ABSTRACT
This study was designed to investigate the correlation of neutrophil/lymphocyte ratio (NLR), platelet/lymphocyte ratio (PLR), and interleukin (IL)-37/IL-17 ratio with the incidence/treatment of rheumatoid arthritis (RA). Firstly, fifty-eight patients with RA treated at the first affiliated hospital of Xinjiang Medical University from January 2018 to January 2019 were selected as the RA group; forty-nine healthy volunteers were enrolled in the control group. RA patients were treated with disease-modifying anti-rheumatic drugs (DMARDs). Next, the NLR, PLR, IL-37, IL-17 and 28-joint disease activity score using erythrocyte sedimentation rate (DAS28-ESR) were deleted in two groups. Subsequently, Spearman correlation analysis was adopted for the correlations of various indicators before and after treatment in two groups. According to the analysis results, the levels of NLR, PLR, IL-37, and IL-17 before treatment in the RA group were higher than those in the control group (P < .05), but the difference in the IL-37/IL-17 level between the two groups was not significant (P > .05). After treatment, NLR, PLR, and IL-37/IL-17 levels were significantly reduced in RA patients (P < .05). NLR and PLR were significantly positively correlated with DAS28-ESR, ESR and C-reactive protein (CRP), of which represented the disease activity of RA. NLP was strongly correlated with IL-37/IL-17. Collectively, NLR, PLR, IL-37, and IL-17 are closely related to the occurrence of RA. In addition, NLR and IL-37/IL-17 are more suitable than PLR in reflecting the therapeutic effect. Therefore, IL-37/IL-17 can be considered as a new indicator for reflecting the treatment effectiveness of RA.
Introduction
Rheumatoid arthritis (RA) is a long-term autoimmune disease associated with progressive disability, systemic complications, early death, and socioeconomic costs (Glant et al., Citation2014; Scott et al., Citation2010). Clinically, RA is characterized by polyarticular, symmetrical and invasive arthritis of the small joints of hands and feet, often accompanied by involvement of extra-articular organs and positive serum rheumatoid factor (RF). Chronic inflammation in the joints is usually a continuous, recurrent process, which is manifested as vascular inflammation, subcutaneous nodules, neurological tissue lesions, and stiffness and swelling of the limbs. The total number of RA patients in China has reached more than four million with peak age around 30–50 years, and the natural life span of RA patients has been shortened by 5 to 10 years (Firestein & McInnes, Citation2017; Malmstrom et al., Citation2017). At present, the etiology and pathogenesis of RA are relatively complex and remain to be explained completely.
It was well known that RA is characterized with increased burden of inflammation (Cakır et al., Citation2016). Currently, the T-lymphocyte-mediated inflammation is an important inflammatory factor that induces RA. The role of neutrophils, platelets, neutrophil/lymphocyte ratio (NLR), and platelet/lymphocyte ratio (PLR) associated with inflammatory response in RA have received widespread attentions in recent years (Boilard et al., Citation2010; Qi et al., Citation2016; Steiner & Smolen, Citation2002). PLR has been introduced as a novel hemogram-derived inflammatory index in various conditions, such as thyroiditis (Erge et al., Citation2023) and other thyroid conditions (Afsin & Aktas, Citation2021), gastrointestinal diseases (Buse Balci & Aktas, Citation2022), cancers (Atak et al., Citation2021), diabetes mellitus (Atak et al., Citation2019), and irritable bowel disease (Aktaş et al., Citation2020). Moreover, increased NLR has been noted in inflammatory disorders, such as inflammatory bowel disease (Posul et al., Citation2015), gastrointestinal diseases (Buse Balci & Aktas, Citation2022), cardiac conditions (Şahin et al., Citation2013), and thyroiditis (Aktas et al., Citation2017). In addition, interleukin (IL)-37 and IL-7 were reported to be related to inflammation inhibition (Dinarello et al., Citation2016; Shabgah et al., Citation2014).
Early diagnosis and treatment based on indicators such as joint function scores and inflammatory reactants, are the main strategies to prevent the development of joint dysfunction (Lin et al., Citation2020). However, due to the lack of more specific indicators for monitoring the development and treatment efficacy of RA, the process of RA is rather difficult to control, and the teratogenic rate remains very high, which seriously affects the life quality of patients. Therefore, it is urgent to explore the diagnostic and therapeutic indicators of RA.
Recent studies have revealed that NLR and PLR levels are closely related to inflammatory responses, including diseases such as RA (Jung et al., Citation2019), malignant tumors (Rajwa et al., Citation2018), myocardial infarction (Sun et al., Citation2018), and Henoch-Schonlein purpura (Makay et al., Citation2014). However, the role of NLR and PLR levels in the progression and treatment efficacy of RA has been rarely investigated. In addition, IL-37, as a novel anti-inflammatory cytokine, was up-regulated in a variety of autoimmune diseases, chronic infections and tumors according to previous studies (Boraschi et al., Citation2011; Nold et al., Citation2010). As for IL-17 factor, it can mediate inflammatory cells to infiltrate joints (Kolls & Lindén, Citation2004). Thus, the IL-37, IL-17 or IL-37/IL-17 levels might be associated with the progression or treatment effects of RA, and this has been rarely investigated so far. Therefore, this study intended to investigate the correlation of the related indicators (NLR, PLR, IL-37, IL-17 and IL-37/IL-17 etc.) with the development and treatment of RA. We analyzed the difference of these indicators between healthy individuals and RA patients (before and after treatment). We found that NLR and IL-37/IL-17 could reflect the therapeutic effect of RA by correlation analysis. Our study may contribute to the prediction and treatment of RA patients.
Materials and methods
Patients
The case data were derived from patients treated at the first affiliated hospital of Xinjiang Medical University from January 2018 to January 2019. A total of 58 patients with active RA were randomly selected as RA group, and 49 healthy volunteers who received health examinations at the same hospital were selected as control group. The inclusion criteria of RA patients were shown as follow: 1) all patients met the diagnostic criteria for RA (RA diagnostic criteria of American Rheumatology Association 2010); 2) patients suffered from highly active period of RA, and the 28-joint disease activity score using erythrocyte sedimentation rate (DAS28-ESR) was higher than 5.5. Exclusion criteria were listed as follows: patients had 1) upper respiratory tract infection, urinary system infection, tuberculosis and other infections that may affect the research results; 2) previous knee infection, joint tuberculosis, or history of surgery; 3) poor treatment effects. The blood sample of RA patients was collected before and after treatment; healthy volunteers were collected the blood sample once at the start of enrollment. This study was approved by Ethics Committee of First Affiliated Hospital of Xinjiang Medical University (Ethical approval number: 20171223-K01). All individual participants included in the study were informed consent.
Intervention
All RA patients received disease-modifying anti-rheumatic drugs (DMARDs). Patients were treated by methotrexate combined with another DMARD (such as leflunomide, tripterygium wilfordii or iguratimod).
Measurement indicators
DAS28-ESR
DAS28-ESR is an effective reference for evaluating the activity of RA (Sharif et al., Citation2018). The detailed evaluation included following four parts: 1) the number of tender joints; 2) number of swollen joints; 3) erythrocyte sedimentation rate (ESR, mm/hour) (Westergren Methods); 4) overall health status evaluation (0–100 points). DAS28-ESR score = 0.56 * sqrt (1) + 0.28 * sqrt (2) + 0.70 * ln (3) + 0.014 * (4). According to the DAS28-ESR criteria, DAS28 < 2.6 indicated remission, 3.2 < DAS28 < 5.1 represented active status, and DAS28 > 5.1 indicated high active status of disease.
NLR and PLR measurement
Peripheral venous blood (2 ml) was collected from patients in the morning. The neutrophils, platelets and lymphocyte were detected by using coulter counter instruments (Beckman Coulter, Brea, California, USA). Next, the NLR and PLR values were calculated.
Measurement of IL-37, IL-17, and IL-37/IL-17 ratio, anti-CCP and CRP
Enzyme-linked immunosorbent assay (ELISA) kit (Sigma, USA) were used to detect the level of IL-37, IL-17 and anti-cyclic citrullinated peptide (anti-CCP) in peripheral venous blood. Briefly, the IL-37, IL-17 and anti-CCP levels were measured using a Tecan Freedom Evolyzer-2200 automatic enzyme immunoassay analyze (Switzerland). Then, the IL-37/IL-17 ratio was calculated. After that, the standard curve was drawn through the absorbance value of the standard samples. The values of actual experimental samples were then calculated based on the standard curve. Additionally, C-reactive protein (CRP) were detected by turbidimetric scattering method.
Statistical analysis
SPSS and R software were responsible for data processing. Count data were expressed as % and analyzed through Chi-square test. Kolmogorov-Smirnov normality test was performed to check the normality of data. The measurement data with a normal distribution were expressed as mean ± standard deviation (SD), and the difference between the two groups were compared with t-test, analysis of variance and LSD-t test. Data with a skewed distribution were expressed as median (quartile), and Mann-Whitney U test were used to analyze the differences between the two groups. Spearman correlation analysis was employed to measure the correlation between two variables. P < .05 indicated a significant difference.
Results
Comparison of baseline baseline data and related indicators between the RA group and control group
Firstly, we compared the baseline data and related indicators between RA patients and healthy individuals. As shown in , there were no significant differences in age and gender between these two groups (P > .05). The average disease duration for RA patients was 20.97 ± 0.75 months. Besides, the levels of most of related indicators (ESR, CRP, neutrophil count, platelet count, RF, anti-CCP, IL-37, IL-17, NLR, and PLR) in RA patient were higher than those in healthy individuals (P < .01). Notably, there was no significant difference in the IL-37/IL-17 ratio between the two groups. A total of 6 months were taken from the treatment to the assessment of the blood.
Table 1. Comparison of baseline data and main indicators between the two groups.
Comparison of related indicators before and after treatment of RA
To find the indicators reflecting the treatment efficacy, the possible indicators related to RA were compared in RA patients before and after treatment. As shown in , the DAS28-ESR, ESR, CRP, RF, neutrophil count, platelet count, IL-17, IL-37, NLR, PLR and IL-37/IL-17 levels were significantly decreased in the RA group after treatment (P < .01).
Table 2. Comparison of relevant indicators before and after RA treatment.
Further, NLR, PLR and IL-37/IL-17 were compared and shown in . It could be observed that the levels of NLR and PLR in RA patients were notably reduced upon six months of treatment (P < .01), but those in the control group were not significantly different (P > .05). Notably, IL-37/IL-17 was significantly decreased in RA patients after treatment (P < .01). Moreover, compared with the control group, the IL-37/IL-17 was markedly lower in RA patients receiving treatment (P < .01).
Figure 1. Comparison of rheumatoid arthritis (RA) with NLR, PLR and IL-37/IL-17 in RA group before/after treatment and control group. R software was adopted for analysis and mapping. Abbreviation: IL-17, interleukin-17; IL-37, interleukin-37; NLR, neutrophil/lymphocyte ratio; PLR, platelet/lymphocyte ratio.

Pairwise correlation analyses among the related indicators in RA patients
Subsequently, we analyzed the correlation between the treatment efficacy and related indicators in RA patients. The results showed that NLR (r = −0.785), PLR (r = −0.357) and IL-37/IL-17 (r = −0.766) were all negatively correlated with the grouping (before and after treatment) (). Moreover, NLR, PLR, and IL-37/IL-17 were positively correlated with DAS28-ESR, ESR and CRP, of which represented the disease activity of RA (). Among these three indicator, NLR was strongly correlated with DAS28-ESR, ESR and CRP (r > 0.6, ). Hence, NLR and IL-37/IL-17 would be more suitable in reflecting the therapeutic effect of RA than PLR. In addition, as displayed in , PLR, NLP and IL-37/IL-17 were positively correlated with each other, while there was no significant difference in the correlation between PLR and IL-37/IL-17.
Figure 2. Correlation among NLR, PLR, IL-37/IL-17 and DAS28-ESR. The correlation analysis and mapping were carried out using R software. P < .05 indicated a significant difference. Abbreviation: DAS28-ESR, 28-joint disease activity score using erythrocyte sedimentation rate; IL-17, interleukin-17; IL-37, interleukin-37; NLR, neutrophil/lymphocyte ratio; PLR, platelet/lymphocyte ratio.
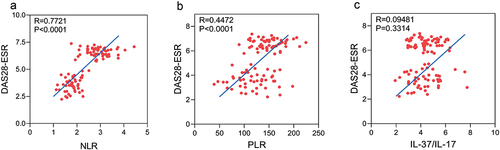
Figure 3. Correlation among NLR, PLR and IL-37/IL-17. The correlation analysis and mapping were carried out by using R software. Differences were considered statistically significant at P < .05. Abbreviation: IL-17, interleukin-17; IL-37, interleukin-37; NLR, neutrophil/lymphocyte ratio; PLR, platelet/lymphocyte ratio.
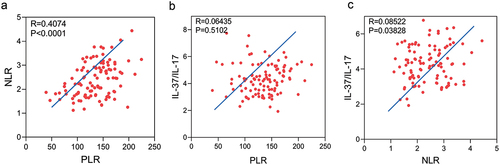
Table 3. Pairwise correlation of indicators in RA group.
Discussion
RA is considered to be one of the most representative autoimmune diseases. Current studies have shown that antigen-driven, lymphocyte-mediated, genetic and environmental factors are involved in the occurrence and development of RA (Gibofsky, Citation2014; Sharif et al., Citation2018). Until now, few indicators have been developed for monitoring the occurrence and development of RA. Cytokines [such as IL-1, IL-2, IL-3, IL- 4, IL-6, IL-8, interferon (IFN) and tumor necrosis factor-ɑ (TNF-ɑ), etc.] play an important role in the pathogenesis of RA (Shuang et al., Citation2019). IL-37 is a new member of the IL-1 cytokine family, which serves as a key cytokine regulating inflammation and involves in the immune response in vivo (Conti et al., Citation2017; Mastrangelo et al., Citation2018; Song et al., Citation2018). IL-17 and TNF-ɑ usually participates in unfavourable prognosis of RA simultaneously. IL-17 combined with TNF-ɑ can synergistically promote the synthesis of prostaglandin E (PGE) by osteoblasts and chondrocytes, stimulate the secretion of cytokines by synovial cells, and increase joint cartilage damage. Zhao et al., (Citation2014) found that IL-37 and IL-17 levels were highly expressed in RA patients and positively correlated. Our data showed that the IL-37 and IL-17 levels were higher in RA patients than healthy volunteers, and after treatment, the IL-37 and IL-17 levels were decreased in RA patients. It is consistent with previous research. However, numerous studies showed that IL-37 can severely inhibit many inflammatory cytokines, such as IL-1, IL-6, interferon-γ (IFN-γ), TNF-a, etc (Charrad et al., Citation2016; Yang et al., Citation2015; Ye et al., Citation2014). Recently, it was reported that IL-37 can inhibit the proliferation of T-helper 17 cells through decreasing the level of cytokine IL-17 in cells, thereby alleviating the disease activity of RA (Ye et al., Citation2014). The IL-37 and IL-17 levels in the development and treatment of RA still need further investigations.
Inspired by the previous studies, we speculated that the ratio of IL-37/IL-17 might be associated with changes in RA condition. Both IL-37 and IL-17 were increased during initial stage of RA, while IL-37 could decrease the levels of IL-17, resulting in a high IL-37/IL-17 ratio. After effective treatments, the levels of IL-37 in RA patients would fall off, and the levels of IL-17 would rebound partially, leading to a decline in IL-37/IL-17 ratio. Our results confirmed that the IL-37/IL-17 was decreased after treatment in RA patients. But there was no significant difference in IL-37/IL-17 ratio between RA patients and healthy individuals.
In addition, some studies have revealed that NLR and PLR levels are related to RA disease activity (Chandrashekara et al., Citation2017; Sargin et al., Citation2018). However, Jung et al. (Jung et al., Citation2019) found that NLR and PLR were associated with disease activity in polymyalgia rheumatica, and could not predict prognosis in patients with RA. Therefore, the role of NLR and PLR in RA disease activity remains controversial.
In this study, we investigated whether NLR, PLR, and IL-37/IL-17 ratio are relevant to the occurrence and treatment of RA. Before treatment, NLR, PLR, IL-37, IL-17, ESR and CRP in RA patients were markedly higher than that in healthy individuals. It was worth mentioning that the difference of IL-37/IL-17 ratio in these two groups was not statistically significant. After six month of treatment, NLR, PLR and IL-37/IL-17 decreased substantially as well as RA activity indicator ESR, CRP and DAS28-ESR, indicating the effectiveness of the treatments. Hence, IL-37/IL-17, NLR and PLR, can be considered as indicators for monitoring the progress and treatment of RA. To further investigate the functions of these indicators, a bi-variate correlation analysis was performed on IL-37/IL-17, NLR and PLR. The analysis result suggested that NLR and IL-37/IL-17 were more suitable in reflecting the development and treatment of RA, as they exhibited much more positive correlation with ESR, CRP and DAS28-ESR than PLR.
There are several limitations in this study due to the research method. First, the sample size (58 RA patients) of this study is still rather small, especially those cases of treatment failure are not included in this study. In addition, this study mainly represents the characteristics of RA patients treated with biological immunodrugs (TNF-a inhibitors). Our future research direction is to conduct in-depth research on the changes of IL-37/IL-17 in RA at different stages and with different treatments, thereby providing a reference for better RA prediction. In general, IL-37/IL-17, NLR and PLR could serve as monitoring indicators of RA progression and treatment, contributing to promptly assessing the treatment effectiveness and adjusting the strategy to avoid delayed treatment. Overall, this study provided a basis for evaluating the effectiveness in RA patients during DMARD treatment.
Conclusion
Levels of NLR, PLR, IL-37, and IL-17 were related to the occurrence of RA. The level of NLR and IL-37/IL-17 will be more suitable in reflecting the effectiveness of RA treatment than PLR.
Author contributions
Yan Meng and Xiu-min Ma designed experiments; Li Luo and Xuan-lin Cai carried out experiments; Shan Cong and Jiao Sun analyzed the data. Yong-wei Hu and Yan-qin Gu wrote the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work
Ethics approval and consent to participate
This study has been approved by Ethics Committee of First Affiliated Hospital of Xinjiang Medical University (Ethical approval number: 20171223-K01). Informed consent was obtained from all individual participants included in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Afsin, H., & Aktas, G. (2021). Platelet to lymphocyte and neutrophil to lymphocyte ratios are useful in differentiation of thyroid conditions with normal and increased uptake. Ethiopian Journal of Health Development, 35, 149–153. https://www.researchgate.net/publication/354474124_Platelet_to_Lymphocyte_and_Neutrophil_to_Lymphocyte_Ratios_are_useful_in_differentiation_of_thyroid_conditions_with_normal_and_increased_uptake
- Aktaş, G., Duman, T. T., Atak, B., Kurtkulağı, Ö., Bilgin, S., Başaran, E., Demirkol, M. E., & Kösekli, M. A. (2020). Irritable bowel syndrome is associated with novel inflammatory markers derived from hemogram parameters. Family Medicine & Primary Care Review, 22(2), 107–110. https://doi.org/10.5114/fmpcr.2020.95311
- Aktas, G., Sit, M., Dikbas, O., Erkol, H., Altinordu, R., Erkus, E., & Savli, H. (2017). Elevated neutrophil-to-lymphocyte ratio in the diagnosis of hashimoto’s thyroiditis. Revista Da Associação Médica Brasileira, 63, 1065–8. https://doi.org/10.1590/1806-9282.63.12.1065
- Atak, B., Aktas, G., Duman, T. T., Erkus, E., Kocak, M. Z., & Savli, H. (2019). O controle diabético poderia ser predicado por Platelet para a relação de linfócitos no hemograma. Revista da Associação Médica Brasileira, 65(1), 38–42. https://doi.org/10.1590/1806-9282.65.1.38
- Atak, B. M., Kahveci, G. B., Bilgin, S., Kurtkulagi, O., & Kosekli, M. (2021). Platelet to lymphocyte ratio in differentiation of benign and malignant thyroid nodules. Experimental Biomedical Research, 4(2), 148–153. https://doi.org/10.30714/j-ebr.2021267978
- Boilard, E., Nigrovic, P. A., Larabee, K., Watts, G. F., Coblyn, J. S., Weinblatt, M. E., Massarotti, E. M., Remold O’Donnell, E., Farndale, R. W., Ware, J., & Lee, D. M. (2010). Platelets amplify inflammation in arthritis via collagen-dependent microparticle production. Science, 327(5965), 580–3. https://doi.org/10.1126/science.1181928
- Boraschi, D., Lucchesi, D., Hainzl, S., Leitner, M., Maier, E., Mangelberger, D., Oostingh, G. J., Pfaller, T., Pixner, C., Posselt, G., Italiani, P., Nold, M. F., Nold-Petry, C. A., Bufler, P., & Dinarello, C. A. (2011). IL-37: A new anti-inflammatory cytokine of the IL-1 family. European Cytokine Network, 22(3), 127–47. https://doi.org/10.1684/ecn.2011.0288
- Buse Balci, S., & Aktas, G. (2022). A comprehensive review of the role of hemogram derived inflammatory markers in gastrointestinal conditions. Iranian Journal of Colorectal Research, 10, 75–86. https://www.researchgate.net/publication/366399503_A_Comprehensive_Review_of_the_Role_of_Hemogram-derived_Inflammatory_Markers_in_Gastrointestinal_Conditions
- Cakır, L., Aktas, G., Mercimek, O. B., & Enginyurt, O. (2016). Are red cell distribution width and mean platelet volume associated with rheumatoid arthritis. Biomedical Research (Tokyo, Japan), 27, 292–294. https://www.researchgate.net/publication/296656278_Are_Red_Cell_Distribution_Width_and_Mean_Platelet_Volume_associated_with_Rheumatoid_Arthritis
- Chandrashekara, S., Mukhtar Ahmad, M., Renuka, P., Anupama, K. R., & Renuka, K. (2017). Characterization of neutrophil-to-lymphocyte ratio as a measure of inflammation in rheumatoid arthritis. International Journal of Rheumatic Diseases, 20(10), 1457–67. https://doi.org/10.1111/1756-185X.13157
- Charrad, R., Berraïes, A., Hamdi, B., Ammar, J., Hamzaoui, K., & Hamzaoui, A. (2016). Anti-inflammatory activity of IL-37 in asthmatic children: Correlation with inflammatory cytokines TNF-α, IL-β, IL-6 and IL-17A. Immunobiology, 221(2), 182–7. https://doi.org/10.1016/j.imbio.2015.09.009
- Conti, P., Carinci, F., Lessiani, G., Spinas, E., Kritas, S. K., Ronconi, G., Caraffa, A., & Theoharides, T. C. (2017). Potential therapeutic use of IL-37: A key suppressor of innate immunity and allergic immune responses mediated by mast cells. Immunologic Research, 65(5), 982–6. https://doi.org/10.1007/s12026-017-8938-7
- Dinarello, C. A., Nold-Petry, C., Nold, M., Fujita, M., Li, S., Kim, S., & Bufler, P. (2016). Suppression of innate inflammation and immunity by interleukin-37. European Journal of Immunology, 46(5), 1067–81. https://doi.org/10.1002/eji.201545828
- Erge, E., Kiziltunc, C., Balci, S. B., Atak Tel, B. M., Bilgin, S., Duman, T. T., & Aktas, G. (2023). A novel inflammatory marker for the diagnosis of hashimoto’s thyroiditis: Platelet-count-to-lymphocyte-count ratio. Diseases, 11(1), 15. https://doi.org/10.3390/diseases11010015
- Firestein, G. S., & McInnes, I. B. (2017). Immunopathogenesis of rheumatoid arthritis. Immunity, 46(2), 183–96. https://doi.org/10.1016/j.immuni.2017.02.006
- Gibofsky, A. (2014). Epidemiology, pathophysiology, and diagnosis of rheumatoid arthritis: A synopsis. The American Journal of Managed Care, 20(7 Suppl), S128–35.
- Glant, T. T., Mikecz, K., & Rauch, T. A. (2014). Epigenetics in the pathogenesis of rheumatoid arthritis. BMC Medicine, 12(1), 35. https://doi.org/10.1186/1741-7015-12-35
- Jung, J. Y., Lee, E., Suh, C. H., & Kim, H. A. (2019). Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio are associated with disease activity in polymyalgia rheumatica. Journal of Clinical Laboratory Analysis, 33(9), e23000. https://doi.org/10.1002/jcla.23000
- Kolls, J. K., & Lindén, A. (2004). Interleukin-17 family members and inflammation. Immunity, 21(4), 467–76. https://doi.org/10.1016/j.immuni.2004.08.018
- Lin, Y. J., Anzaghe, M., & Schulke, S. (2020). Update on the pathomechanism, diagnosis, and treatment options for rheumatoid arthritis. Cells, 9(4), 880. https://doi.org/10.3390/cells9040880
- Makay, B., Gücenmez, Ö. A., Duman, M., & Ünsal, E. (2014). The relationship of neutrophil-to-lymphocyte ratio with gastrointestinal bleeding in Henoch–Schonlein purpura. Rheumatology International, 34(9), 1323–1327. https://doi.org/10.1007/s00296-014-2986-2
- Malmstrom, V., Catrina, A. I., & Klareskog, L. (2017). The immunopathogenesis of seropositive rheumatoid arthritis: From triggering to targeting. Nature Reviews Immunology, 17(1), 60–75. https://doi.org/10.1038/nri.2016.124
- Mastrangelo, F., Frydas, I., Ronconi, G., Kritas, S., Tettamanti, L., Caraffa, A., D Ovidio, C., Younes, A., Gallenga, C., & Conti, P. J. J. B. R. H. A. (2018). Low-grade chronic inflammation mediated by mast cells in fibromyalgia: Role of IL-37. Journal of Biological Regulators and Homeostatic Agents, 32(2), 195–198.
- Nold, M. F., Nold-Petry, C. A., Zepp, J. A., Palmer, B. E., Bufler, P., & Dinarello, C. A. (2010). IL-37 is a fundamental inhibitor of innate immunity. Nature Immunology, 11(11), 1014–22. https://doi.org/10.1038/ni.1944
- Posul, E., Yilmaz, B., Aktas, G., & Kurt, M. (2015). Sagt der Neutrophilen/Lymphozyten Quotient die Aktivität einer Colitis ulcerosa voraus? Wiener klinische Wochenschrift, 127(7–8), 262–5. https://doi.org/10.1007/s00508-014-0683-5
- Qi, L., Zhang, X., & Wang, X. (2016). Heparin inhibits the inflammation and proliferation of human rheumatoid arthritis fibroblast-like synoviocytes through the NF-κB pathway. Molecular Medicine Reports, 14(4), 3743–3748. https://doi.org/10.3892/mmr.2016.5719
- Rajwa, P., Życzkowski, M., Paradysz, A., Bujak, K., & Bryniarski, P. (2018). Evaluation of the prognostic value of LMR, PLR, NLR, and dNLR in urothelial bladder cancer patients treated with radical cystectomy. European Review for Medical and Pharmacological Sciences, 22(10), 3027–37. https://doi.org/10.26355/eurrev_201805_15060
- Şahin, Ş., Sarıkaya, S., Alcelik, A., Erdem, A., Tasliyurt, T., Akyol, L., Altunkas, F., Aktas, G., & Karaman, K. (2013). Neutrophil to lymphocyte ratio is a useful predictor of atrial fibrillation in patients with diabetes mellitus. Acta Medica Mediterranea, 29, 847–851. https://www.researchgate.net/publication/289118005_Neutrophil_to_lymphocyte_ratio_is_a_useful_predictor_of_atrial_fibrillation_in_patients_with_diabetes_mellitus
- Sargin, G., Senturk, T., Yavasoglu, I., & Kose, R. (2018). Relationship between neutrophil-lymphocyte, platelet-lymphocyte ratio and disease activity in rheumatoid arthritis treated with rituximab. International Journal of Rheumatic Diseases, 21(12), 2122–7. https://doi.org/10.1111/1756-185X.13400
- Scott, D. L., Wolfe, F., & Huizinga, T. W. J. (2010). Rheumatoid arthritis. The Lancet, 376(9746), 1094–108. https://doi.org/10.1016/S0140-6736(10)60826-4
- Shabgah, A. G., Fattahi, E., & Shahneh, F. Z. (2014). Interleukin-17 in human inflammatory diseases. Postepy Dermatol Alergol, 4, 256–261. https://doi.org/10.5114/pdia.2014.40954
- Sharif, K., Sharif, A., Jumah, F., Oskouian, R., & Tubbs, R. S. (2018). Rheumatoid arthritis in review: Clinical, anatomical, cellular and molecular points of view. Clinical Anatomy, 31(2), 216–223. https://doi.org/10.1002/ca.22980
- Shuang, C., Cheng-Yi, Z., & University B. (2019). Research progress of IL-1, IL-6 and IL-10 in Rheumatoid diseases. World Latest Medicine Information. https://doi.org/10.7507/1002-1892.202012083
- Song, L., Wang, Y., Sui, Y., Sun, J., Li, D., Li, G., Liu, J., Li, T., & Shu, Q. (2018). High interleukin-37 (IL-37) expression and increased mucin-domain containing-3 (TIM-3) on peripheral T cells in patients with rheumatoid arthritis. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 24, 5660–7. https://doi.org/10.12659/MSM.909254
- Steiner, G., & Smolen, J. (2002). Autoantibodies in rheumatoid arthritis and their clinical significance. Arthritis Research, 4(Suppl 2), S1–5. https://doi.org/10.1186/ar551
- Sun, X.-P., Li, J., Zhu, W.-W., Li, D.-B., Chen, H., Li, H.-W., Chen, W.-M., & Hua, Q. J. A. (2018). Platelet to lymphocyte ratio predicts contrast-induced nephropathy in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology, 69(1), 71–78. https://doi.org/10.1177/0003319717707410
- Yang, Y., Zhang, Z.-X., Lian, D., Haig, A., Bhattacharjee, R. N., & Jevnikar, A. M. (2015). IL-37 inhibits IL-18-induced tubular epithelial cell expression of pro-inflammatory cytokines and renal ischemia-reperfusion injury. Kidney International, 87(2), 396–408. https://doi.org/10.1038/ki.2014.295
- Ye, L., Ji, L., Wen, Z., Zhou, Y., Hu, D., Li, Y., Yu, T., Chen, B., Zhang, J., Ding, L., Du, J., & Huang, Z. (2014). IL-37 inhibits the production of inflammatory cytokines in peripheral blood mononuclear cells of patients with systemic lupus erythematosus: Its correlation with disease activity. Journal of Translational Medicine, 12(1), 69. https://doi.org/10.1186/1479-5876-12-69
- Zhao, P.-W., Jiang, W.-G., Wang, L., Jiang, Z.-Y., Shan, Y.-X., Jiang, Y.-F., & Bassaganya-Riera, J. (2014). Plasma levels of IL-37 and correlation with TNF-α, IL-17A, and disease activity during DMARD treatment of rheumatoid arthritis. PLOS ONE, 9(5), e95346. https://doi.org/10.1371/journal.pone.0095346

