Abstract
Medical security support for rehabilitation therapy in China is different from that in other countries. We investigated whether the discharge plan to continue rehabilitation therapy in tertiary hospitals for patients after traumatic spinal cord injury (TSCI) was influenced by payment sources or other conditions. This was a cross-sectional, observational study. Information was collected on the general condition, caregiver, types of payment sources for continued rehabilitation, American Spinal Injury Association Impairment Scale (AIS) scores, and discharge plans. In total, 135 patients with TSCI (107 male, mean age 41.00 ± 13.73 years, mean spinal cord injury duration 238.43 ± 345.54 days) were enrolled. Medical insurance (43%) and out-of-pocket payments (27.4%) were the primary payment sources. Although most patients were beyond the acute phase, 40% continued rehabilitation therapy at other tertiary hospitals. The caregiver, payment sources, injury level, AIS level, and complete urinary tract infection (UTI) were different due to discharge plans (p > .05). Patients seemingly consider a higher AIS level and co-UTI as the requirement for tertiary hospital therapy. In non-medical insurance payment source patients, the discharge plan also differed due to the AIS level and co-UTI (p > .05). However, in medical insurance patients, the discharge plan differed only in terms of TSCI duration (p > .05). The restricted duration of medical coverage restricted the continuation of rehabilitation therapy and influenced the discharge plan of most patients with TSCI.
Introduction
Spinal cord injury (SCI) is a devastating incident that results from trauma to any level of the spinal cord, causing temporary or permanent damage [Citation1,Citation2]. Studies in other countries have shown that traumatic spinal cord injury (TSCI) is second only to traumatic brain injury, which causes disability [Citation3]. Patients and their families experience the worst bodily limitations and financial burden in the first year after a traumatic accident, with over half of the overall medical expenditure occurring this year [Citation4]. Before making the discharge plan, patients with TSCI and caregivers will consider both economic and body functional conditions, especially in the post-acute stage. However, the factors that play a more important role in the discharge plan remain unclear.
In China, universal healthcare payment policies and payment cycles for rehabilitation therapy differ from those in many other countries. Government medical insurance does not cover injuries related to certain situations such as motor vehicle collisions, suicide attempts, or physical alterations. Unless they have purchased commercial insurance, patients with such injuries must pay out-of-pocket medical care. In China, the predominant components of medical insurance encompass Urban Employee Basic Medical Insurance, Urban Resident Medical Insurance, and the New Rural Cooperative Medical Scheme, among others. These insurance programs primarily cater to the medical expenses incurred by individuals seeking treatment for illnesses, thereby rendering costs arising from health conditions eligible for reimbursement by medical insurance. Nonetheless, occurrences of accidental harm, such as traffic accidents and suicide, are typically not classified as conventional health issues. This can be attributed to the differentiation between medical insurance and accidental injury insurance within the realm of insurance types. Additionally, the extensive burden that would be placed on the insurance fund if regular health insurance were to encompass all health risks contributes to this phenomenon. Consequently, incidents of this nature are not included within the scope of medical insurance payments. Additionally, national policies guide the distribution of medical resources and adjust expenses between tertiary and other hospitals, which inadvertently increases the burden on patients willing to continue rehabilitation therapy at tertiary hospitals with out-of-pocket payments.
In recent years, the Chinese government has attempted to expand medical insurance coverage to narrow inequalities in access to healthcare between different resident groups; by the end of 2022, the Chinese medical security system had covered 95% of its residents [Citation5,Citation6]. However, guaranteed payments for rehabilitation therapy are only available for 90 days after the current injury (the items included in the medical insurance reimbursement list encompass manual functional examinations, spinal joint mobilization, and isokinetic muscle strength training that are commonly used, and clinically essential items are basically incorporated into the medical insurance coverage). Moreover, due to the medical insurance policy, patients who received medical insurance services in systems could not be transferred to other payment methods even if they voluntarily made out-of-pocket payments. The period of hospitalization, particularly in tertiary hospitals in China, is limited to 14 days, and patients need to consider their next period of therapy. Little is known about the effect of payment sources on discharge plans in patients with TSCI past the medical coverage timeframe in China.
Therefore, the current study aimed to investigate the discharge plans of patients with TSCI and whether they were influenced by the payment source, severity of injury, or other conditions.
Methods
Study design
This cross-sectional study was conducted between January and October 2023 at a regional rehabilitation center in a university-affiliated hospital, the largest SCI center in Yunnan province, China. This study was reviewed by the Ethics Committee of tertiary hospitals, and consent was obtained (no. PJ-2022-74). All patients were provided with verbal and written instructions on all the details of the experiment.
Participants
Eligible patients were those aged >18 years who experienced SCI due to trauma in a stable general condition after injury and were transferred or admitted to our rehabilitation department. Other causes of injury, such as myelitis, spinal cord tumor, and unexpected spinal injury during the operation, were excluded from this study.
Data collection
Medical information was collected from medical records and patients, and the caregivers investigated the discharge plan seven days before the scheduled discharge by our researcher. Data on epidemiological characteristics, infections, complications, caregivers, payment sources, discharge plans, and American Spinal Injury Association Impairment Scale (AIS) scores were collected. The discharge plans were divided into three categories: (a) discharge to another tertiary hospital, (b) discharge to a community hospital, or (c) discharge to home.
Statistical analysis
Statistical analysis was conducted because of the non-normality of all data variables. The differences between the discharge plans and payment sources according to the patient’s characteristics were analyzed using the Kruskal–Wallis H test, and a post hoc test was performed using the Mann–Whitney U-test. Correlations were conducted between the discharge plan, caregiver, injury level, AIS level, and co-UTI using Kendall’s correlation analysis. All statistical analyses were performed using SPSS version 26 (IBM, Armonk, NY), and statistical significance was set at p < .05. Data were plotted using the GraphPad Prism 8.0 program (GraphPad Inc., San Diego, CA).
Results
Demographic and clinical characteristics
In total, 135 patients were included in this study, 107 of whom were male (79.25%). The average age of the participants was 41 years, and the average TSCI duration was 238.43 days. The leading cause of injury was falls (48.14%), followed by motor vehicle collisions (26.67%). The thoracic region was the most commonly affected level of injury, representing 57.03% of cases, and the proportion belonging to AIS grade A, which is the most severe classification, is higher than other levels. For voiding management, most patients with TSCI in our study opted for an indwelling bladder catheter (IBC), with a prevalence of 58.21%. Additionally, approximately one-third of the patients experienced urinary tract infections (UTIs), and nearly half reported neuropathic pain (NP) symptoms ().
Table 1. Demographic characteristics in all patients.
Payment methods and discharge plan
In this study, the main source of payment was medical insurance, accounting for 42.96% of the cases. Additionally, over 27% of patients relied on out-of-pocket payments, primarily stemming from injuries sustained at private worksites or private businesses, which were covered by the owners. Despite the majority of patients being beyond the acute phase, 40% expressed intention to seek treatment at another tertiary hospital ().
Table 2. Payment sources and discharge plan in total patients.
The discharge plan varied depending on factors such as caregiver, payment source, injury level, AIS level, and co-UTI (p < .05). Furthermore, the AIS score and co-UTI differed between patients discharged to tertiary hospitals and those discharged to community hospitals, as well as between tertiary hospitals and returning home (p < .05). The number of patients who planned discharge to the community hospital between back to home differed according to injury level and AIS level (p < .05) ().
Table 3. Difference between discharge plan and characteristics in total patients.
Subgroup analysis and correlation analysis
In patients who received compensation from medical insurance, the discharge plan varied based solely on the duration of TSCI (p < .05). Conversely, among patients with alternative payment sources, the discharge plan differed significantly in relation to the caregiver, payment sources, AIS level, and co-UTI (p < .05) ().
Figure 1. The items showed significant difference in different payment resources according to discharge plan and the correlation analysis between discharge plan and other factors. (A) The items showed significant difference in between-group analysis in patient utilizing medical insurance payment; (B) the items showed significant difference in between-group analysis in patient utilizing other payment resources; (C) correlation analysis between discharge plan and significant factors; TSCI: spinal cord injury; AIS: American Spinal Injury Association Impairment Scale; UTI: urinary tract infection (only the items that showed significant difference between groups according to the discharge plan are shown in A and B).
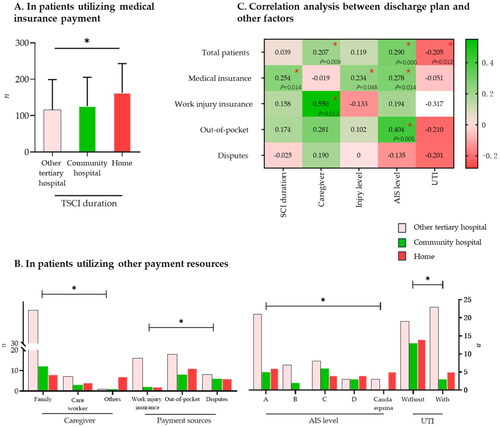
Correlation analysis was conducted to examine the relationship between the discharge plan and various factors found to be statistically significant in the previous analysis. The results revealed a moderate correlation between discharge plan and caregiver in work injury insurance payment patients (r = 0.55, p = .013), as well as between discharge plan and AIS score in out-of-pocket payment patients (r = 0.404, p = .005). However, the remaining correlations either demonstrated weak associations or no significant relationships between the discharge plan and previously identified factors.
Discussion
The economic burden on patients with TSCI is a great concern. In China, universal health coverage was achieved in 2013, and basic medical insurance covered urban residents, employees, and, more recently, rural cooperatives. However, all these types of medical insurance provide rehabilitation therapy for only the first three months after therapy initiation, which makes the burden of out-of-pocket payment rapidly increase when the patient is more than 90 days post-onset. The limited duration of rehabilitation therapy after injury covered by medical insurance was beneficial in reducing the high pressure of health insurance funds to pay [Citation7]. However, due to the long recovery period, more than half of the patients with SCI in China bear all rehabilitation costs in the late stages in China [Citation8].
In other countries, the rehabilitation period was bundled into the cost of surgery, such as a single bundled payment to healthcare organizations for all services related to the received health service 90 days after surgery [Citation9]. In contrast, in China, the medical insurance system could automatically screen for a high degree of suspicious information, such as still receiving rehabilitation services more than 90 days after injury and providing related penalties to the responsible doctors. The policy of patients consuming but doctors being punished has resulted in the need for clinicians to exercise caution when treating patients with medical insurance, particularly when their payment period is nearly 90 days. This is because they may have to manually alternate some of the rehabilitation therapy costs to be paid out of pocket. Additionally, the limited time of coverage provided by medical insurance was also the primary factor in the difficulty of community rehabilitation and services, as perceived by general practitioners in community hospitals [Citation10].
Given the need for specialized services and the duration of stay in rehabilitation units, it is advisable to adopt acute rehabilitation services within tertiary-level hospitals as the optimal service model, whereas post-acute services should be implemented at the secondary level. Consequently, the government has been compelled to increase the cost of services in tertiary hospitals to encourage patient dispersal to community or lower-level hospitals. Nevertheless, the lack of precise definitions for these distinct services has resulted in a concentration of patients seeking high-quality care at high-level hospitals despite the associated higher costs [Citation10].
Previous studies have shown that motor vehicle collisions and falls are the most frequent causes of TSCI [Citation11,Citation12]. The etiology of TSCI in Yunnan Province appears to differ from that in other areas of China. In our study, more than half of the patients with TSCI were injured, participating in activities with a high risk of falls. In Guangdong Province, Beijing City itself, and several richer cities, the main etiology of which has been reported to be motor vehicle collisions or high falls and increased falls in older adults [Citation11,Citation12]. However, high falls and injuries from ‘being struck by an object’ are common etiologies of TSCI in Yunnan Province. A possible explanation for this is that Yunnan Province is in Southwest China, where the development pattern is different from that of other developed regions. Construction sites and topography-related high falls may, therefore, be more likely in Yunnan Province. A large proportion of the patients are injured during farm work or construction. This may suggest that most patients with TSCI, such as AIS A patients, had severe injuries, similar to our study.
Patients with TSCI, particularly those with complete injuries, are often unable to care for themselves. Although a previous study noted that one of the important types of rehabilitation services is long-term rehabilitation services and that patients with TSCI need lifelong continuation of rehabilitation, patients with TSCI facing permanent disability and loss of income often cannot utilize these costly services [Citation13,Citation14]. Secondary and community hospitals can provide relatively simple and inexpensive rehabilitation; however, most of these institutions do not have professionals working in multidisciplinary teams in this area [Citation15].
AIS grade A was the most common condition in our study. Patients with complete injury were hospitalized for longer durations owing to the higher risk of complications in complete TSCI than in those with incomplete TSCI [Citation8,Citation16,Citation17]. This suggests that patients with complete TSCI are more willing to use higher levels of rehabilitation services, as the correlation shows in the present study in patients with other payment sources. According to our study, patients who were financially supported by external institutions or individuals, such as work injury insurance, disputes, or especially out-of-pocket payments, primarily focused on their health condition when contemplating their discharge plan. Conversely, patients covered by medical insurance appeared to prioritize the duration of their TSCI as it directly impacted their economic burden. These characteristics could also be found in the different SCI durations of different payment sources; it is easy to find more than one year of patients in other payment sources, but most of the patients paid by medical insurance were less than one year.
We were taken aback by the discovery that patients with TSCI tend to consider the AIS level and the presence of co-UTI as criteria for continuing high-quality rehabilitation therapy. The most prevalent method for managing voiding in this study was IBC management, which carries various risks, including UTI [Citation18]. To optimize the benefits of neurogenic bladder training, which is commonly observed in patients with injuries above the L2 level, intermittent catheterization should be employed as the gold standard to facilitate bladder emptying [Citation19].
To date, there is a dearth of systematic comparative studies on service provision for TSCI across different countries, and payment systems exhibit significant variations across these countries. The objective of this study was to analyze the discharge plan for patients with TSCI in China, considering various payment methods. Although a significant number of patients expressed a preference for superior rehabilitation services, it is important to acknowledge that the majority of patients covered by medical insurance face restrictions on the duration of their insurance, as determined by the rehabilitation service criteria, and have to choose other options. However, it is noteworthy that these patients constituted the majority of the patients in this study, suggesting that the demand for high-quality rehabilitation may have been underestimated.
Limitation
This study had some limitations. First, it was conducted at a single center, which means that while the payment characteristics and observed phenomenon may be common in China, the results may vary in other regions owing to differences in the duration of TSCI. Second, although the AIS score was used to assess the extent of injury, other functional factors in the discharge plan were not compared. It is important to note that this study did not include patients with milder injuries, who may have been underreported and who were discharged from our hospital but not our center for other reasons, such as earlier return to independence.
Conclusions
Definitions of the cost of care and different time horizons are inherently complex, with broad heterogeneity and differences among health system structures. Thus far, the economic situation of TSCI-related research has been halted because it is extremely costly. This study investigated discharge plans according to payment sources to understand the hidden difficulties faced by patients with TSCI who had to choose a community hospital or return home for economic reasons. These results can assist healthcare providers and administrators in making better decisions concerning the allocation of resources based on patient needs and disease characteristics.
Ethical approval
This study was approved by the Institutional Review Board of the Second Hospital of Kunming Medical University (No. PJ-2022-74). All patients were informed of the study’s purpose and provided informed consent.
Authors’ contributions
All authors have made substantial contributions to this work and have approved the final version of the manuscript. Concept and design: LHJ, YML; Acquisition of data: LHJ, YQH, HNW; Statistical analysis: JCD, LHJ; Data interpretation: YQH, YFD, WYW; Authorship of the original draft: LHJ, YQH; Review and editing: YML; Funding: YML, YFD.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets used and/or analyzed for the development of this manuscript are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Garcia-Arguello LY, O’horo JC, Farrell A, et al. Infections in the spinal cord-injured population: a systematic review. Spinal Cord. 2016;55(6):1–8. doi: 10.1038/sc.2016.173.
- White N-H, Black N-H. Spinal cord injury facts and figures at a glance. National spinal cord injury statistical center, facts and figures at a glance. Birmingham (AL): University of Alabama at Birmingham; 2017.
- Polinder S, Meerding WJ, Mulder S, et al. Assessing the burden of injury in six European countries. Bull World Health Organ. 2007;85(1):27–34. doi: 10.2471/blt.06.030973.
- McDaid D, Park A-L, Gall A, et al. Understanding and modelling the economic impact of spinal cord injuries in the United Kingdom. Spinal Cord. 2019;57(9):778–788. doi: 10.1038/s41393-019-0285-1.
- Fu R, Bao H, Su S, et al. Effect of the medical insurance on the quality of care for Chinese patients with chronic heart failure. Int J Qual Health Care. 2016;28(6):785–792. doi: 10.1093/intqhc/mzw105.
- National Bureau of Statistics. Statistical Communiqué of the People’s Republic of China on the 2022 National Economic and Social Development; 2023 [Online]. Available from: https://www.stats.gov.cn/english/PressRelease/202302/t20230227_1918979.html
- An Y, Wang M, Wu X, et al. Analysis of the economic performance of municipal children’s hospitals in Shanghai: a study on the impacts of policy changes in healthcare service prices. Ann Transl Med. 2020;8(22):1479–1479. doi: 10.21037/atm-20-6863.
- Zhang Z, Wang F, Wu Y. Factors affecting length of stay in hospital of patients with traumatic spinal cord injury in China. J Rehabil Med. 2020;52(11):jrm00123. doi: 10.2340/16501977-2761.
- Finkelstein A, Ji Y, Mahoney N, et al. Mandatory Medicare bundled payment program for lower extremity joint replacement and discharge to institutional postacute care: interim analysis of the first year of a 5-year randomized trial. JAMA. 2018;320(9):892–900. doi: 10.1001/jama.2018.12346.
- Jin L, Han Y, Dong J, et al. Current status of rehabilitation services and problems in Yunnan Province, Southwest China: a general doctors’ questionnaire-based study. Ann Med. 2023;55(2):2268123. doi: 10.1080/07853890.2023.2268123.
- Chen J, Chen Z, Zhang K, et al. Epidemiological features of traumatic spinal cord injury in Guangdong Province, China. J Spinal Cord Med. 2021;44(2):276–281. doi: 10.1080/10790268.2019.1654190.
- Liu J, Liu H-W, Gao F, et al. Epidemiological features of traumatic spinal cord injury in Beijing, China. J Spinal Cord Med. 2022;45(2):214–220. doi: 10.1080/10790268.2020.1793505.
- Gutenbrunner C, Blumenthal M, Geng V, et al. Rehabilitation services provision and payment. Am J Phys Med Rehabil. 2017;96(2 Suppl. 1):S35–S40. doi: 10.1097/PHM.0000000000000668.
- Saur M, Abel R. Rehabilitation nach Querschnittlähmung. Orthopade. 2015;44(6):477–488. doi: 10.1007/s00132-015-3125-9.
- Negrini S, Kiekens C, Zampolini M, et al. Methodology of "Physical and Rehabilitation Medicine practice, Evidence Based Position Papers: the European position" produced by the UEMS-PRM Section. Eur J Phys Rehabil Med. 2015;52(1):134–141.
- Stillman MD, Barber J, Burns S, et al. Complications of spinal cord injury over the first year after discharge from inpatient rehabilitation. Arch Phys Med Rehabil. 2017;98(9):1800–1805. doi: 10.1016/j.apmr.2016.12.011.
- Zatzick D, Jurkovich GJ, Rivara FP, et al. A national US study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Ann Surg. 2008;248(3):429–437. doi: 10.1097/SLA.0b013e318185a6b8.
- Wu B, Wang J, Chen X-J, et al. Bladder perforation caused by long-term catheterization misdiagnosed as digestive tract perforation: a case report. World J Clin Cases. 2020;8(20):4993–4998. doi: 10.12998/wjcc.v8.i20.4993.
- Shen L, Wu H, Chen H, et al. A case report: intermittent catheterization combined with rehabilitation in the treatment of carbapenem-resistant Klebsiella pneumoniae catheter-associated urinary tract infection. Front Cell Infect Microbiol. 2022;12:1027576. doi: 10.3389/fcimb.2022.1027576.

