Abstract
Purpose
Hypertension is a major public health problem, thus, its timely and appropriate diagnosis and management are crucial for reducing cardiovascular morbidity and mortality. The aim of the new Hungarian Hypertension Registry is to evaluate the blood pressure measurement practices of general practitioners (GPs), internists and cardiologists in outpatient clinics, as well as to assess the seasonal variability of blood pressure.
Materials and methods
Omron M3 IT devices were used during four-month periods between October 2018 and April 2023 in GP practices and in hypertension clinics. The blood pressure data were then transmitted online from the monitors’ cuffs to a central database using the Medistance system of Omron.
Results
Family physicians (n = 2491), and internists/cardiologists (n = 477) participated in the study. A total of 4804 821 blood pressure measurements were taken during 10 four-month evaluation periods. In the ten periods, the daily average number of measurements was between 3.0 and 5.6. Following ESH diagnostic criteria, the proportion of subjects in optimal, normal and high-normal blood pressure categories were 14, 13.4 and 16.7%, respectively. Altogether 56% of the measurements belonged to stage 1, stage 2 or stage 3 hypertension categories (31.6, 17.1 and 7.4%, respectively). On average, a difference of 5/2 mmHg was observed between winter and summer data in systolic and diastolic blood pressures, respectively. The average systolic blood pressure values were higher in GP practices with more than 2000 patients than in the ones with less than 1500 patients (141.86 mmHg versus 140.02 mmHg, p < 0.05).
Conclusion
In conclusion, the low daily average number of blood pressure measurements indicates a limited blood pressure screening awareness/capacity in the case of Hungarian family physicians. In GP practices with more patients, blood pressure is usually less well-controlled. These results suggest that the further promotion of home blood pressure monitoring is necessary.
PLAIN LANGUAGE SUMMARY
What is the background?
The standard method for the diagnosis of hypertension and for the control of treatment efficacy in hypertensive patients is office blood pressure measurement.
Until now we had no real-life data on the blood pressure measurement practices of general practitioners (GPs), internists and cardiologists.
Although seasonal differences in blood pressure values are well known, we had no data on the extent of these changes.
What is new?
In this real-world, nationwide observational study we were able to measure the frequency of blood pressure measurements in the daily practice of GPs, internists and cardiologists in Hungary, which was found to be very low compared to the number of patients they treat. In practices with more patients, blood pressure is generally less well-controlled.
We could also detect a significant seasonal variation in systolic and diastolic blood pressure values over the observed time periods.
What is the impact?
The low daily average number of blood pressure measurements indicates a limited blood pressure screening awareness/capacity in the case of Hungarian family physicians, supporting the further promotion of home blood pressure measurement.
The marked seasonal blood pressure changes demonstrated by our study require attention and the individual adjustment of treatment in different seasons.
Introduction
Hypertension is the leading risk factor of cardiovascular (CV) morbidity and mortality, thus its effective treatment can markedly improve CV outcome [Citation1]. As its prevalence in adults is between 30–45% in Europe affecting millions in each country, hypertension management is a very important task of general practitioners (GPs), who perform the highest number of hypertension-related consultations [Citation2].
The management of hypertension used to be based mostly on office blood pressure measurement until 2018, when the European hypertension guideline equalised the use of office, home and ambulatory blood pressure measurements for the confirmation of diagnosis and the long-term care of hypertension [Citation3,Citation4]. Accurate office blood pressure measurement requires 3–5 min of rest and repeated measurements meaning three measurements with a one-minute interval, where the average of the second and the third values should be considered for clinical decision [Citation5]. This accurately performed procedure is time-consuming, which, combined with other activities related to hypertension, significantly prolongs visits. As the screening and care of hypertension is only one task in the daily practice of GPs, and their office hours are usually busy, it is likely that not all patients are getting their blood pressure measured properly during visits. Until now, there were no accurate data on the number of blood pressure measurements taken during working days, but with recent technical advances, it is now possible to transmit all blood pressure and time data from devices in the office to a central server for further analysis.
The significance of seasonal blood pressure variability was described decades ago [Citation6]. Blood pressure is higher in winter and lower in summer and this difference may also affect the titration of daily antihypertensive medication [Citation6]. However, data from the Central European region are not yet available.
The aim of our study was to evaluate the blood pressure measurement practices of Hungarian GPs, internists and cardiologists in outpatient clinics. We also aimed to assess the distribution of blood pressure values and the seasonal variation in blood pressure. Our other aim was to access these data by building an efficient, reliable national blood pressure registry system.
Materials and methods
The Hungarian Hypertension Registry is an ongoing multicentre, open-label, observational study, where data collection started in October 2018. Omron M3 IT devices were distributed for four-month periods to family physician practices and to hypertension clinics. The current analysis contains data collected between October 2018 and April 2023. Part of these data have been presented at the Annual Meeting of the European Society of Hypertension and published in abstract form [Citation7]. Blood pressure values were transmitted online from the monitors to a central database using the Medistance system of Omron. GPs, internists and cardiologists working in outpatient clinics were invited to participate in the study. Attending a hypertension management course was not required for the inclusion of the doctors. At inclusion, a survey was completed, which covered demographic and professional data about the physicians and the number of patients cared for in the GP practice. The physicians involved were asked to continue their daily practice with the device being tested and to use the data transmitter once a week to send the blood pressure measurements (including heart rate and the time of measurements) for further analysis. No demographical data on patients were collected.
The study was approved by the Scientific and Research Ethics Committee of the Medical Research Council, the Hungarian Ministry of Health (Approval No.: OGYÉI/42899/2018) and was carried out in accordance with the tenets of the Declaration of Helsinki.
Statistical analysis
Descriptive statistics were reported as mean, standard deviation and relative frequencies. To examine group differences, one-way ANOVA and independent samples t-test were used with partial eta squared and Hedges’ g effect size measurement. For testing association, Pearson’s correlation coefficients were calculated. Statistical calculations were made by IBM SPSS Statistics for Windows, Version 28.0 (IBM Corp. Released 2021. Armonk, NY: IBM Corp).
Results
In the registry, 2983 physicians were involved. Fifteen GPs were excluded from the final analysis due to incomplete descriptive data on the physician or the practices. Finally, 2968 physicians were included in the analysis. shows the descriptive parameters of the included physicians and GP practices. Based on the average age of the doctors, mostly middle-aged physicians were involved. In 2491 cases the physician was a specialised GP with or without any other specialisations, while 477 physicians were internists or cardiologists. The majority of GP practices had 1500–2000 patients and most of the doctors had only one assistant.
Table 1. General descriptives of the physicians and the general practitioners’ practices.
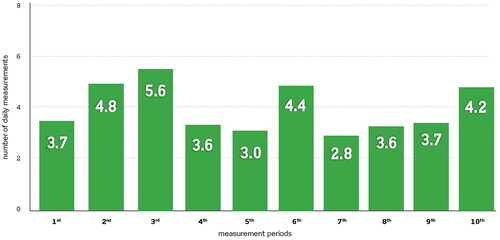
A total of ten 4-month measurement periods were completed. During these periods 4,804,821 blood pressure measurements were recorded. demonstrates the average number of daily measurements in the different measurement periods. The number of daily measurements varied between 3.0 and 5.6. Based on the data of the Hungarian Central Statistical Office, in 2022 the average number of patients treated by a general practitioner daily in the office was 43 (average number of patients in a GP office (n = 11,040)/number of workdays in 2022 (n = 254)) [Citation8]. However, some of these patient visits are due to administrative issues (prescriptions, referral documents or working disability warrants for insurance companies), but it can be concluded that less than every tenth patient had their blood pressure measured in the office.
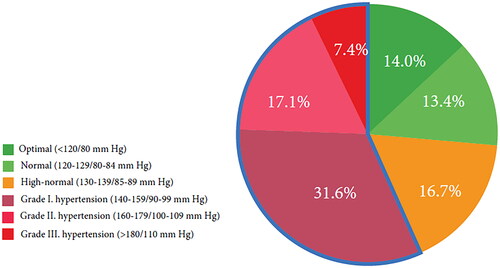
demonstrates the proportion of patients in different blood pressure categories based on the classification used in Europe [Citation4]. 56.1% of the measurements fell into the category of hypertension and 16.7% of them were in the high-normal category, which also requires further evaluation to exclude masked hypertension.
shows the impact of different confounders on the measured blood pressure and heart rate values. Patients treated in the offices of internists/cardiologists had moderately lower blood pressure and heart rate values compared to patients treated in GP practices. Although the number of GP assistants had no effect on the measured blood pressure values, the number of patients in GP practices had a significant impact. Practices with fewer than 1500 patients had 1.8/0.8 mmHg lower systolic and diastolic blood pressure than practices with more than 2000 patients. The increasing number of patients was in correlation with the measured values with r = 0.114, r = 0.100 and r = 0.065 for systolic and diastolic blood pressure and heart rate, respectively (p < 0.001 in all cases).
Table 2. The effect of different confounders for the blood pressure and heart rate.
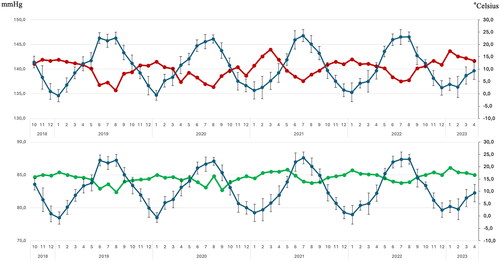
Significant seasonal variation of systolic (mean change 5 mmHg) and diastolic (mean change 2 mmHg) blood pressure values was noticed over the observed periods with lower blood pressure in summer and higher in winter, parallel to the change in the average of mean daily temperature values (.).
Discussion
Based on literature data, our study is the first to use the applied data reporting system, which allowed us to investigate the blood pressure measurement practices of GPs, internists and cardiologists working in outpatient clinics. We found that the average number of measurements on a working day varied between 3 and 6 meaning that only a small proportion of patients had office blood pressure measurement. Additionally, we found marked seasonal variation in blood pressure – until now, no data were available on this issue in the Central European region.
The accurate measurement of blood pressure in the office is fundamental for proper diagnosis and the long-term care of patients with hypertension [Citation3,Citation4]. A sophisticated protocol for office blood pressure measurement is recommended to guide physicians, which includes 3 measurements with 1-min intervals, where the average of the second and the third measurements should be used for clinical decisions [Citation5]. The low number of daily office blood pressure measurements suggests that probably only a low proportion of physicians are adherent to guidelines. This hypothesis is consistent with the results of previous studies based on questionnaire surveys in different countries. A study by Beger C. and their colleagues in Germany found that 66.3% of the patients had only a single blood pressure measurement [Citation9]. In the study by Ozone S. et al. performed in Japanese geriatric health service facilities, it was found that only in 1.6% of the involved centres were more than 80% of the measurements performed at least two or more times to obtain an average value [Citation10]. In a study performed in Salt Lake City, USA, Woolsey S. et al. demonstrated better results, but still only just over half (58.5%) of the responding clinics measured blood pressure twice, which at that time met the recommendation of the US guidelines [Citation11]. These data suggest that physicians in outpatient clinics have a low adherence to blood pressure measurement guidelines and the Hungarian Hypertension Registry data suggest a similar situation in Hungary. In addition to improving physicians’ awareness of blood pressure measurement according to the guidelines, the further promotion of home blood pressure measurement could improve hypertension care on different levels of the healthcare system.
In our study 56.1% of the measurements fall into the category of hypertension. This high proportion of elevated values is probably due to inadequate measurement techniques, but it is still remarkable. During the May Measurement Month (MMM) screening campaigns in 2017 and 2019 the proportion of participants (either treated or untreated) with elevated blood pressure was 30.7% and 29.2%, respectively [Citation12,Citation13]. In the case of MMM, guideline-based blood pressure measurement is required with three measurements and 1- min intervals (all of them are needed to be uploaded electronically) and the average of the second and the third are used for further analysis. It is assumed that these data give a more realistic picture about the rate of subjects with new or uncontrolled hypertension on the level of primary care.
In practices with fewer than 1500 patients, the average blood pressure was lower than in practices with more patients. Different explanations can be hypothesised for this observation. First, this finding can suggest that with a lower number of patients, the physician has more opportunities to perform a higher quality of care. This conclusion is logically associated with the fact that the guideline-based blood pressure measurement procedure is time-consuming as the appropriate office blood pressure measurement protocol requires about 16 min [Citation14]. Moreover, the time required for the treatment of comorbidities and further educational duties of the physician is added to the total time which could be required for an extended care of a hypertensive patient. This is probably challenging for GPs. A second hypothesised explanation for this finding is based on the tendency of GPs to concentrate on the most serious cases. The pressure for patient selection can increase as the number of patients increases. Especially doctors with a large number of patients may want to focus on their high-risk patients due to prioritisation principles and consequently, fewer measurements are performed in low-risk subject for screening purposes, resulting in a higher average value of measurements. The clarification of these hypothesis requires further studies, as the lower quality of care and/or a higher level of patient selection can both lead to higher blood pressure results in the practices with a growing number of patients.
The blood pressure and heart rate results were better controlled by internists and cardiologists compared to the GPs, however, these were only small or moderate differences. The explanation for this observation can also be based on the quality of care. GPs in Hungary have in general 4 office hours daily and 43 patients on an average day, meaning that one patient gets only 5–6 min. As internists and cardiologists work with 15–20 min schedules for an appointment, it enables them to provide better care. However, this is only a hypothesis, and the exact explanation of this phenomenon requires further studies which also include patient characteristics.
Due to the fact that the observation periods lasted for more than 4 years, we were able to analyse the long-term variability of blood pressure values. We have demonstrated a marked, 5/2 mmHg seasonal difference between the average systolic and diastolic blood pressure with higher values in winter and lower values in summer. These findings are in line with the study of Lewington S. et al. who found a 10 mmHg difference in systolic blood pressure between summer and winter in the China Kadoorie Biobank study on 506,673 adults [Citation15]. Western European data are also available by Alpérovich et al. who showed a difference of 8 mmHg in systolic blood pressure in the 4 seasons between the lowest and the highest temperature quintiles in 8801 subjects of three French cities [Citation16]. Brennan et al. provided data as early as in 1982 that with a 20 °C difference in daily maximal temperature, blood pressure can vary with 4–6 mmHg, increasingly more so with age [Citation6]. The results of our study confirm that seasonal blood pressure variability is an important phenomenon in Central Europe as well. This fact is of particular clinical importance, as taking into account the adaptation of antihypertensive medications to seasonal climate changes can help to optimise the care of hypertensive patients.
This study has some limitations. As the registry has only blood pressure and heart rate data, no clinical information was available on the subjects measured. Additionally, although the physicians and assistants were asked to use the provided device, it cannot be excluded that other devices were also used during the measurement periods for blood pressure evaluation which data were not uploaded into the register. Moreover, environmental temperature data were not collected in the study period so the exact contribution of temperature differences to blood pressure variability could not have been calculated. Finally, due to the large amount of data, the proportion of recommendation-based repeated measurements in 1-min intervals was not analysed; however, the low number of average daily measurements suggests that only a few of them were repeated ones.
In conclusion, the low daily average number of blood pressure measurements indicates a limited blood pressure screening awareness/capacity in the case of Hungarian family physicians. In practices with more patients, blood pressure is generally less well-controlled. These results suggest that the further promotion of home blood pressure measurement is necessary. The marked seasonal blood pressure changes demonstrated by this study requires further attention in order to identify the optimal medical treatment.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Rahimi K, Bidel Z, Nazardazeh M, et al. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397(10285):1–8.
- Piepoli MF, Hoes AW, Agewall S, et al. European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts)developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–2381. 2016 doi: 10.1093/eurheartj/ehw106.
- Williams B, Mancia G, Spiering W, et al. ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953–2041. doi: 10.1097/HJH.0000000000001940.
- Mancia G, Kreutz R, Brunström M, et al. ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41(12):1874–2071. 2023 doi: 10.1097/HJH.0000000000003480.
- Stergiou GS, Palatini P, Parati G, et al. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1293–1302. doi: 10.1097/HJH.0000000000002843.
- Brennan PJ, Greenberg G, Miall WE, et al. Seasonal variation in arterial blood pressure. Br Med J. 1982;285(6346):919–923. doi: 10.1136/bmj.285.6346.919.
- Járai Z, Nemcsik J, Páll D. Office blood pressure measurements in Hungary: 3 year results of an open label, prospective, observational study. J Hypertension. 2022;40(Suppl 1):e100. doi: 10.1097/01.hjh.0000836228.93352.fe.
- Központi Statisztikai Hivatal (Hungarian Central Statistical Office). Data on file. 2023. https://www.ksh.hu/stadat_files/ege/hu/ege0007.html.
- Beger C, Mayerböck A, Klein K, et al. Current practice of blood pressure measurement in Germany: a nationwide questionnaire-based survey in medical practices. Blood Press. 2023;32(1):2165901. doi: 10.1080/08037051.2023.2165901.
- Ozone S, Sato M, Takayashiki A, et al. Adherence to blood pressure measurement guidelines in long-term care facilities: a cross sectional study. J Gen Fam Med. 2018;19(3):97–101. doi: 10.1002/jgf2.162.
- Woolsey S, Brown B, Ralls B, et al. Diagnosing hypertension in primary care clinics according to current guidelines. J Am Board Fam Med. 2017;30(2):170–177. doi: 10.3122/jabfm.2017.02.160111.
- Nemcsik J, Páll D, Ábrahám G, et al. May measurement month 2017: an analysis of blood pressure screening in Hungary-Europe. Eur Heart J Suppl. 2019;21(Suppl D):D56–d58. doi: 10.1093/eurheartj/suz054.
- Nemcsik J, Páll D, Nemes-Nagy Z, et al. May measurement month 2019: an analysis of blood pressure screening results from Hungary. Eur Heart J Suppl. 2021;23(Suppl B):B70–b72. doi: 10.1093/eurheartj/suab025.
- Sala C, Santin E, Rescaldani M, et al. How long shall the patient rest before clinic blood pressure measurement? Am J Hypertens. 2006;19(7):713–717. doi: 10.1016/j.amjhyper.2005.08.021.
- Lewington S, Li L, Sherliker P, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens. 2012;30(7):1383–1391. doi: 10.1097/HJH.0b013e32835465b5.
- Alpérovitch A, Lacombe J-M, Hanon O, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the three-city study. Arch Intern Med. 2009;169(1):75–80. doi: 10.1001/archinternmed.2008.512.