Abstract
Objectives
The coronavirus disease-19 (COVID-19) increased the already heavy workload in the pulmonary and respiratory departments, which therefore possibly increased the prevalence of burnout among pulmonologists or respiratory therapists. We aimed to compare the differences in burnout among pulmonologists or respiratory therapists pre- and post-COVID-19 by doing a systematic review with meta-analysis.
Methods
We searched pulmonologist, or pulmonary, or respiratory, and burnout up to 29 January 2023 in six databases. We included studies investigating pulmonologists or respiratory therapists and reporting the prevalence of burnout among them. The risk of bias was assessed by a tool for prevalence studies. The overall prevalence of burnout was pooled.
Results
A total of 2859 records were identified and 16 studies were included in the final analysis. The included studies reported 3610 responding individuals and 2336 burnouts. The pooled prevalence of burnout was 61.7% (95% confidence interval (CI), 48.6–73.2%; I2 = 96.3%). The pooled prevalence of burnout during COVID-19 was significantly higher than it was prior to the outbreak (68.4% vs. 41.6%, p = .01). The result of the meta-regression revealed that COVID-19 coverage was significantly associated with the prevalence of burnout (p = .04).
Conclusions
Burnout was widely prevalent among pulmonologists or respiratory therapists and increasingly perceived during COVID-19. Therefore, interventions were needed to reduce burnout in this specialty.
The coronavirus disease-19 increased the already heavy workload in the pulmonary and respiratory departments.
Burnout was widely prevalent among pulmonologists or respiratory therapists and increasingly perceived during COVID-19.
KEY MESSASGES
Introduction
The coronavirus disease-19 (COVID-19) has been declared an end as a global health emergency in May 2023 [Citation1]. However, with 767 million confirmed cases and 6.9 million deaths as of writing, the disease remains a health threat to the public [Citation2]. Life is returning to what it is like before COVID-19 with some vaccines and anti-virus drugs, but a great number of health workers are still working in the frontline and fighting against local surges in cases and deaths. The outbreak once left no room for mental preparedness. COVID-19 increases the workload and stress placed on health workers, which has an impact on their physical and mental health, including professional burnout, depression and anxiety [Citation3,Citation4]. Burnout is a work-related syndrome of emotional exhaustion (EE), depersonalization (DP) and a reduced perception of personal accomplishment (PA) [Citation5]. Multiple studies have indicated that during the COVID‐19 pandemic, nurses [Citation6], physicians [Citation7], surgeons [Citation8], residents [Citation9] and medical students all experience high levels of burnout [Citation10]. Significant differences were noticed across various specialities [Citation11]. The disease causes respiratory-tracts-related symptoms increasing the already heavy workload in the pulmonary and respiratory departments. In 2015, the prevalence was reported as high as 47% among pulmonary medicine [Citation12]. Several studies investigated the burnout of pulmonary physicians [Citation13] and respiratory therapists during COVID-19 [Citation14,Citation15]. They observed that burnout was widely perceived and levelled up during the pandemic. However, there have not been studies to summarize the prevalence of burnout among pulmonologists and respiratory therapists. Therefore, we aimed to report the overall prevalence by conducting a systematic review and performing a meta-analysis.
Methods
We followed the PRISMA 2020 guideline to report this study [Citation16].
Database search
We searched pulmonologist, or pulmonary, or respiratory, and burnout up to 29 January 2023 in the following databases: PubMed, EMBASE, PsycINFO, Cochrane Central Register of Controlled Trials (CENTRAL), Scopus and Web of Science. The search strategy for all databases was provided in the supplementary material. We also screened the references of related publications to identify additional relevant studies. Two researchers independently searched the databases.
Inclusion criteria
The inclusion criteria of eligible studies were as follows: studies investigating the population of pulmonologists or respiratory therapists; studies reporting the prevalence of burnout among the aforementioned population. Studies were excluded if they (1) failed to state the number of burnouts among pulmonologists or respiratory therapists; (2) were qualitative studies without reporting the prevalence of burnout; (3) only investigated the interventions against burnout without reporting the baseline prevalence of burnout; and (4) were case reports, reviews, comments, editorials, corrections, replies, notes or book chapters.
Study selection
EndNote 20 (Clarivate PLC, Jersey, UK) was used to manage the records imported from each database. Duplicated publications were initially removed by the same DOI number and then verified manually. Studies were first screened by reviewing the titles and abstracts. The possibly eligible ones subsequently underwent full-text reviews. The selection was independently conducted by the two reviewers (Z.W. and X.B.). A third reviewer (L.W.) was involved in the disagreements of the included studies that could not be resolved through discussion.
Data extraction
Based on the purpose of the study, the following information was extracted: first author, publication year, study setting, COVID-19 experience, centres, study design, study period and survey response rate. The following information was extracted from the investigated population: specialty, clinical level, burnout measure instrument, the total number of respondents, demographic characteristics of respondents (sex, age, marriage and COVID-19 care), number of burnouts, the prevalence of burnout, risk factors of burnout and their odds ratios. Two reviewers (Z.W. and X.B.) independently collected data using a standard collection form.
Risk of bias assessment
The risk of bias in included studies was assessed by a tool proposed by Hoy et al. for prevalence studies [Citation17]. This tool consists of 10 items, one point for each, addressing bias of selection, nonresponse, measurement and analysis. The risk of bias was graded as low (score 0–3), moderate [Citation4–6] and high [Citation7–10]. Certainty was graded using a variation version of the Grading of Recommendations Assessment, Development and Evaluation (GRADE) for environmental and occupational health [Citation18].
Statistical analysis
R 4.2.1 (R Foundation, Vienna, Austria) was used for all statistical analyses. The prevalence of burnout among pulmonologists and respiratory therapists was pooled by using logit transformation and presented in a forest plot. No study was excluded because all studies included reported their prevalence of burnout. Heterogeneity was evaluated by measure of I2 and considered significant when I2 ≥ 50%. When there was significant heterogeneity between studies, the random-effects model was used for pooling; otherwise, the fixed-effects model was used. The generalized linear mixed model and the logit transformation were used in the meta-analysis of proportions. The subgroup analysis of burnout prevalence was performed based on their COVID-19 coverage, survey respondent rate, respondent size, measurement instrument and department. A meta-regression was conducted to determine if there were any independent risk factors for burnout prevalence. The difference was considered significant when a two-sided p value was less than .05. Influence analysis by leaving out one study at a time was performed to the pooled prevalence to assess its robustness.
Results
Included studies
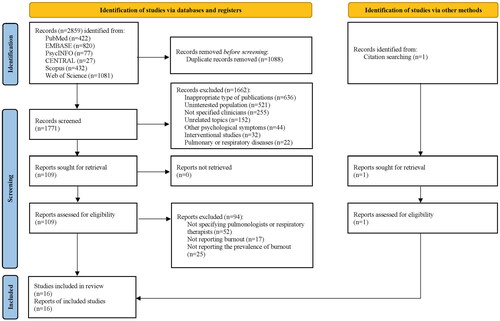
A total of 2859 records were identified from PubMed (n = 422), EMBASE (n = 820), PsycINFO (n = 77), CENTRAL (n = 27), Scopus (n = 432) and Web of Science (n = 1081). There were 1088 duplicates removed. The remaining 1771 records went through title-and-abstract reviews. A total of 1662 records were excluded owing to the following reasons: inappropriate type of publications (n = 636), uninterested population (n = 521), unspecified clinicians (n = 255), unrelated topics (n = 152), other psychological symptoms (n = 44), interventional studies (n = 32) and pulmonary or respiratory diseases (n = 22). Therefore, 109 records were considered eligible when evaluated by full-text reviews. Ninety-four records were excluded for the following reasons: an unspecified number of pulmonologists or respiratory therapists (n = 52), not reporting burnout (n = 17) or not reporting the prevalence of burnout (n = 25). One additional paper was found by screening the reference lists of the included studies. Therefore, the final analysis comprised 16 studies () [Citation14,Citation19–33]. Risk of bias was assessed as low in 13 studies, and moderate in the other three studies (Supplementary Table 1).
Figure 1. PRISMA flow of study selection. A total of 2859 records were identified from PubMed (n = 422), EMBASE (n = 820), PsycINFO (n = 77), CENTRAL (n = 27), Scopus (n = 432) and Web of Science (n = 1081). There were 1088 duplicates removed. The remaining 1771 records went through title-and-abstract reviews. We excluded 1662 records due to reasons presented in the figure. Therefore, 109 records were further evaluated by full-text reviews. Ninety-four were excluded because of reasons in the above column. One additional paper was found by screening the reference lists of the included studies. Thus, 16 studies were included in the final analysis.
The 16 studies were conducted in eight countries, including the United States (n = 6), Saudi Arabia (n = 4), Qatar, Italy, China, the United Kingdom, Brazil and Mexico (n = 1 for each). A cross-sectional design was used for 15 investigations, whereas a longitudinal analysis was used in the other study. The cross-sections spanned from 2009 to 2021 with 12 studies covering the outbreak of COVID-19. The median response rate was 67.6% (range: 36.4–96.2%). Six studies had respondent sizes <100, whereas the other 10 studies had sizes >100. While the nine studies were from multiple centres, the other six were from single sites. Twelve studies investigated respiratory therapists (students), while the other four reported fellows, physicians (n = 2) and residents. Five studies focused on the intensive care unit (ICU), six on the pulmonary and respiratory medicine departments, and the remaining five were from unspecified departments. This information is presented in .
Table 1. Information of the included studies (n = 16).
Respondent characteristics
The included studies reported a total of 3610 responding individuals, with nine studies presenting the demographic characteristics of their respondent population (n = 2100, 58%) [Citation20, Citation22–24, Citation26, Citation29–31,Citation33]. The reported mean or median ages ranged from 20 to 40 years old. The pooled percentage of males was 46.8% (95% confidence interval (CI), 34.4–60.0%; I2 = 95.7%). The pooled percentage of married individuals was 52.7% (95% CI, 26.1–77.9%; I2 = 98.7%). Additionally, the studies reported features of the region, workload, years of experience, education level, night shifts and others.
Prevalence of burnout
Most studies (n = 10) used the Maslach Burnout Inventory (MBI) to measure burnout. One study used the MBI two-item, an adapted tool from MBI [Citation24]. The instruments of the other five studies are listed in , including three tools not available owing to restricted access to their full texts. The 10 studies varied in their definitions and grading cutoffs of burnout despite employing the same tool, MBI, to evaluate burnout (). Collectively, six studies defined burnout as the combination of high EE, high DP and low PA. Another two studies defined less strictly as fulfilling one of the above three manifestations. The other two did not give the exact definition of burnout; however, they presented the respective number of burnouts concerning the three aspects.
Table 2. The measure, definition and prevalence of burnout of the included studies (n = 16).
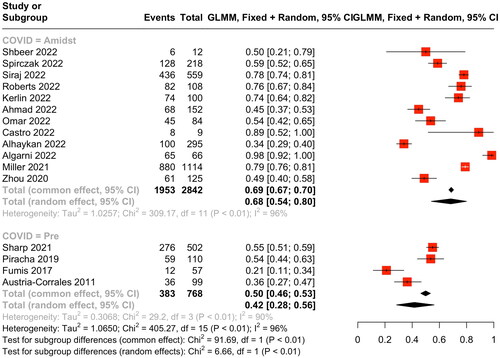
The included studies reported 2336 burnouts. The pooled prevalence of burnout was 61.7% (95% CI, 48.6–73.2%; I2 = 96.3%). Influence analysis revealed that the value was not significantly changed by omitting one study at a time. The pooled prevalence was 58.5% (95% CI, 39.5–75.2%; I2 = 95.5%) if only included studies using the MBI instrument and 60.9% (95% CI, 46.0–74.0%; I2 = 94.8%) if only included studies in full text. The subgroup analysis revealed that experiencing COVID-19 was significantly associated with burnout prevalence. The pooled prevalence of burnout during COVID-19 was significantly higher than it was prior to the outbreak (68.4% vs. 41.6%, p = .01, ). The subgroup analysis showed subgroups separated by the sample size (<100 vs. ≥100), the survey response rate (>50% vs. ≥50%), the measurement instrument (MBI vs. non-MBI) and the department (ICU vs. non-ICU) were not significantly different in the prevalence of burnout (p = .65, .83, .50 and .37, respectively). The outcome of the meta-regression revealed that COVID-19 was significantly associated with the prevalence of burnout (p = .04). The certainty was graded as low by using adapted GRADE tool mainly because all were cross-sectional studies.
Figure 2. Forest plot of the overall prevalence of burnout. The included studies reported a total of 3610 responding individuals and 2100 burnouts. The pooled prevalence of burnout was 61.7% (95% CI, 48.6–73.2%; I2 = 96.3%). The pooled prevalence of burnout during COVID-19 was significantly higher than it was prior to the outbreak (68.4% vs. 41.6%, p = .01).
Risk factors
Eight studies reported the risk factors of burnout [Citation20, Citation23–26, Citation30, Citation31, Citation33]. Female pulmonologists or respiratory therapists tended to experience more burnout than their male counterparts [Citation20, Citation23, Citation26]. In two studies, a heavier weekly workload was reported to exacerbate burnout [Citation24, Citation26], while another study presented that the weekly workload was not significantly associated with burnout [Citation20]. The coverage system and mental health services were reported to be protective factors from burnout [Citation24]. Age, academic year and nationality were also found to be significant factors associated with burnout [Citation30, Citation31, Citation33].
Discussion
To the best of our knowledge, this study was the first meta-analysis to provide a summary of the prevalence of burnout among pulmonologists and respiratory therapists. The overall burnout prevalence was determined to be 61.7%, which was higher (68.4%) during the outbreak than it had been before (40.7%).
The level of burnout we obtained was consistent with prior reports from a more general medical population. According to a meta-analysis, the prevalence of burnout among European physicians, using a unidimensional definition, was 43.2% [Citation34], which was comparable to what we observed in the pre-COVID-19 subgroup. The prevalence during COVID-19 was approximately 67% [Citation35], which was consistent with the pooled subgroup result we reported. Furthermore, our findings suggested that there was an increase over the past 3 years, which was observed elsewhere. According to a longitudinal cohort study, burnout was more prevalent during COVID-19, with a post-peak rate being approximately 13% higher than before [Citation36]. Other studies among various demographics have reported that COVID-19 has an impact on the increase in burnout [Citation37–39].
Pulmonologists and respiratory therapists work in close relation with healthcare professionals in the ICU or critical care medicine. Both departments have long been reported to present high burnout prevalence owing to extensive workloads, mental stress, emergency burden and the complexity of patients’ conditions [Citation40–43]. The severe acute respiratory syndrome coronavirus 2 enters the respiratory tract, subsequently harming the respiratory system [Citation44]. Therefore, the likelihood of increased stress and burnout levels in several specific departments was high [Citation45]. Our findings were close to the prevalence of burnout among frontline workers in the ICU [Citation43,Citation46]. Therefore, it was possible that both daunting work stress and overwhelming pandemic together put on a heavy burden on pulmonologists and respiratory therapists to level up the perception of occupational burnout.
The extent COVID-19 contributed to burnout (if any) could not be determined. The pandemic affected practically every facet of daily life. Thus, it may have been a confounding factor that masked several important factors, such as lack of wellness resources [Citation37], shortage of personal protective equipment [Citation47] and poor leadership [Citation48]. Future individual studies could delve into the greater impact of COVID-19.
Immediate interventions are necessary to address burnout. Out of 10 pulmonologists or respiratory therapists, six to seven experience burnout. This number was not only higher than the frontline health workers during COVID-19 [Citation49], but also much higher than nurses (even working in ICU) [Citation6,Citation50]. On the other hand, there is strong evidence linking occupational burnout to clinicians’ less sustainable career development and, consequently, lowering healthcare quality [Citation51]. The high prevalence of burnout and the significant harm to healthcare organizations highlight the need for urgent interventions to improve burnout. Series of studies among Serbian health workers revealed that fostering resilience and mentalizing would be helpful to reduce burnout [Citation52–54]. Clinicians could pay more attention to their own mental status and find their own solutions towards occupational burnout. The healthcare system should also take burnout into account and facilitate clinicians to reduce burnout. It was observed that residents and trainees were more susceptible to burnout [Citation51]. In addition, COVID-19 served as an obstacle to physical skill training [Citation55]. This highlights yet another need for training programs to establish effective individual-focused or organizational strategies to reduce burnout [Citation56].
There were some limitations in our study. A reliable assessment of the prevalence of burnout among physicians was difficult owing to the inconsistency of the definition and cut-off of burnout [Citation57,Citation58]. This circumstance was also observed in our study. Few studies have reported burnout among pulmonologists, which makes further research difficult. Moreover, the participant sizes in about half of the identified studies were <100 and some studies had response rates <50%. These tend to introduce a respondent bias since burnout is self-reported [Citation59].
Conclusions
We reported that the overall prevalence of burnout among pulmonologists or respiratory therapists was as high as 61.4%, which was 68.4% during COVID-19 and 40.7% predating the pandemic. The high prevalence and the significant increase in burnout established the need for immediate interventions to reduce burnout in this specialty.
Ethical approval
Not applicable.
Consent form
Not applicable.
Author contributions
Conception and design: XB, ZW, JT and LW. Administrative support: LW and XT. Provision of study materials or patients: XB, ZW, JT and DZ. Collection and assembly of data: XB, ZW and LW. Data analysis and interpretation: DZ, XW, KS, LQ, YZ, YW, WC, WJ and XT. ZW prepared the figures and tables. Manuscript writing and reviewing: all authors. Final approval of manuscript: all authors.
Supplemental Material
Download MS Excel (9.3 KB)Supplemental Material
Download MS Excel (10.9 KB)Disclosure statement
All of us declare that we have no competing interests.
Data availability statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Additional information
Funding
References
- WHO chief declares end to COVID-19 as a global health emergency. Global perspective human stories (health). UN News; 2023.
- WHO coronavirus (COVID-19) dashboard; 2023. Available from: https://covid19whoint/
- Aymerich C, Pedruzo B, Perez JL, et al. COVID-19 pandemic effects on health worker’s mental health: systematic review and meta-analysis. Eur Psychiatry. 2022;65(1):1. doi: 10.1192/j.eurpsy.2022.1.
- Munn LT, Liu TL, Swick M, et al. Original research: well-being and resilience among health care workers during the COVID-19 pandemic: a cross-sectional study. Am J Nurs. 2021;121(8):24–9. doi: 10.1097/01.NAJ.0000767352.47699.0c.
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397.
- Galanis P, Vraka I, Fragkou D, et al. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286–3302. doi: 10.1111/jan.14839.
- Prasad K, McLoughlin C, Stillman M, et al. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: a national cross-sectional survey study. EClinicalMedicine. 2021;35:100879. doi: 10.1016/j.eclinm.2021.100879.
- Kabir T, Tan AYH, Koh FHX, et al. Burnout and professional fulfilment among surgeons during the COVID-19 pandemic. Br J Surg. 2021;108(1):e3–e5. doi: 10.1093/bjs/znaa001.
- Fadle AA, Khalifa AA, Mahran DG, et al. Burnout syndrome (BOS) among resident doctors in an Egyptian Tertiary Care University Hospital: prevalence and determinants during the COVID-19 pandemic. Int J Soc Psychiatry. 2023;69(2):396–405. doi: 10.1177/00207640221104698.
- Zis P, Artemiadis A, Bargiotas P, et al. Medical studies during the COVID-19 pandemic: the impact of digital learning on medical students’ burnout and mental health. Int J Environ Res Public Health. 2021;18(1):349.
- Firew T, Sano ED, Lee JW, et al. Protecting the front line: a cross-sectional survey analysis of the occupational factors contributing to healthcare workers’ infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open. 2020;10(10):e042752. doi: 10.1136/bmjopen-2020-042752.
- Peckman C. Physician burnout: it just keeps getting worse. Medscape; 2015.
- O’Toole J, Zaeh S, Eakin MN, et al. Balancing demands: determinants of burnout reported by fellows in pulmonary and critical care medicine. ATS Sch. 2021;2(1):108–123. doi: 10.34197/ats-scholar.2020-0097OC.
- Strickland SL, Roberts KJ, Smith BJ, et al. Burnout among respiratory therapists amid the COVID-19 pandemic. Respir Care. 2022;67(12):1578–1587. doi: 10.4187/respcare.10144.
- Stark N, Hayirli T, Bhanja A, et al. Unprecedented training: experience of residents during the COVID-19. Ann Emerg Med. 2022;79(5):488–494. doi: 10.1016/j.annemergmed.2022.01.022.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71.
- Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014.
- Morgan RL, Thayer KA, Bero L, et al. GRADE: assessing the quality of evidence in environmental and occupational health. Environ Int. 2016;92–93:611–616. doi: 10.1016/j.envint.2016.01.004.
- Shbeer A, Ageel M. Assessment of occupational burnout among intensive care unit staff in Jazan, Saudi Arabia, using the Maslach Burnout Inventory. Crit Care Res Pract. 2022;2022:1298887. doi: 10.1155/2022/1298887.
- Omar AS, Hanoura S, Labib A, et al. Burnout among respiratory therapists and perception of leadership: a cross sectional survey over eight intensive care units. J Intensive Care Med. 2022;37(12):1553–1562. doi: 10.1177/08850666221086208.
- Castro HM, Prieto MA, Muñoz AM. Prevalence of burnout in healthcare workers during the COVID-19 pandemic and associated factors. A cross-sectional study. Medicina. 2022;82(4):479–486.
- Alhaykan AEA. Exploring the relationship between burnout and supervisory support among respiratory therapists [Ph.D. thesis]. Seton Hall University; 2022.
- Algarni SS, Algihab AA, Bin Dahmash HA, et al. Burnout among respiratory therapists in a tertiary hospital in Saudi Arabia. Respir Care. 2023;68(2):228–233. doi: 10.4187/respcare.10140.
- Sharp M, Burkart KM, Adelman MH, et al. A national survey of burnout and depression among fellows training in pulmonary and critical care medicine: a special report by the Association of Pulmonary and Critical Care Medicine Program Directors. Chest. 2021;159(2):733–742. doi: 10.1016/j.chest.2020.08.2117.
- Miller AG, Roberts KJ, Smith BJ, et al. Prevalence of burnout among respiratory therapists amidst the COVID-19 pandemic. Respir Care. 2021;66(11):1639–1648. doi: 10.4187/respcare.09283.
- Zhou Y, Gu W, Tao R, et al. The impact of gender and working hours on pulmonary physician burnout. Ann Transl Med. 2020;8(18):1166. doi: 10.21037/atm-20-5827.
- Piracha S, Raza A, Niazi M, et al. A study of burnout and professional fulfilment among respiratory physicians (RP) in United Kingdom (UK). Eur Respir J. 2019;54:PA1976. doi: 10.1183/13993003.congress-2019.PA1976.
- Fumis RRL, Junqueira Amarante GA, de Fátima Nascimento A, et al. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann Intensive Care. 2017;7(1):71. doi: 10.1186/s13613-017-0293-2.
- Austria-Corrales F, Cruz-Valdés B, Herrera-Kiengelher L, et al. Burnout syndrome among medical residents during the influenza a H1N1 sanitary contingency in Mexico. Gac Med Mex. 2011;147(2):97–103.
- Spirczak A, Kaur R, Vines DL. Burnout among respiratory therapists during COVID-19 pandemic. Can J Respir Ther. 2022;58:191–198. doi: 10.29390/cjrt-2022-049.
- Siraj RA, Aldhahir AM, Alqahtani JS, et al. Burnout and resilience among respiratory therapy (RT) students during clinical training in Saudi Arabia: a nationwide cross-sectional study. Int J Environ Res Public Health. 2022;19(20):13047.
- Kerlin MP, Silvestri JA, Klaiman T, et al. Critical care clinician wellness during the COVID-19 pandemic: A longitudinal analysis. Ann Am Thorac Soc. 2022;19(2):329–331. doi: 10.1513/AnnalsATS.202105-567RL 34398722.
- Ahmad RG, Gadah YS, Yamani RA, et al. The relationship between physical activity and burnout among respiratory therapists in Jeddah city, Saudi Arabia. Can J Respir Ther. 2022;58:204–208. doi: 10.29390/cjrt-2022-029IF:NANANA.
- Hiver C, Villa A, Bellagamba G, et al. Burnout prevalence among European physicians: a systematic review and meta-analysis. Int Arch Occup Environ Health. 2022;95(1):259–273. doi: 10.1007/s00420-021-01782-z.
- Han R, Hahn E, Done SJ, et al. Resident depression and burnout during the COVID-19 pandemic: a survey of Canadian laboratory medicine trainees. Arch Pathol Lab Med. 2022;147(3):368–375.
- Kok N, van Gurp J, Teerenstra S, et al. Coronavirus disease 2019 immediately increases burnout symptoms in ICU professionals: a longitudinal cohort study. Crit Care Med. 2021;49(3):419–427. doi: 10.1097/CCM.0000000000004865.
- Coleman JR, Abdelsattar JM, Glocker RJ, et al. COVID-19 pandemic and the lived experience of surgical residents, fellows, and early-career surgeons in the American College of Surgeons. J Am Coll Surg. 2021;232(2):119–135.e20. doi: 10.1016/j.jamcollsurg.2020.09.026.
- Queiroz de Paiva Faria AR, Campos Coelho HF, Silva AB, et al. Impact of the COVID-19 pandemic on the development of burnout syndrome in frontline physicians: prevalence and associated factors. Rev Assoc Med Bras (1992). 2021;67(7):942–949. doi: 10.1590/1806-9282.20210244.
- Scatularo CE, Battioni L, Bellia S, et al. Psychophysical impact of the covid-19 pandemic on healthcare workers in Argentina. The ImPPaCTS-SAC.20 survey. Rev Argent Cardiol. 2021;89(3):196–202.
- Gualano MR, Sinigaglia T, Lo Moro G, et al. The burden of burnout among healthcare professionals of intensive care units and emergency departments during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2021;18(15):8172.
- Colville GA, Smith JG, Brierley J, et al. Coping with staff burnout and work-related posttraumatic stress in intensive care. Pediatr Crit Care Med. 2017;18(7):e267–e273. doi: 10.1097/PCC.0000000000001179.
- Pastores SM, Kvetan V, Coopersmith CM, et al. Workforce, workload, and burnout among intensivists and advanced practice providers: a narrative review. Crit Care Med. 2019;47(4):550–557. doi: 10.1097/CCM.0000000000003637.
- Hu Z, Wang H, Xie J, et al. Burnout in ICU doctors and nurses in mainland China—a national cross-sectional study. J Crit Care. 2021;62:265–270. doi: 10.1016/j.jcrc.2020.12.029.
- Harrison AG, Lin T, Wang P. Mechanisms of SARS-CoV-2 transmission and pathogenesis. Trends Immunol. 2020;41(12):1100–1115. doi: 10.1016/j.it.2020.10.004.
- Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2020. Mayo Clin Proc. 2022;97(3):491–506. doi: 10.1016/j.mayocp.2021.11.021.
- Stocchetti N, Segre G, Zanier ER, et al. Burnout in intensive care unit workers during the second wave of the COVID-19 pandemic: a single center cross-sectional Italian study. Int J Environ Res Public Health. 2021;18(11):6102.
- Leao T, Duarte G, Goncalves G. Preparedness in a public health emergency: determinants of willingness and readiness to respond in the onset of the COVID-19 pandemic. Public Health. 2022;203:43–46. doi: 10.1016/j.puhe.2021.11.021.
- Mehta AB, Lockhart S, Reed K, et al. Drivers of burnout among critical care providers: a multicenter mixed-methods study. Chest. 2022;161(5):1263–1274. doi: 10.1016/j.chest.2021.11.034.
- Zhang X, Wang J, Hao Y, et al. Prevalence and factors associated with burnout of frontline healthcare workers in fighting against the COVID-19 pandemic: evidence from China. Front Psychol. 2021;12:680614. doi: 10.3389/fpsyg.2021.680614.
- Ramírez-Elvira S, Romero-Béjar JL, Suleiman-Martos N, et al. Prevalence, risk factors and burnout levels in intensive care unit nurses: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(21):11432.
- Hodkinson A, Zhou A, Johnson J, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. 2022;378:e070442. doi: 10.1136/bmj-2022-070442.
- Safiye T, Vukčević B, Čabarkapa M. Resilience as a moderator in the relationship between burnout and subjective well-being among medical workers in Serbia during the COVID-19 pandemic. Vojnosanitetski Pregled. 2021;78(11):1207–1213.
- Safiye T, Vukčević B, Gutić M, et al. Resilience, mentalizing and burnout syndrome among healthcare workers during the COVID-19 pandemic in Serbia. Int J Environ Res Public Health. 2022;19(11):6577.
- Safiye T, Gutić M, Dubljanin J, et al. Mentalizing, resilience, and mental health status among healthcare workers during the COVID-19 pandemic: a cross-sectional study. Int J Environ Res Public Health. 2023;20(8):5594.
- Poelmann FB, Koeter T, Steinkamp PJ, et al. The immediate impact of the coronavirus disease 2019 (COVID-19) pandemic on burn-out, work-engagement, and surgical training in The Netherlands. Surgery. 2021;170(3):719–726. doi: 10.1016/j.surg.2021.02.061.
- West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi: 10.1016/S0140-6736(16)31279-X.
- Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777.
- Karuna C, Palmer V, Scott A, et al. Prevalence of burnout among GPs: a systematic review and meta-analysis. Br J Gen Pract. 2022;72(718):e316–e324. doi: 10.3399/BJGP.2021.0441.
- Guenette JP, Smith SE. Burnout: prevalence and associated factors among radiology residents in New England with comparison against United States resident physicians in other specialties. AJR Am J Roentgenol. 2017;209(1):136–141. doi: 10.2214/AJR.16.17541.

