedback that improved this paper.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data generated or analyzed during the present study are included in this published article.
Additional information
Funding
References
- Wharton S, Lau DCW, Vallis M, et al. Obesity in adults: a clinical practice guideline. CMAJ. 2020;192(31):1–9.
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390(10113):2627–2642.
- Ebong IA, Wilson MD, Appiah D, et al. Relationship between age at menopause, obesity, and incident heart failure: the atherosclerosis risk in communities study. J Am Heart Assoc. 2022;11:e24461.
- Otto CM. Heartbeat: hypertension risk is higher when obesity onset occurs earlier in adult life. Heart. 2022;108(9):661–663.
- Sun M, Bjørge T, Teleka S, et al. Interaction of leisure-time physical activity with body mass index on the risk of obesity-related cancers: a pooled study. Int J Cancer. 2022;151:859–868.
- Salem V, Alhusseini N, Abdul RH, et al. Prevalence, risk factors, and interventions for obesity in Saudi Arabia: a systematic review. Obes Rev. 2022;23:e13448.
- Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
- Amin RM, Raad M, Rao SS, et al. Survival bias may explain the appearance of the obesity paradox in hip fracture patients. Osteoporos Int. 2021;32(12):2555–2562.
- Khalid SI, Omotosho PA, Spagnoli A, et al. Association of bariatric surgery with risk of fracture in patients with severe obesity. JAMA Netw Open. 2020;3(6):e207419.
- Lane JC, Butler KL, Poveda-Marina JL, et al. Preschool obesity is associated with an increased risk of childhood fracture: a longitudinal cohort study of 466,997 children and up to 11 years of follow-up in Catalonia, Spain. J Bone Miner Res. 2020;35(6):1022–1030.
- Zhang T, Lary CW, Zullo AR, et al. Post-Hip fracture mortality in nursing home residents by obesity status. J Am Geriatr Soc. 2019;67(9):1983–1985.
- Sadeghi O, Saneei P, Nasiri M, et al. Abdominal obesity and risk of hip fracture: a systematic review and meta-analysis of prospective studies. Adv Nutr. 2017;8(5):728–738.
- Sogaard AJ, Holvik K, Omsland TK, et al. Abdominal obesity increases the risk of hip fracture. A population-based study of 43,000 women and men aged 60–79 years followed for 8 years. Cohort of Norway. J Intern Med. 2015;277(3):306–317.
- Compston JE, Wyman A, Fitzgerald G, et al. Increase in fracture risk following unintentional weight loss in postmenopausal women: the global longitudinal study of osteoporosis in women. J Bone Miner Res. 2016;31(7):1466–1472.
- Armstrong MEG, Spencer EA, Cairns BJ, et al. Body mass index and physical activity in relation to the incidence of hip fracture in postmenopausal women. J Bone Miner Res. 2011;26(6):1330–1338.
- Compston JE, Watts NB, Chapurlat R, et al. Obesity is not protective against fracture in postmenopausal women: GLOW. Am J Med. 2011;124(11):1043–1050.
- Feskanich D, Willett W, Colditz G. Walking and leisure-time activity and risk of hip fracture in postmenopausal women. JAMA. 2002;288(18):2300–2306.
- Crandall CJ, Yildiz VO, Wactawski-Wende J, et al. Postmenopausal weight change and incidence of fracture: post hoc findings from women’s health initiative observational study and clinical trials. BMJ. 2015;350:h25.
- Turcotte A-F, O’Connor S, Morin SN, et al. Association between obesity and risk of fracture, bone mineral density and bone quality in adults: a systematic review and meta-analysis. PLOS One. 2021;16(6):e252487.
- Charles A, Mugisha A, Iconaru L, et al. Distribution of fracture sites in postmenopausal overweight and obese women: the FRISBEE study. Calcif Tissue Int. 2022;111(1):29–34.
- Rikkonen T, Sund R, Sirola J, et al. Obesity is associated with early hip fracture risk in postmenopausal women: a 25-year follow-up. Osteoporos Int. 2021;32(4):769–777.
- Kim H, Lee C, Nam MJ, et al. Association between body composite indices and vertebral fractures in pre and postmenopausal women in Korea. PLoS One. 2021;16(8):e0254755.
- Li G, Compston JE, Leslie WD, et al. Relationship between obesity and risk of major osteoporotic fracture in postmenopausal women: taking frailty into consideration. J Bone Miner Res. 2020;35(12):2355–2362.
- Tanaka S, Kuroda T, Saito M, et al. Overweight/obesity and underweight are both risk factors for osteoporotic fractures at different sites in Japanese postmenopausal women. Osteoporos Int. 2013;24(1):69–76.
- Prieto-Alhambra D, Premaor MO, Fina AF, et al. The association between fracture and obesity is site-dependent: a population-based study in postmenopausal women. J Bone Miner Res. 2012;27(2):294–300.
- Pirro M, Fabbriciani G, Leli C, et al. High weight or body mass index increase the risk of vertebral fractures in postmenopausal osteoporotic women. J Bone Miner Metab. 2010;28(1):88–93.
- Gnudi S, Sitta E, Lisi L. Relationship of body mass index with main limb fragility fractures in postmenopausal women. J Bone Miner Metab. 2009;27(4):479–484.
- Page MJ, Mckenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- Taylor KS, Mahtani KR, Aronson JK. Summarising good practice guidelines for data extraction for systematic reviews and meta-analysis. BMJ Evid Based Med. 2021;26(3):88–90.
- Wang YB, Ma R, Wang ZB, et al. Transcatheter arterial chemoembolization in combination with high-intensity focused ultrasound for intermediate and advanced hepatocellular carcinoma: a meta-analysis. Front Oncol. 2022;12:797349.
- Lei S, Li X, Zhao H, et al. Risk of dementia or cognitive impairment in sepsis survivals: a systematic review and meta-analysis. Front Aging Neurosci. 2022;14:839472.
- Shor E, Roelfs D, Vang ZM. The “hispanic mortality paradox” revisited: meta-analysis and meta-regression of life-course differentials in Latin American and Caribbean immigrants’ mortality. Soc Sci Med. 2017;186:20–33.
- Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. Chichester (UK): John Wiley & Sons; 2011.
- Li X, Gong X, Jiang W. Abdominal obesity and risk of hip fracture: a meta-analysis of prospective studies. Osteoporos Int. 2017;28(10):2747–2757.
- Tang X, Liu G, Kang J, et al. Obesity and risk of hip fracture in adults: a meta-analysis of prospective cohort studies. PLOS One. 2013;8(4):e55077.
- Kim J, Lee S, Kim SS, et al. Association between body mass index and fragility fracture in postmenopausal women: a cross-sectional study using Korean National Health and Nutrition Examination Survey 2008–2009 (KNHANES IV). BMC Womens Health. 2021;21(1):60.
Appendix A:
The retrieval strategies and retrieval results of each database are shown in
Table A1. PubMed.
Table A2. Embase.
Table A3. Cochran Library.
Table A4. Web of science.