Abstract
Purpose
To explore the incidence, risk factors, management and prognosis of systemic complications after ophthalmic surgeries.
Methods
A retrospective review of hospitalized patients undergoing ophthalmic surgeries between 2012 and 2022 at Peking Union Medical College Hospital was performed to summarize and analyse the postoperative systemic complications. Multivariate logistic and linear regression analyses were conducted to clarify the risk factors of postoperative systemic complications and factors associated with the severity of adverse events.
Results
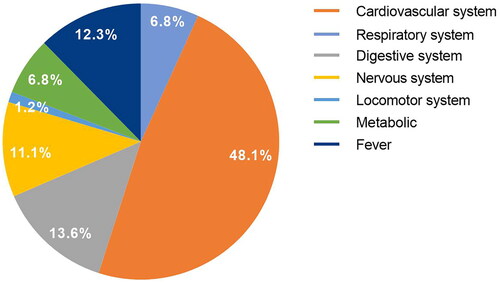
A total of 34,841 patients underwent inpatient ophthalmic surgery, among which 162 systemic complications occurred in 150 patients during postoperative hospitalization. The overall incidence rate was 0.4%, with cardiovascular events (48.1%), digestive events (13.6%) and fever (12.3%) being the leading causes. About 17.3% of the cases had conditions improved after observation, 19.1% after symptomatic treatment, 54.9% had consultation with specific intervention and 8.6% were transferred to the corresponding departments for specialized treatment. For the prognosis, 93.8% had condition improved, 5.6% chose voluntary discharge without improvement, and one patient died of respiratory failure caused by postoperative pulmonary infection. The worse ADL (activities of daily living) grading, indication of primary intraocular lymphoma or intraocular tumour, surgery of simple pars plana vitrectomy (PPV), PPV with silicone oil tamponade, PPV with gas tamponade, general anaesthesia, history of diabetes mellitus (DM), chronic heart failure and digestive system disease were the risk factors positively correlated with postoperative systemic complications (p < .05). The worse ADL grading, history of DM and respiratory system disease were also positively correlated with the severity of the adverse events (p < .05).
Conclusions
The incidence of postoperative systemic complications was low among patients undergoing ophthalmic surgery, most were mild and could be relieved after observation, symptomatic or specialist consultation. Patients with worse ADL and history of DM should be paid extra attention.
Introduction
With the rapid development of medical care and technology, the number of ophthalmic surgeries is blooming dramatically around the world. According to statistics, the number of ophthalmic inpatients in China has increased from 3.1 million in 2012 to 8.1 million in 2021 [Citation1]. The blooming number of procedures also implies a higher risk of complications, especially in elderly patients with underlying disease, and patients with diabetic retinopathy related vitreous haemorrhage or retinal detachment (RD) are also considered to have multiple comorbidities (diabetes mellitus (DM), renal failure, coronary heart disease, etc.) and more complex and severe surgical indications. Another dilemma is whether and when to perform complex preoperative examination for systemic comorbidities and the difficult balance to achieve among safe ophthalmic surgery, unnecessary medical resources cost, and reduced risk of postoperative systemic complications, especially in the elderly [Citation2–5]. These remind us that greater attention should be paid to understanding and managing perioperative systemic complications and that more comprehensive preoperative evaluation and thoughtful postoperative clinical care could help us in providing greater medical resources and reducing the risk of unsatisfactory surgical prognosis.
Current studies focused on whether routine preoperative examination could reduce the risk of postoperative incidents, which demonstrated that 1–4% [Citation6–8] of cases of pars plana vitrectomy (PPV) and around 3% of cases of cataract surgery had adverse systemic events [Citation9,Citation10]. It was also proposed that general anaesthesia was associated with an increased rate of complications, which adversely affected surgical outcomes [Citation6,Citation11]. However, there is little information regarding the total incidence and the prediction of short-term postoperative systemic complications in patients undergoing ophthalmic surgery. Such information may help ophthalmologists to identify patients who are at greater risk for timely intervention and reduce the burden of adverse outcomes.
Therefore, we completed a large and retrospective review conducted at Peking Union Medical College Hospital in Beijing, China, to analyse the incidence and associated risk factors of adverse systemic events after ophthalmic surgeries. The purpose of this study was to determine the overall incidence of postoperative medical adverse events and to identify relevant clinical parameters that could predict postoperative complications. In addition, our secondary objective was to ascertain the characteristics and prognosis of postoperative systemic complications to optimize perioperative management.
Methods
Patient population
This was a population‑based retrospective study. The study protocol was approved by the Ethical Committee of the Peking Union Medical College Hospital (study code K3857) and was conducted in accordance with the Declaration of Helsinki. Patients who underwent inpatient ophthalmic surgery from November 2012 to July 2022 at Peking Union Medical College Hospital, Beijing, China, were retrospectively analysed. The surgery included anterior segment surgery (mainly surgery for cataracts, lens/intraocular lens luxation or aphakic eye, etc.), glaucoma surgery, PPV (divided into simple PPV, PPV with silicone oil tamponade, and PPV with gas tamponade), scleral buckling, strabismus surgery and oculoplastic surgery (eyelid surgery, orbital surgery, lacrimal apparatus surgery and eye removal surgery, etc.). Those that cannot be classified into the above types of surgery, embolization of cavernous aneurysm, for example, were excluded. Only patients with complete medical records were included. All patients were routinely evaluated before surgery, including medical history, physical and ocular examination, blood routine, coagulation function, infectious indicators, hepatic and renal function, urine routines, electrocardiogram evaluation and chest X-ray.
The following data were obtained from electronic medical records after retrospectively reviewed: age, gender, activities of daily living (ADL) (which was divided into three grades according to the score: 61–100 for grade 1; 41–60 for grade 2; and score ≤40 for grade 3), indications for surgery, type of surgery and anaesthesia. Time of the postoperative events was categorized as immediate (occurs intraoperatively or during recovery from anaesthesia), within 24 hours, and after 24 hours.
Presence of baseline comorbidities was recorded including hypertension, DM, coronary artery disease, arrhythmia, chronic heart failure, history of cerebrovascular accident, chronic kidney disease, history of nonocular malignancy, and respiratory, digestive, urinary and locomotor system diseases.
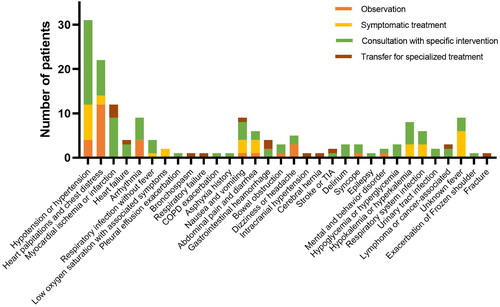
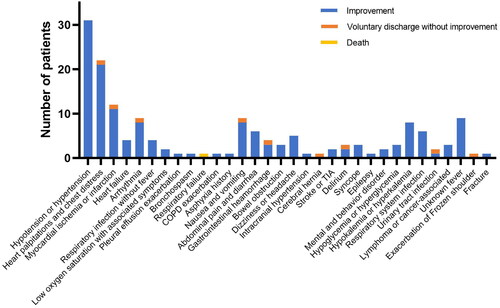
Outcome measure
Postoperative complications that occurred during hospitalization were recorded and the adverse events were further classified into cardiovascular system, respiratory system, digestive system, nervous system, metabolic, fever and locomotor system. The management of the complications was divided into four grades. Grade 1: observation (monitoring patient’s condition and vital signs, oxygen therapy if needed); grade 2: symptomatic treatment (antipyretic, antihypertensive, antiemetic, analgesic, etc.); grade 3: consultation with specific intervention (relevant specialist consults and proposes further treatment plan); grade 4: transfer for specialized treatment (transfer to the relevant department for specialized treatment). Prognosis and discharge mode were classified as improvement, voluntary discharge without improvement, and death.
Statistical analysis
Categorical and numerical data were displayed as number (%) and mean ± standard deviation , respectively. Student’s t-test, rank-sum test and Chi‑square analysis were used to compare the results among the group with or without postoperative complications. The multivariable logistic regression analyses were used to determine the effect of individual risk factors for postoperative complications, presented as odds ratio with 95% confidence intervals (CIs). The multiple linear regression was conducted to identify the factors associated with the severity of the postoperative complications (divided into five grades, grade 1: condition improved after observation; grade 2: condition improved after symptomatic treatment; grade 3: condition improved after consultation with specific intervention; grade 4: transfer needed for specialized treatment; grade 5: death), which were evaluated by the score of ADL and presented as regression coefficients with 95% CI. Statistical analyses were performed using StataSE 12.0 software (StataCorp, College Station, TX). p Values of less than .05 were considered to be statistically significant.
Results
Demographics and baseline characteristics
The general description of the included patients is presented in . Between November 2012 and July 2022, a total of 34,841 patients with a mean age of 59.0 ± 18.7 years underwent inpatient ophthalmic surgeries, 19,034 (54.6%) were females. The mean ADL grading was 1.04 ± 0.22. The most common indication of the surgery was cornea/lens/iris-related disease (62.2%), followed by RD unrelated to PDR (8.8%), and silicone oil tamponade removal (6.1%). The most common type of surgery was anterior segment surgery (62.1%), followed by simple PPV (15.2%) and PPV with silicone oil tamponade (7.7%). 93.5% of the patients underwent local anaesthesia surgery, the others had general anaesthesia. The most common comorbidity was hypertension (37.6%), followed by DM (17.6%) and coronary artery disease (8.7%).
Table 1. Demographics and baseline characteristics of all included patients.
Patients with postoperative systemic complications
A total of 162 complications occurred in 150 of 34,841 patients during postoperative hospitalization with an incidence rate of 0.4%. Cardiovascular events were the most common complications and accounted for 48.1% (78/162), followed by digestive complications as 13.6% (22/162), fever as 12.3% (20/162) and nervous system complications as 11.1% (18/162) ().
For the management, 28 cases (17.3%) had conditions improved after observation, 31 cases (19.1%) after symptomatic treatment, 89 cases (54.9%) had consultation with specific intervention, while 14 cases (8.6%) were transferred to the corresponding departments for specialized treatment. For the prognosis, 93.8% (152/162) had condition improved after proper interventions, 5.6% (9/162) were not improved and chose voluntary discharge, and one patient died of respiratory failure secondary to postoperative pulmonary infection. The postoperative complications and detailed management are summarized in and and .
Table 2. Management and prognosis of postoperative complications.
For the patients with postoperative systemic complications, there was no significant difference in age and sex ratio when compared with the patients without postoperative complications. While their ADL grading was statistically significantly different (p < .05, ), the composition of the indications for surgery, type of surgery, anaesthesia and previous medical history were also significantly different (p < .05, ).
Factors associated with the risk and severity of postoperative systemic complications
The multivariable logistic regression analyses indicated that a worse ADL grade, indication of primary intraocular lymphoma (PIOL) or intraocular tumour, surgery of simple PPV, PPV with silicone oil tamponade, PPV with gas tamponade, general anaesthesia, history of DM, chronic heart failure and digestive system disease were positively correlated with the risk of postoperative systemic complications (p < .05, ). While the indications of cornea/lens/iris-related disease, glaucoma, silicone oil tamponade removal, comorbidities of coronary heart disease and history of nonocular malignancy were negatively correlated with the risk of postoperative systemic adverse events (p < .05, ).
Table 3. Multivariate logistic regression analysis for risk factors and severity of postoperative complications.
The multiple linear regression found that a worse ADL grade, comorbidities of DM and respiratory system disease were positively correlated with the severity of the complications (p < .05, ).
Discussion
In this 10-year retrospective study, we reviewed the incidence and management of postoperative systemic complications in 34,841 patients who underwent inpatient ophthalmic surgery. We found that the overall incidence rate was 0.4% (162 events in 150 cases), and the most common complications were cardiovascular events (48.1%), followed by digestive complications (13.6%) and fever (12.3%). 17.3% of the cases had conditions improved after observation, 19.1% after symptomatic treatment, 54.9% had consultation with specific intervention, and 8.6% were transferred to the corresponding departments for specialized treatment. For the prognosis, 93.8% had condition improved, 5.6% chose voluntary discharge without improvement, one patient died of respiratory failure as a result of postoperative respiratory infections. A worse ADL grading, indication of PIOL or intraocular tumour, surgery of simple PPV, PPV with silicone oil tamponade, PPV with gas tamponade, general anaesthesia, comorbidities of DM, chronic heart failure and digestive system disease were the risk factors positively correlated with postoperative systemic complications (p < .05). A worse ADL grading, comorbidities of DM and respiratory system disease were also positively correlated with the severity of the adverse events (p < .05).
In our series, the incidence of postoperative systemic complications was 0.4%, which was lower than the previous studies. A meta-analysis [Citation10] including three randomized clinical trials with a total of 21,531 cataract cases reported 707 surgery-associated medical adverse events (3.3%), of which 61 occurred during hospitalization (0.028%) and the rest within 2 months postoperatively. For cases undergoing surgery for primary rhegmatogenous RD, Alabi et al. [Citation8] reported intraoperative and postoperative systemic complications of 5.7% (11/193) and 1% (2/193), respectively. McCannel et al. [Citation6] found that 2.6% (11/418) of cases occurred postoperative adverse events within 4 weeks after vitreoretinal or ocular oncologic surgery under general anaesthesia. According to the study of Shalwala et al. [Citation7], the incidence of systemic adverse events after vitreoretinal surgery within 30 days was 4% (89/2215), with about 72% of the complications occurring within the first 24 h. We thought the differences in observation time and type of surgery could be the reason for the significant variation in reporting rates. In reviewing the electronic medical record, we found that although patients were asked to visit our ophthalmology clinic for follow-up at one week and one month after surgery, some complications data may still be lost because more than half of our patients came from out of town, which means that they returned to local hospitals for follow-up. Therefore, our study mainly focused on the systemic complications occurring during hospitalization, where the average hospital stay was 1–3 days for anterior segment surgery and appropriately longer but usually less than 1 week for posterior segment surgery. Besides, all common types of ophthalmic surgery were included in our research to achieve a more comprehensive description. This was a continuous large sample study at a single ophthalmic centre that yields objective results and focuses on the risk and management of postoperative complications during hospitalization, in order to provide a solid reference for the ophthalmologist worldwide.
The cardiovascular events (48.1%) were not surprisingly the most common postoperative adverse events given most patients of advanced age. Of these, hypotension and hypertension with symptoms were the most common. It has been reported that the risk of ischemic heart disease and stroke doubles for every 20/10 mmHg increase in blood pressure [Citation12]. Severe complications were rare, with four cases of congestive heart failure and 12 cases of myocardial ischemia or infarction. Most of those cases had a history of coronary artery disease, so these cardiovascular events might be triggered by preoperative stress or unauthorized discontinuation of anticoagulants [Citation13].
Digestive system events accounted for 13.6% of postoperative complications, with nausea and vomiting being the most common ones. Scleral buckling and strabismus surgery were found to cause nausea and vomiting due to pulling on the extraocular muscles; therefore, a causal relationship seems likely. General anaesthesia is another important reason, with female gender, lower body mass index and inhalation anaesthesia reported as risk factors [Citation14]. McCannel et al. [Citation6] suggested that persistent severe postoperative nausea and vomiting, and subsequent dehydration might lead to myocardial ischemia or infarction. More importantly, one patient in the study was transferred to the department of gastroenterology for further intervention of persistent severe vomiting over one week. He was considered to be suffering from gastrointestinal dysfunction due to a long history of DM eventually.
Fever after ophthalmic surgery accounted for 12.3% of postoperative complications. The most common cause of fever was elderly with respiratory infection, followed by tumour-related fever, and urinary tract infection. In children, fever happened after general anaesthesia but usually did not exceed 38.5 °C, which was considered to be related to disorders of the thermoregulatory centre. Fever in children could be relieved with antifever medicine, such as acetaminophen or ibuprofen.
A total of 18 cases of nervous system events occurred in this study, with serious complications including one case of stroke and one case of cerebral hernia. The case of cerebral hernia occurred the day after surgery in a patient who underwent diagnostic vitrectomy for suspected PIOL, and was referred to the haematology department and finally diagnosed with primary central nervous system lymphoma. In terms of metabiotic, hyperkalaemia and hypokalaemia were the main disorders. Hyperkalemia mostly occurred in PDR patients and was mainly associated with poor glycaemic control, while hypokalaemia was probably attributed to postoperative nausea and vomiting and inadequate food intake [Citation15]. The blood glucose of our PDR patients was routinely monitored during hospitalization, so serious complications like diabetic ketoacidosis or diabetic hyperosmolar syndrome were well avoided. Three patients suffered from postoperative delirium, which was found to be associated with inadequate treatment of perioperative pain, and nalbuphine, which has an adequate analgesic effect on pain management after ophthalmic surgery in preschool children, may reduce the incidence of delirium [Citation16]. In addition, an randomized controlled trial study found that visual impairment was responsible for the development of delirium in preschool children, and that prophylactic eye patch treatment could reduce the development of delirium [Citation17].
In our series, one patient died 28 days postoperatively due to respiratory failure caused by postoperative pulmonary infection. This 79-year-old man had a history of aspiration pneumonia one year before surgery and was subsequently treated with long-term aerosol inhalation. He came to the emergency ophthalmology department due to acute angle closure glaucoma and underwent bilateral phacoemulsification combined with goniosynechialysis surgery successively. A recurrent high fever (38.3–39.7 °C) with a large amount of yellow pus sputum was seen two days after surgery. Blood routine indicated elevated leukocytes, chest computed tomography scan suggested bacterial pneumonia. He was given anti-infection treatment and sputum drainage, but the infection was poorly controlled and he died 28 days after the ocular surgery. The elderly were more prone to musculoskeletal abnormalities and neurological disorders, which make them susceptible to respiratory dysfunction.
In this study, several risk factors were identified for postoperative systemic complications. General anaesthesia and comorbidities of chronic heart failure were significant predictors for systemic adverse events, which were consistent with the results of the previous studies found in PPV surgery [Citation7,Citation8]. We also found that patients with worse ADL grading, patients diagnosed with PIOL, and PPV were risk factors for systemic complications. Because a worse ADL score reflects a poor general condition and more complicated comorbidity of the patients, we suggested that ADL should be regarded as a routine assessment after admission, and more attention should be paid to those patients with worse ADL. Our study also identified patients with history of DM and digestive disease as the risk factors, which was inconsistent with the results of previous studies, as they reported a notable association of coronary artery disease, asthma and chronic renal disease with systemic complications [Citation7].
There were still several limitations in this study. First, this was a single‑centre study, the data might not be comparable with the data from a multicentre. Second, this research only focused complications that occurred during hospitalization, those developed after discharge could be missed and therefore causing an underestimation of the true adverse events rate. Lastly, there might be some inherent selection bias in those patients who were at potentially higher risk of postoperative complications, as they may have more pre-admission tests and evaluation, then preferentially be referred for systemic interventions before ocular surgery. However, we would like to highlight the multiple strengths of this study, including a large number of consecutive patients, the investigation of a hot and unresolved topic, and the nearly complete identification of medical events during the study period. Although prospective trials are preferable, the low incidence of postoperative systemic events in ophthalmology makes such studies difficult to conduct. In any case, a large sample size means more convincing outcomes and might result in more statistical power to detect subtle but relevant risk factors.
Conclusions
In summary, the incidence of postoperative systemic complications was low among patients undergoing ophthalmic surgery. Most adverse events were mild and might not lead to permanent morbidity, and could be relieved after observation, symptomatic or specialist consultation. A worse ADL grading, PPV surgery, general anaesthesia, history of DM, chronic heart failure and digestive system disease were the positive risk factors. A worse ADL grading, history of DM and respiratory system disease were also positively correlated with the severity of the complications.
Author contributions
SYC and YFW completed the entire process, including study design, data collection, and manuscript drafting. XWG, QZ and LHM contributed to the revision of the manuscript. YXC and XYZ participated in statistical analysis and the entire process of drafting and revising the manuscript. All authors have read and approved the final manuscript.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethical Committee of the Peking Union Medical College Hospital (study code K3857).
Disclosure statement
The authors declare no conflict of interest.
Data availability statement
All data are available within the manuscript and upon request to the corresponding author.
Additional information
Funding
References
- Zhang W. Number of ophthalmic inpatients in China from 2012 to 2021; 2022 [cited 2022 Jan 27]. Available from: https://wwwstatistacom/statistics/952978/china-number-of-ophthalmic-inpatients/
- Hanna V, Popovic MM, El-Defrawy S, et al. Preoperative evaluations for ophthalmic surgery: a systematic review of 48,869 eyes. Surv Ophthalmol. 2023;68(3):1–10. doi: 10.1016/j.survophthal.2022.12.004.
- Alboim C, Kliemann RB, Soares LE, et al. The impact of preoperative evaluation on perioperative events in patients undergoing cataract surgery: a cohort study. Eye. 2016;30(12):1614–1622. doi: 10.1038/eye.2016.203.
- Raczyńska D, Glasner L, Serkies-Minuth E, et al. Eye surgery in the elderly. Clin Interv Aging. 2016;11:407–414. doi: 10.2147/CIA.S101835.
- Chen CL, Lin GA, Bardach NS, et al. Preoperative medical testing in Medicare patients undergoing cataract surgery. N Engl J Med. 2015;372(16):1530–1538. doi: 10.1056/NEJMsa1410846.
- McCannel CA, Nordlund JR, Bacon D, et al. Perioperative morbidity and mortality associated with vitreoretinal and ocular oncologic surgery performed under general anesthesia. Trans Am Ophthalmol Soc. 2003;101:209–213; discussion 213–205.
- Shalwala A, Hwang RY, Tabing A, et al. The value of preoperative medical testing for vitreoretinal surgery. Retina. 2015;35(2):319–325. doi: 10.1097/IAE.0000000000000306.
- Alabi RO, Turnbull ZA, Coombs PG, et al. Assessing the value of preoperative medical clearance in patients with primary rhegmatogenous retinal detachment. Clin Ophthalmol. 2019;13:1711–1718. doi: 10.2147/OPTH.S209681.
- Schein OD, Katz J, Bass EB, et al. The value of routine preoperative medical testing before cataract surgery. Study of medical testing for cataract surgery. N Engl J Med. 2000;342(3):168–175. doi: 10.1056/NEJM200001203420304.
- Keay L, Lindsley K, Tielsch J, et al. Routine preoperative medical testing for cataract surgery. Cochrane Database Syst Rev. 2019;1(1):CD007293. doi: 10.1002/14651858.CD007293.pub4.
- Mendes JF, Vieira V, Freitas C. Peri-operative anaesthetic complications of ophthalmic surgery. Br J Anaesth. 2016;117:EL_13721. doi: 10.1093/bja/el_13721.
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2.
- Kong KL, Khan J. Ophthalmic patients on antithrombotic drugs: a review and guide to perioperative management. Br J Ophthalmol. 2015;99(8):1025–1030. doi: 10.1136/bjophthalmol-2014-306036.
- Nitahara K, Sugi Y, Shono S, et al. Risk factors for nausea and vomiting following vitrectomy in adults. Eur J Anaesthesiol. 2007;24(2):166–170. doi: 10.1017/S0265021506001360.
- Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118(1):85–113. doi: 10.1213/ANE.0000000000000002.
- Leister N, Trieschmann U, Yücetepe S, et al. Nalbuphine as analgesic in preschool children undergoing ophthalmic surgery and the occurrence of emergence delirium. Br J Ophthalmol. 2022. doi: 10.1136/bjo-2022-321575.
- Lin Y, Shen W, Liu Y, et al. Visual preconditioning reduces emergence delirium in children undergoing ophthalmic surgery: a randomised controlled trial. Br J Anaesth. 2018;121(2):476–482. doi: 10.1016/j.bja.2018.03.033.