ABSTRACT
Purpose
Lacrimal bypass is the creation of a fistula connecting the conjunctiva with the lacrimal sac or nasal cavity. Bypass is indicated in canalicular obstruction or agenesis; sac absence, destruction or prior excision; lacrimal pump failure; or dacryocystorhinostomy failure. We aim to review the various techniques that have been developed over the last century for lacrimal bypass.
Methods
We conducted a comprehensive literature review of techniques which have focused on creating a conduit extending from the conjunctiva or canaliculi to the lacrimal sac, or extending that bypass to the nasal cavity bypass.
Results
The main techniques reviewed include canaliculodacryocystorhinostomy, conjunctivodacryocystostomy, conjunctivorhinostomy, conjunctivodacryocystorhinostomy, and conjunctivoductivodacryocystorhinostomy.
Conclusion
Lacrimal bypass surgery has evolved due to innovation in microsurgical techniques, instruments and materials. Conjunctivodacryocystorhinostomy with Jones tube insertion is the predominant bypass technique, reflecting a culmination of historical developments. Understanding the variety of lacrimal bypass techniques is important for exploring alternative options when necessary.
INTRODUCTION
Lacrimal bypass is the creation of a fistula that connects the conjunctiva directly with the lacrimal sac or nasal cavity.Citation1 This procedure is indicated in cases of canalicular obstruction or agenesis; sac absence, destruction or prior excision; lacrimal pump failure; or dacryocystorhinostomy (DCR) failure. The most common techniques that have influenced those used today were developed over the last century and continue to be refined and modified.
Bypass from Canaliculi to the Nose
One of the earliest lacrimal bypass techniques was canaliculorhinostomy, first described by Arruga in 1935.Citation2 Canaliculorhinostomy was performed following dacryocystectomies where the inferior canaliculus remained intact. At the time, dacryocystectomy was commonly performed for recurrent dacryocystitis.Citation3 In canaliculorhinostomy, an osteotomy was created in the lacrimal sac fossa, then flaps of nasal mucosa were sutured to the tissue surrounding the opening of the canaliculus, then intubated with a plastic tube. However, surgeons at the time noted the canalicular opening would ultimately stenose and alternative techniques were sought.Citation4
Bypass from the Canaliculi to the Sac
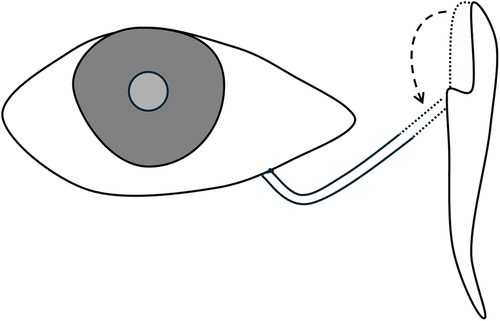
In 1954 Lester Jones described a technique he termed canaliculodacryocystostomy for strictures in the region of the common canaliculus ().Citation5 This technique is also known as canaliculoplasty.Citation6 An LT Jones canaliculodacryocystostomy utilized the lateral half of the lacrimal sac as a tubular flap to connect with the lower canaliculus.Citation5 The use of a flap made from the lacrimal sac is simple compared to other techniques which may involve a vein graft or buccal mucosa wrapped around a polyurethane tube.Citation7–11
Figure 1. LT Jones’ Canaliculodacryocystostomy.
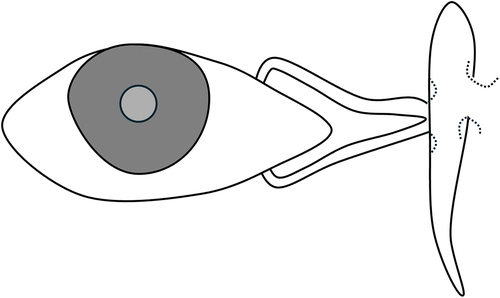
Canaliculodacryocystorhinostomy was developed by Barrie Jones in 1960 to address obstructions of the common canaliculus ().Citation12 The technique involved excision of the medial end of the common canaliculus, anastomosis with the lacrimal sac followed by a rhinostomy.Citation13 Despite a likely patent nasolacrimal duct, a dacryocystorhinostomy would prevent the canaliculi from adhering to the incision on the side of the sac.Citation12 Doucet and Hurwitz also described the use of this technique for individual upper and lower canalicular obstruction with an intact common canaliculus.Citation14 The standard procedure described anterior and posterior anastomoses between the lacrimal sac and nasal mucosa. Rodgers and Hurwitz described an alternative technique that utilized the flap from the sac as the posterior wall of the anastomosis and a nasal flap as the anterior wall.Citation15 Canaliculodacryocystorhinostomy may show a higher success rate in proximal common canalicular obstructions compared to distal canalicular obstructions.Citation16 Another modification was developed whereby a trapdoor opening was made in the fundus of the sac and intubated canaliculi were sutured to the opening.Citation17
Figure 2. BR Jones’ Canaliculodacryocystorhinostomy.
Bypass from the Fornix to the Sac and Nasolacrimal Duct
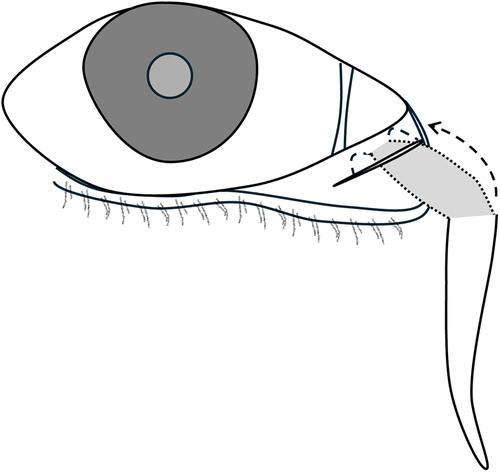
In 1940, the technique of conjunctivodacryocystostomy was described in a paper by Stallard in a case of upper and lower canalicular trauma with a preserved lacrimal sac.Citation18 In Stallard’s operation,Citation19 the lacrimal sac was mobilized from the fossa and brought to the plane of the caruncle (). Orbital fat was allowed to herniate into the lacrimal fossa to support the new position of the sac. The fundus of the sac was incised and the edges sutured to the conjunctival incision edges to create a bypass from the conjunctiva to the lacrimal sac and down into the nasolacrimal duct.Citation18 An advantage of this technique was preservation of the lacrimal bone. However, the long-term success of this technique was not further examined in subsequent studies. Lester Jones transplanted a piece of buccal mucosa into the wall of the new ostium when trauma resulted in deficient epithelium.Citation20 An alternative technique was developed by Chandler in 1975 who dissected but did not mobilize the sac, and instead used a Bowman probe to facilitate the insertion of a tube from the fornix into the sac and nasolacrimal duct to the inferior meatus.Citation6,Citation21,Citation22 Rycroft described a number of disadvantages of the Stallard technique including a) the rarity of a preserved lacrimal sac when both canaliculi are affected, b) difficulty in determining the preoperative patency of the lacrimal sac and nasolacrimal duct, and c) frequent collapse and secondary closure of the conjunctival opening.Citation4 Later, Jones reported that other difficulties included dissecting and mobilizing the lacrimal sac and its fundus, closure of the new ostium without a tube, poor tolerance of tube retention due to the movement of the lids, and unpredictable drainage.Citation23 These issues led to the development of other techniques.
Figure 3. Stallard’s Conjunctivodacryocystostom.
Several techniques describing the creation of a fistula from the conjunctiva to the sac were developed and iterated by different authors. Goar in 1931 incised and created a channel from the fornix to the sac, with repeated probing to epithelialise the tract, though the longevity of this technique was not reported.Citation24 Thiel in 1942 incised a tract between the conjunctiva and lateral wall of the lacrimal sac.Citation25 He then fashioned a tube of buccal mucosa around a tapered instrument, inserting this through the incision. The medial end of the mucosa-lined tube was sutured to the anterior and posterior wound edges of the lateral lacrimal sac wall and the lateral end was sutured to the conjunctiva. An alternative technique was developed by Zarzycki in 1937 who used the term ‘lacodacryocystostomy’.Citation26,Citation27 Zarzycki created a new wound channel from the conjunctiva to the lateral wall of the lacrimal sac by creating a conjunctival ‘tongue’ that was detached from the limbus, then advanced onto the posterior surface of the wound to line the posterior wall of the fistula. Elsching Kraupa furthered this conjunctival tongue by rotating the strip by 180 degrees to create a funnel-like channel.Citation28 Gomez-Marquez also modified this procedure by obtaining a thinner conjunctival tongue attached to the plica semilunaris, which was then attached to a double-armed suture, brought in apposition with the lacrimal sac and then externalised through the skin.Citation29 The conjunctival strip thus lined the anterior wall of the fistula. Bangerter also described his technique of lacrodacryocystostomy in 1944,Citation7 which involved anastomosing flaps between the lacrimal sac and the conjunctiva. A tube of oral mucosa was fashioned to line the fistula from the caruncle to the sac. Bangerter also developed another technique called the ‘lacoductosomy’ for use when the sac was absent.Citation30 This involved an anastomosis between the inferomedial fornix and nasolacrimal duct with an intermediate channel formed again from oral mucosa. Finally, Rycroft described the ‘canthocystostomy’ in a 1951 publication, which was indicated if there was extensive or total occlusion of the lower canaliculus but the upper punctum and canaliculus, lacrimal sac and nasolacrimal duct were intact. The operation involved incising the lateral wall of the lacrimal sac from the entrance of the upper canaliculus down to the opening of the nasolacrimal duct which therefore involved opening the entire lateral wall of the lacrimal sac into the caruncle.Citation4,Citation19
Bypass from the Conjunctival Fornix to the Nose
Similarly, many techniques have been described in creating a fistula from the conjunctiva to the nose. Stallard and Rycroft described a technique of canthorhinostomy, indicated when neither canaliculi nor sac were available.Citation31 The procedure involved connecting the nasal cavity with the conjunctiva,Citation19 where a section of a large vein or inverted buccal mucosa covering a piece of polyethylene tubing, was sutured into an opening made inferior and posterior to the medial palpebral ligament attachment. Jones and Boyden further modified their technique by utilizing a pedicled flap of nasal mucosa to line the surgical ostium.Citation5 Murube Del Castillo developed a less invasive technique of subcutaneous conjunctivorhinostomy which avoided the need for an osteotomy.Citation32 A pointed clamp was inserted into the nose, passed subcutaneously in front of the maxilla, and directed to the lower fornix where it would appear immediately beneath the lower punctum. The tract was kept patent by a silicone-encased glass tube or hydrophilic silicone tube, allowing tears to drain into the nose. Further, Murube Del Castillo described a version of conjunctivorhinostomy, termed ‘dacryo-fornix-rhinostomy’ in 1992.Citation33 A cranially pedicled nasal mucosal flap extending from the orbital rim to the nasal valve area was fashioned, externalized, and divided into two parts for reconstruction of the posterior wall and anterior wall of the passage between the conjunctiva and nose. The flaps were sutured to the corresponding posterior and anterior lip of the conjunctival incision and stented. In a similar fashion a new conduit was created from combined conjunctival and nasal flaps by Arden (1990),Citation34 and Huang (1992).Citation35 A technique using conjunctival and cartilage-containing nasal flap was developed by Walter in 1997.Citation36 In this technique, the cartilage provided autologous stenting of the posterior wall adjacent to the osseous perforation, a critical region for restenosis. Further modifications were made by Bhattacharjee who sutured the labial mucosal graft to the surrounding orbicularis oculi muscle.Citation37
The technique of conjunctivodacryocystorhinostomy is sometimes attributed to Von Hoffmann in 1904.Citation38 His technique was more consistent with a canaliculotomy or wedge excision of posterior lip of the canaliculus, in which the lower lip of the wound was excised to create a gutter for tear drainage.Citation39 This gutter may extend to the sac forming the cystostomy. In fact, conjunctivodacryocystorhinostomy with a Pyrex glass tube was developed in 1960 by Lester Jones ().Citation23,Citation40 This technique revolutionized lacrimal bypass surgery and continues to be used today, though with ongoing modifications and refinements. The originally reported indications of the technique included congenital absence, traumatic destruction, or complete closure of the upper and lower canaliculi; closure of ≥2 mm of the distal ends of the canaliculi; following an unsuccessful dacryocystorhinostomy, and cases secondary to permanent paralysis of the lacrimal pump such as facial nerve palsy. The technique involves creating a fistula from the conjunctival fornix through to the nasal cavity, therefore bypassing the lacrimal sac with the insertion of a plastic or glass tube. Polyethylene tubes were in frequent use before the development of Pyrex glass tubes.Citation41
Figure 4. LT Jones’ Conjunctivodacryocystorhinostomy with Jones tube.
The original technique involved an external approach. Endoscopic endonasal techniques have since been developed.Citation42,Citation43 There have been several variations on the types of tubes used. Important examples include the Gladstone Putterman tube (Pyrex glass tube with secondary flange to reduce recurrent extrusion),Citation44 and the Ipswich tube (tube fashioned from nasal septal mucosa).Citation45 Other fistula lining techniques have been described such as buccal mucosa,Citation8,Citation46 venous grafting,Citation11 superficial temporal artery,Citation47,Citation48 and fascial flap wrapped around buccal mucosa.Citation49,Citation50 There have also been refinements in the detail of various surgical steps developed since the first description which are detailed elsewhere.Citation1,Citation51 Schwarcz et al. described an approach where an incision was made in the inferior conjunctival fornix, preserving the caruncle, and a tube was directed through the conjunctival fornix directly into the lateral nasal wall following an osteotomy.Citation52
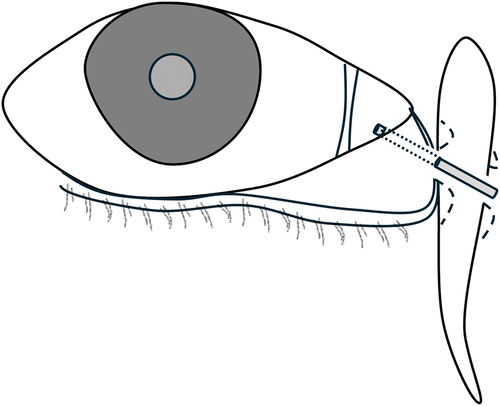
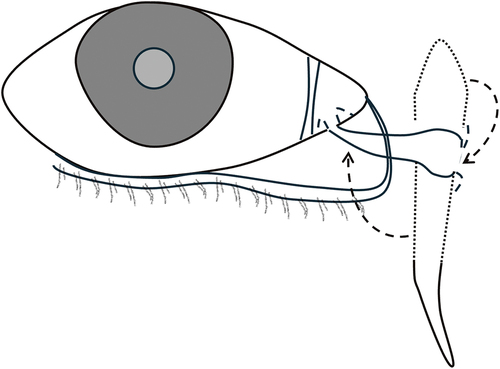
More recently in 2022, Ushio et al. described the technique of conjunctivoductivodacryocystorhinostomy. This approach involves the creation of an anastomosis between the conjunctiva and nasolacrimal duct by rotating the lacrimal sac laterally by 90 degrees, such that the duct would be in apposition with the conjunctiva and the lacrimal sac fundus would be opened to allow drainage of tears directly into the nasal cavity ().Citation53 The technique was developed to address postoperative scarring encountered with other techniques and the various complications associated with Jones tubes including burden of follow up, tube migration and extrusion.Citation54 The technique begins as a dacryocystorhinostomy, but the lacrimal sac requires complete mobilization up to the fundus, which may be difficult to achieve from a purely endonasal approach particularly following prior trauma or medial canthus surgery. The severed end of the nasolacrimal duct is brought up to the conjunctiva and sutured in place as a new conduit between the caruncle and the sac. The lacrimal sac wall is then opened to allow direct communication of the new pathway into the nasal cavity. The authors report that the advantages include avoidance of canaliculoplasty, foregoing the need for a semi-permanent tube such as Jones tube and the absence of skin incision. However, the technique cannot be used in the presence of nasolacrimal duct obstruction.
Figure 5. Conjunctivoductivodacryocystorhinostomy.
Other Bypass Techniques
Less common techniques have been described in case reports although have not been popularized as those mentioned previously. Bennett et al. described in 1959 the technique of conjunctivoantrorhinostomy. When parotid gland transplantation was performed for xerophthalmia,Citation55 there was a need for addressing subsequent high tear volume. In conjunctivoantrorhinostomy, an opening was made from the inferior conjunctival sac into the maxillary antrum then into the posterior aspect of the nasal cavity. The tears were therefore drained via gravity.Citation56 Although conjunctivodacryocystorhinostomy with a larger diameter Pyrex tube can accommodate higher tear volumes and is often preferred,Citation23 a lacosinuostomy has been used in cases of neoplastic invasion of the medial canthus.Citation57
CONCLUSION
In conclusion, modern lacrimal bypass surgery has evolved over the last century due to advances in microsurgical techniques, instrumentation, and materials. Of all these techniques, conjunctivodacryocystorhinostomy with Jones tube insertion has become the dominant lacrimal bypass technique. An understanding of the historical developments that led to this technique is important to continue the pioneering of alternative options when needed.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the author(s).
Additional information
Funding
REFERENCES
- Athanasiov PA, Madge S, Kakizaki H, Selva D. A review of bypass tubes for proximal lacrimal drainage obstruction. Surv Ophthalmol. 2011;56(3):252–266. doi:10.1016/j.survophthal.2011.02.009.
- Arruga H. Heilung des Tränens in Fällen, wo früher der Tränensack schon exstirpiert wurde. Klin Monatsbl Augenheilkd. 1935;95:613–620.
- Harish V, Benger RS. Origins of lacrimal surgery, and evolution of dacryocystorhinostomy to the present. Clin Exp Ophthalmol. 2014;42(3):284–287. doi:10.1111/ceo.12161.
- Rycroft BW. Surgery of external rhinostomy operations. Br J Ophthalmol. 1951;35(6):328–338. doi:10.1136/bjo.35.6.328.
- LT J. Epiphora: Its causes and new surgical procedures for its cure*: A preliminary report. Am J Ophthalmol. 1954;38(6):824–831. doi:10.1016/0002-9394(54)90412-2.
- Hofmann H, Hanselmayer H. Operations on the lacrimal system. In: Blodi F, Mackensen G, and Neubauer H, eds. Surgical Ophthalmology. Berlin, Heidelberg: Springer, 1991:Vol. 1, 253–259.
- Bangerter A. Zur Behandlung bei Tränenröhrchenstenose. Ophthalmologica. 2010;114(4–5):195–202. doi:10.1159/000300469.
- Campbell CB, Shannon GM, Flanagan JC. Conjunctivodacryocystorhinostomy with Mucous Membrane Graft. Vol. 14. NJ:SLACK Incorporated Thorofare; 1983.
- HANNA DC, CLAIRMONT AA. Nasolacrimal duct reconstruction with a vein graft: a noninvasive technique. Plast Reconstr Surg. 1978;62(1):85–88. doi:10.1097/00006534-197807000-00012.
- Paufique L, Durand L. Surgical treatment of eye watering: Repair of the canaliculus with a venous graft (technic). Annales d’oculistique. 1969;202(4):337–44.
- Soll DB. Vein Grafting in Nasolacrimal System Reconstruction. Vol. 14. NJ:SLACK Incorporated Thorofare; 1983.
- Jones B. The surgical cure of obstruction in the common lacrimal canaliculus. Trans Ophthalmol Soc UK. 1960;80:343–359.
- Jones B. Principles of lacrimal surgery. Trans. Ophthalmol. Soc. U.K. 1973;93(00):611–618.
- Doucet TW, Hurwitz JJ. Canaliculodacryocystorhinostomy in the treatment of canalicular obstruction. Arch Ophthalmol. 1982;100(2):306–309. doi:10.1001/archopht.1982.01030030308017.
- Rodgers KJA, Hurwitz JJ. A simplified canaliculodacryocystorhinostomy. Orbit. 1983;2(4):231–234. doi:10.3109/01676838309019189.
- Quaranta-Leoni FM, Fiorino MG, Serricchio F, Quaranta-Leoni F. Management of proximal lacrimal obstructions: a rationale. Acta Ophthalmol. 2021;99(4):e569–e75. doi:10.1111/aos.14632.
- Busse H, Hollwich F. ERKRANKUNGEN DER ABLEITENDEN TRAENENWEGE UND IHRE BEHANDLUNG. 1978.
- Stallard H. An operation for epiphora. Lancet. 1940;236(6120):743–744. doi:10.1016/S0140-6736(00)92077-4.
- HB S. Eye Surgery H.B. Stallard: John Wright & Sons; 1965.
- Jones LE. II. Its relation to the anatomic structures and surgery of the medial canthal region. Am J Ophthalmol. 1957;43(2):203–212. doi:10.1016/0002-9394(57)92911-2.
- Chandler AC. Modifications of the conjunctivodacryocystostomy procedure. Am J Ophthalmol. 1975;80(3 Pt 2):522–524. doi:10.1016/0002-9394(75)90220-2.
- Chandler AC, Wadsworth JAC. Conjunctivodacryocystostomy. Am J Ophthalmol. 1974;77(6):830–836. doi:10.1016/0002-9394(74)90386-9.
- Jones LT. Conjunctivodacryocystorhinostomy. Am J Ophthalmol. 1965;59(5):773–783. doi:10.1016/0002-9394(65)93004-7.
- GOAR EL. CONGENITAL ABSENCE of the LACRIMAL PUNCTA and of the CANALICULI. Arch Ophthalmol. 1931;6(5):724–730. doi:10.1001/archopht.1931.00820070753007.
- Thiel R. Zur Wiederherstellungschirurgie der Tranenwege. Klin Mbl Augenheilk. 1942;108:576.
- Walser E. Plastische Chirurgie am Auge. Munich: J.F. Bergmann-Verlag; 2012.
- Zarzycki P. La lacodacryocystostomie. Bull Soc Opht Paris. 1937;49:9–12.
- KRAUPA E. Die angeborene Atresie der Tranenwege und ihre operative Behandlung. Klin Mbl Augenheilk. 1910;48.
- GOMEZ-MARQUEZ. Contribución a la dacriocistorrinostomía. Arch Oftal B Aires. 1927;25:473–488.
- Huber P, Benz G. Verlaufskontrollen und Spätresultate nach operativer Behandlung praesaccaler Dakryostenosen. Ophthalmologica. 1970;161(2–3):313–323. doi:10.1159/000306130.
- HINE P-M. Sectional Proceedings of the Royal Society of Medicine Vol. XLIII. Proceedings of the Royal Society of Medicine, Western Ophthalmic Hospital, London, UK; 43:25.
- Murube-Del-Castillo J. Conjunctivorhinostomy without osteal perforation. Arch Ophthalmol. 1982;100(2):310–311. doi:10.1001/archopht.1982.01030030312018.
- Del Castillo J M, Martinez Baradas A, Hernandez King J, et al. Dacryo-fornix-rhinostomy with two flaps. Eur J Ophthalmol. 1992;2(2):73–78. doi:10.1177/112067219200200204.
- Arden RL, Mathog RH, Nesi FA. Flap Reconstruction Techniques in Conjunctivorhinostomy. Otolaryngol Head Neck Surg. 1990;102(2):150–155. doi:10.1177/019459989010200209.
- Huang TT, Sasaki K, Nozaki M. Reconstruction of the lacrimal excretory system. Plast Reconstr Surg. 1992;90(3):399–404. doi:10.1097/00006534-199209000-00006.
- Walter C. Plastisch-chirurgische Eingriffe im Kopf-Hals-Bereich. Stuttgart, Germany: Thieme Stuttgart; 1997.
- Bhattacharjee K, Singh M, Shrivastava R, et al. Long-term outcomes of labial mucosal graft in conjunctivo-rhinostomy surgery. Can J Ophthalmol. 2019;54(2):258–264. doi:10.1016/j.jcjo.2018.05.002.
- Hoffmann V. Keilförmige Excision (eines Schleimhautstückchens) eine Verbesserung der Bowmanschen Schlitzung. Congr Internat Opht. 1904:41–46.
- OPHTHALMOLOGICAL I, Lucerne GJ. Dixième Congrès international d’ophtalmologie, Lucerne … 1904. Compte rendu publié par le Comité d’organisation avec le concours du Dr J. Gonin1905. 1904;B41–B46.
- JONES LT. An anatomical approach to problems of the eyelids and lacrimal apparatus. Arch Ophthalmol. 1961;66(1):111–124. doi:10.1001/archopht.1961.00960010113025.
- Henderson JW. Management of strictures of the lacrimal canaliculi with polyethylene tubes. Arch Ophthalmol. 1950;44(2):198–203. doi:10.1001/archopht.1950.00910020203002.
- Trotter WL, Meyer DR. Endoscopic conjunctivodacryocystorhinostomy with jones tube placement. Ophthalmology. 2000;107(6):1206–1209. doi:10.1016/S0161-6420(00)00119-6.
- Devoto MH, Bernardini FP, de Conciliis C. Minimally invasive conjunctivodacryocystorhinostomy with jones tube. Ophthalmic Plast Reconstruct Surg. 2006;22(4):253–255. doi:10.1097/01.iop.0000226861.02781.af.
- Gladstone GJ, Putterman AM. A modified glass tube for conjunctivodacryocystorhinostomy. Arch Ophthalmol. 1985;103(8):1229–1230. doi:10.1001/archopht.1985.01050080141036.
- Hardman-Lea S, Yung MW. Ipswich lacrimal tube: pedicle nasal septal tube for the reconstruction of lacrimal drainage passage. J Laryngology Otol. 2003;117(2):130–131. doi:10.1258/002221503762624585.
- Can I, Can B, Yarangümeli A, et al. CDCR with buccal mucosal graft: Comparative and histopathological study. Ophthalmic Surg Lasers Imaging Retina. 1999;30(2):98–99. doi:10.3928/1542-8877-19990201-05.
- Jamshidian-Tehrani M, Kashkouli MB, Ghahvehchian H, Amini M. Lacrimal canalicular bypass surgery with autologous superficial temporal artery graft. J Curr Ophthalmol. 2022;34(4):486–488. doi:10.4103/joco.joco_98_22.
- Erickson BP, Kossler A, Blessing N, et al. The superficial temporal artery as ‘biologic jones tube’: A cadaveric proof of concept. Invest Ophthalmol Vis Sci. 2020;61(7):401–.
- Benlier E, Bozkurt M, Kulahci Y. An alternative procedure for conjunctivodacryocystorhinostomy: Supratrochlear artery-based island flap combined with buccal mucosal graft. Ann Plast Surg. 2008;60(1):55–57. doi:10.1097/SAP.0b013e31804efca6.
- Bozkurt M, Kulahci Y, Kapi E, Karakol P. A new design for superficial temporal fascial flap for reconstruction of the eyebrow, upper and lower eyelids, and lacrimal system in one-stage procedure: medusa flap. Ann Plast Surg. 2009;63(6):636–639. doi:10.1097/SAP.0b013e3181999e1b.
- Fiorino MG, Quaranta-Leoni C, Quaranta-Leoni FM. Proximal lacrimal obstructions: a review. Acta Ophthalmol. 2021;99(7):701–711. doi:10.1111/aos.14762.
- Schwarcz RM, Lee S, Goldberg RA, Simon GJ. Modified conjunctivodacryocystorhinostomy for upper lacrimal system obstruction. Arch Facial Plast Surg. 2007;9(2):96–100. doi:10.1001/archfaci.9.2.96.
- Ushio M, Masahara H, Sakamoto M, et al. Conjunctivoductivo-dacryocystorhinostomy: A novel surgery for intractable canalicular obstruction. Laryngoscope. 2022;132(4):728–731. doi:10.1002/lary.29861.
- Bagdonaite L, Pearson AR. Twelve-year experience of Lester Jones tubes—results and comparison of 3 different tube types. Ophthalmic Plast Reconstruct Surg. 2015;31(5):352–356. doi:10.1097/IOP.0000000000000340.
- Filatov V, Chevaljev V. Surgical treatment of parenchymatous ophthalmoxerosis. J Ophthalmol (Odessa). 1951;3:131–137.
- BENNETT JE, ARMSTRONG JR, JONES RE, SCHILLER F. Conjunctivoantrorhinostomy: a gravity drainage operation utilizing the maxillary sinus, with report of two cases. AMA Arch Ophthalmol. 1959;62(2):248–254. doi:10.1001/archopht.1959.04220020074011.
- Zapala J, Bartkowski AM, Bartkowski SB. Lacrimal drainage system obstruction: management and results obtained in 70 patients. J Craniomaxillofac Surg. 1992;20(4):178–183. doi:10.1016/S1010-5182(05)80393-2.

