?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Left ventricular assist device (LVAD) has been highlighted as a new treatment option in the end-stage heart failure (HF). Kidney outcome after LVAD in severe cardiorenal syndrome (CRS) patients requiring kidney replacement therapy (KRT) is unclear. We investigated the impact of preoperative KRT on kidney function and survival in LVAD patients with severe CRS. A total of 50 patients followed up for at least 1 year after LVAD implantation was analyzed. The primary outcomes were estimated glomerular filtration rate and survival rate. Patients were divided into two groups depending on in-hospital KRT before LVAD implantation: the control group (n = 33) and the KRT group (n = 17). Postoperative KRT was performed for 76.5% of patients in the KRT group, and all of them discontinued KRT before discharge. There were no statistically significant differences in the degree of eGFR decline in survivors according to preoperative KRT. Although there were no statistically significant differences in the degree of eGFR decline in survivors regardless of preoperative KRT, old age (β −0.94, p < 0.01), preexisting chronic kidney disease (β −21.89, p < 0.01), and high serum creatinine (β −13.95, p < 0.01) were identified as independent predictors of post-LVAD eGFR decline. Mortality rate was higher, and more patients progressed to end-stage kidney disease in KRT group than control group. However, LVAD still can be considered as the treatment option in end-stage HF patients with severe CRS requiring KRT, especially in those with young age and previous normal kidney function.
Introduction
The prevalence of heart failure (HF) is dramatically increasing with the aging of population [Citation1]. The nationwide prevalence of HF in Korea in 2002 was 0.75% and 1.53% in 2012 and is expected to increase to 3.35% in 2040, with more than 1.7 million Koreans expected to suffer from HF [Citation2]. Heart transplantation (HT) is the definitive treatment for end-stage HF, and the annual number of HTs has increased worldwide over the last decade [Citation3]. However, the shortage of organs for transplantation is a big obstacle. In North America, 40,253 patients were waiting for HT from 1987 to 2012, with a median survival of 2.3 years [Citation4]. Left ventricular assist device (LVAD) has become a new treatment option as a bridge to HT or a definite treatment, especially for patients with refractory HF who are difficult to receive or wait for HT. LVAD improves survival and quality of life in HF patients, with an overall survival rate of 67.7% at 2 years after isolated continuous flow LVAD implantation [Citation5].
Cardiorenal syndrome (CRS) is defined as a spectrum of disorders involving both heart and kidneys in which acute or chronic dysfunction in one organ induces acute or chronic dysfunction in the other organ [Citation6]. Therefore, kidney dysfunction is very common in patients with HF. More than half of patients with HF usually have some degree of kidney impairment, and approximately 30% of HF patients have moderate to severe kidney impairment [Citation7]. Kidney dysfunction may be associated with poor survival in HF patients including the patients undergoing HT [Citation8]. On the other hand, the incidence of cardiovascular events has been shown to be significantly higher in patients with advanced CKD [Citation9]. In considering the importance of heart–kidney crosstalk defined as CRS, combined heart–kidney transplantation was recommended for irreversible severe kidney dysfunction (GFR < 30 mL/min/1.73 m2) [Citation10].
Kidney function was reported to improve after LVAD implantation by increasing kidney perfusion through circulatory improvement [Citation11,Citation12]. However, several studies reported that kidney dysfunction before or after LVAD is associated with poor survival [Citation13,Citation14]. Furthermore, patients with end-stage kidney disease (ESKD) showed extremely poor prognosis after LVAD, so ESKD is considered a contraindication for LVAD [Citation15,Citation16]. In this study, we investigated post-LVAD kidney outcome in severe HF patients receiving LVAD implantation. The clinical impacts of preoperative kidney replacement therapy (KRT) before LVAD implantation were comprehensively analyzed focusing on changes in eGFR and survival after surgery.
Materials and method
Study population and variables
This single-center, retrospective cohort study included all patients who received continuous flow LVAD (HeartMate II LVAS or HeartWare HVAD) at Samsung Medical Center, Sungkyunkwan University School of Medicine from 2012 to 2019. All patients were classified into two groups depending on preoperative KRT. Preoperative KRT was defined as hemodialysis (HD) or continuous renal replacement therapy (CRRT) started before LVAD implantation. Patients receiving KRT only after surgery were classified as the postoperative KRT group in the subgroup analysis.
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Samsung Medical Center (IRB number: SMC 2021-07-051-001). Written informed consent from the participants was waived by the IRB.
Risk factors for CRS including preexisting diabetes mellitus (DM), hypertension (HTN), underlying chronic kidney disease (CKD), and atrial fibrillation (AF) were analyzed with baseline kidney function. CKD was defined as eGFR < 60 mL/min/1.73 m2 at least for 3 months before admission. Laboratory results including hemoglobin (Hb), BUN, serum uric acid, urine albumin/creatinine ratio (UACR), and N-terminal pro-brain natriuretic peptide (NT-proBNP) were analyzed. Echocardiographic findings for ventricular dysfunction including left ventricle ejection fraction (LVEF), early and late mitral inflow velocity, mitral annular early diastolic velocity (e′), left atrium volume index (LAVI), tricuspid annular plane systolic excursion (TAPSE), tricuspid lateral annular systolic velocity (S′), and maximum pressure gradient of tricuspid regurgitation (TR Vmax) were analyzed. Medications associated with heart and kidney function, including β-blocker (BB), renin–angiotensin system (RAS) blocker such as angiotensin receptor blocker (ARB) and angiotensin converting enzyme inhibitor (ACEi), sacubitril-valsartan, and aldosterone antagonist, were also analyzed.
Outcomes
The primary outcome was the changes in eGFR after LVAD according to preoperative KRT. Kidney function was evaluated by estimated glomerular filtration rate (eGFR) calculated with the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [Citation17]. When dialysis was required after discharge, eGFR was assumed to be 5 mL/min/1.73 m2 for convenience of analysis.
Statistical analysis
Continuous variables are presented as mean ± SD in normally distributed data or as median (interquartile range) in non-normally distributed data. Categorical variables were presented as counts (percentage). Continuous variables were compared using the independent two-sample t test or Mann–Whitney U test, and categorical variables were compared using the Chi-square test. Differences in serial eGFR after LVAD implantation between the two groups and risk factors of kidney function impairment were assessed by a linear fixed effects model. Repeated eGFR measurements were modeled using a linear fixed effects model with preoperative KRT. Time was treated as a categorical variable (at admission, postoperative 1 year, postoperative 2 years, and postoperative 3 years). We applied log function to NT-proBNP due to skewed distribution. Multivariable analysis included significant variables with p < 0.05 in univariable analysis and no interaction with time. Preoperative KRT and LVEF were include as exception. Analysis of variance (ANOVA) with Bonferroni correction and the linear fixed effects model were used for subgroup analysis. Survival probability was analyzed by Kaplan–Meier survival analysis. Statistical analysis was performed with IBM SPSS statistics 25.0 for Windows (IBM Corp., Armonk, NY, USA). A two-sided p 0.05 was considered statistically significant.
Results
Patient characteristics
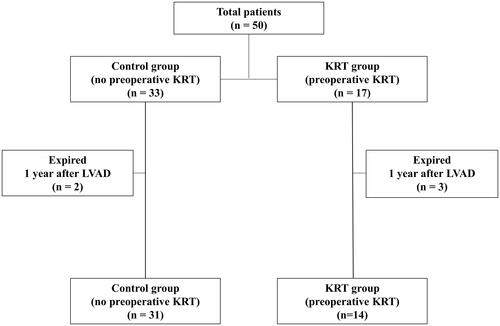
This study included 50 Korean patients who received continuous flow LVAD. No patients with preexisting ESKD were included in our study. Flowchart of enrolled patients was presented as . The median age was 65 years and 76% of the enrolled patients were male. Patients were divided into two groups depending on preoperative KRT: the control (non-KRT) group (n = 33) and KRT group (n = 17). The main indications of preoperative KRT were oliguria and uncontrolled volume overload before LVAD implantation.
Figure 1. Flowchart of enrolled patients. A total of 50 patients were included in our study. Patients were divided into two groups depending on preoperative KRT: the control (non-KRT) group (n = 33) and the KRT group (n = 17). Analysis for baseline characteristics and survival was performed. Linear fixed effects analysis regarding post-LVAD eGFR was performed after excluding patients who expired before 1 year after LVAD implantation (n = 2 in the control group and n = 3 in the KRT group).
Baseline characteristics including primary heart disease and type of LVAD are shown in . Average body mass index (BMI) was approximately 23 kg/m2 at admission in both groups. Age, sex, and comorbidities such as HTN, DM, AF, and CKD were comparable between the two groups. However, serum creatinine (Cr) at admission was higher in KRT group [control 1.35 (1.10, 1.79) vs. KRT 2.18 (1.43, 3.23) mg/dL, p = 0.041] and the eGFR at admission tended to be higher in the control group [control 46 (37.0, 64.4) vs. KRT 34.4 (17.5, 53.0) mL/min/1.73 m2, p = 0.061]. Anemia was more severe in the KRT group (hemoglobin, control 12.66 ± 1.84 vs. KRT 10.89 ± 2.43 g/dL, p = 0.01). LVEF was comparable in the two groups (control 22.15 ± 5.77 vs. KRT 25.16 ± 6.09 %, p = 0.10), but NT-proBNP was higher in the KRT group [control 7922 (4681, 12,756) vs. KRT 16,470 (6923, 25,427) pg/mL, p = 0.06].
Table 1. Baseline characteristics.
The use of RAS blockers including ARB and ACEi, sacubitril/valsartan, β-blocker, and aldosterone antagonist was comparable in the two groups. Two types of LVAD devices, HeartMate II LVAS (Abbott, Chicago, IL, USA) and HeartWare HVAD (Medtronic, Dublin, Ireland), were used in the study population. The strategies of LVAD implantation were classified by goal: bridge to HT or destination therapy. There were no significant differences between the type of machine and strategy of device at the time of LVAD implantation. Dilated cardiomyopathy (DCMP) was the most common diagnosis, followed by ischemic cardiomyopathy (ICMP). The Interagency Registry for Mechanically assisted Circulatory Support (INTEMACS) patient profile classified 60% of total patients as profile 3 (stable but inotrope dependent) and 30% of total patients as profile 2 (progressive decline). Postoperative KRT was applied in 76.5% of the patients receiving preoperative KRT [9 (27.3%) in the control group vs. 13 (76.5%) in the KRT group, p < 0.01].
Kidney function changes after LVAD implantation
In 47 patients (94%), postoperative kidney function significantly improved after LVAD implantation (eGFR at admission 46.6 ± 24.6 vs. eGFR at discharge 78.8 ± 33.2 mL/min/1.73 m2, p < 0.01). However, eGFR gradually decreased during the follow-up period after discharge (eGFR: post-LVAD 1 year, 61.9 ± 28.3 mL/min/1.73 m2; 2 years, 58.5 ± 30.1; 3 years, 59.9 ± 32.9 mL/min/1.73 m2).
Difference in kidney function after LVAD implantation according to preoperative KRT
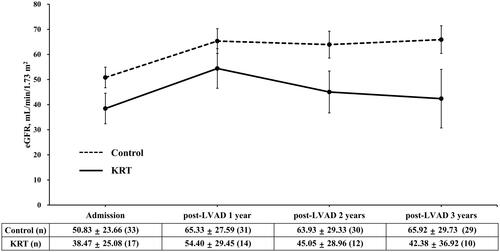
Serial changes in eGFR until 3 years after LVAD implantation were analyzed (). At each examined time point, the eGFR of the KRT group was lower than that of the control group (eGFR at admission, control 51.53 ± 24.25 vs. KRT 37.16 ± 27.39 mL/min/1.73 m2, p = 0.11; post-LVAD 1 year, control 65.33 ± 27.59 vs. KRT 54.40 ± 29.45 mL/min/1.73 m2, p = 0.25; 2 years, control 63.93 ± 29.33 vs. KRT 45.05 ± 28.96 mL/min/1.73 m2, p = 0.071; 3 years, control 65.92 ± 29.73 vs. KRT 42.38 ± 36.92 mL/min/1.73 m2, p = 0.091). However, there was no statistically significant difference in the overall slope of eGFR decline in survivors between the groups (p = 0.57).
Figure 2. Changes in eGFR depending on preoperative KRT. In all patients, eGFR was significantly improved after LVAD implantation. At each time point up to 3 years after LVAD implantation, eGFR of the KRT group was lower than that of the control group. However, there was no statistical difference in the degree of eGFR decline over postoperative time between the two groups (p = 0.57). *p < 0.05 compared with the control group at each time point. The eGFR are presented as mean ± SD at the time point.
The factors affecting post-LVAD eGFR changes are summarized in . The eGFR of expired patients was excluded at each time point in the analysis. Preoperative KRT was not associated with post-LVAD eGFR changes in univariable and multivariable analyses. Although preoperative KRT and LVEF was not associated with lower eGFR after LVAD in univariable analysis, these were included in multivariable analysis to confirm the effect to the changes of eGFR. Considering interaction between CKD, BUN, and serum Cr, these were divided in multivariable model separately. Model 1 included CKD, model 2 included BUN, and model 3 included serum Cr. Multivariable analysis identified old age as a risk factor for lower eGFR after LVAD implantation. CKD, BUN, and serum Cr also showed statistical significance in included model each. Though HTN was associated with lower eGFR in univariable analysis, we excluded it in multivariable analysis because of interaction with time. High log10(NT-proBNP) was a risk factor of model 1 and E/e’ was a risk factor of model 2. The device strategy for bridge to HT was associated with lower eGFR in univariable analysis but not in multivariable analysis.
Table 2. Patient outcomes.
Table 3. Changes in eGFR after LVAD implantation according to preoperative KRT and other variables.
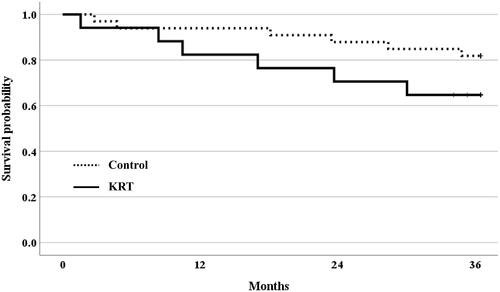
After discharge, four patients in the KRT group and one patient in the non-KRT group progressed to ESKD (). There was significant difference in the development of ESKD between the two groups (log rank p = 0.008) (). Maintenance HD was initiated for five ESKD patients at 14, 15, 18, 33, and 36 months after LVAD implantation. No ESKD patient was on peritoneal dialysis after LVAD implantation.
Survival after LVAD implantation
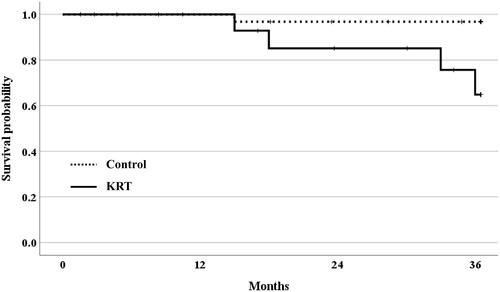
None of the patients died during hospitalization after LVAD. Two patients in the control group and three patients in the KRT group died after 1 year of LVAD implantation. Six patients in each group died after 3 years of LVAD implantation (). Kaplan–Meier survival analysis up to 3 years after surgery was performed (). Although the absolute number of deaths was higher in the KRT group than in the control group, no statistically significant difference was observed in the cumulative survival between groups (log rank p = 0.16). Additionally, three patients who developed ESKD died after 37 (KRT group), 40 (KRT group), 52 months (control group) of LVAD implantation each.
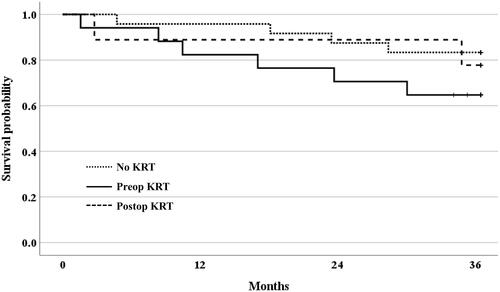
Subgroup analysis: preoperative KRT and postoperative KRT groups
In the subgroup analysis according to the initiation timing of KRT, patients in control group were divided into the no KRT group (n = 13) and postop KRT group (n = 9). The eGFR of the postop KRT group was lower than that of the no KRT group ().
Table 4. Subgroup analysis according to the initiation timing of KRT.
Kaplan–Meier survival analysis showed no significant difference in cumulative survival among subgroups (p = 0.35) ().
Discussion
In this study, we demonstrated that LVAD implantation can significantly improve kidney function even in HF patients with severe CRS requiring preoperative KRT. Furthermore, all patients requiring KRT were able to wean from KRT at discharge. Although the eGFR was still lower and more patient progressed to ESKD in the KRT than that of the control group after LVAD implantation, the decline of kidney function up to 3 years after LVAD was comparable in the two groups in survivors regardless of preoperative KRT. Age, preexisting CKD, and parameters related to heart function were independent predictors of post-LVAD eGFR decline. The overall mortality rate was 24% and mortality rate 3 years after LVAD was higher in the KRT group than the control group, although there was no statistically significant difference.
Like previous studies, our study showed that AKI caused by CRS in end-stage HF patients can be improved by LVAD implantation [Citation13,Citation14]. LVAD operation significantly improved kidney function in most patients regardless of preoperative KRT. Although patients requiring KRT before LVAD had a lower eGFR than those not requiring KRT and five patients in the KRT group progressed to ESKD after discharge, the degree of eGFR decline after discharge was comparable regardless of KRT. As increased renal venous congestion and high intratubular pressure decrease kidney perfusion and impair kidney function in patients with CRS, LVAD is expected to improve kidney function by reducing renal venous congestion and increasing cardiac output and renal arterial blood flow [Citation6]. REMATCH trial showed that LVAD improved both kidney function and quality of life and reduced mortality by 48% compared with medical therapy in patients with advanced HF [Citation18]. Butler et al. reported that, in patients with pre-LVAD creatinine clearance < 50 mL/min, the recovery of kidney function to creatinine clearance > 50 mL/min was associated with a trend toward better 30-day survival compared with those who remained at creatinine clearance < 50 mL/min after LVAD implantation [Citation19].
Although statistically insignificant, mortality rate after LVAD tended to be higher in the KRT group compared to the control group (control 13.2 vs. KRT 35.3% at 3 years after LVAD). However, the 3-year survival rate in the preoperative KRT group in our study was approximately 64.7%, which was higher than the previously reported survival rates. Previous studies reported a poor survival rate after LVAD implantation in patients with AKI requiring perioperative KRT. Only one-third of patients requiring KRT after LVAD were discharged after discontinuation of KRT, one-third were discharged with KRT-dependent status and the remaining one-third died during hospitalization [Citation13]. Additionally, a recent study by Silver et al. reported an in-hospital mortality of 47.4% in LVAD patients with AKI requiring dialysis [Citation20]. Other studies also showed a worse prognosis after LVAD in patients with kidney dysfunction compared with our study [Citation20–22]. Post-LVAD AKI requiring KRT showed 5.4-fold increased risk of 1-year mortality in a recent meta-analysis [Citation23].
Interestingly, all patients in the KRT group were able to discontinue KRT before discharge and no in-hospital mortality was reported in our study. Patients who require post-LVAD KRT remained at high risk for adverse outcomes even if their kidney function recovered enough to no longer require KRT [Citation13]. The patient selection criteria for LVAD and the strategy of applying KRT before and after LVAD implantation in our study might be different from those of other studies.
A postoperative kidney function decline between discharge and 3 years after LVAD implantation was shown in our study. Post-LVAD AKI was a common complication and a decline of eGFR was observed after LVAD implantation in several studies [Citation14,Citation18,Citation19,Citation23,Citation24]. The cause of the gradual decrease in kidney function after initial improvement after LVAD is still unclear. The gradual worsening of native cardiac function including right ventricular failure, pigment nephropathy due to chronic hemolysis, or adverse effect of continuous flow by LVAD were suggested as underlying mechanisms of kidney function deterioration after LVAD [Citation14,Citation25,Citation26]. An animal study showed that the continuous flow of LVAD can induce severe periarteritis and the upregulation of the intrarenal renin–angiotensin–aldosterone system [Citation27]. However, this late decrease in eGFR was similarly observed in patients with pulsating and continuous flow LVAD [Citation15,Citation28]. Additionally, decreased creatinine production due to sarcopenia in severe HF patients can overestimate baseline serum creatinine–based eGFR including the CKD-EPI equation. An improvement in the overall conditions and increased muscle mass after LVAD implantation can potentially induce some degree of decrease in serum creatinine-based eGFR. Further research is needed to identify the cause of the gradual decrease in kidney function after LVAD.
Older age and preexisting CKD were associated with eGFR decrement after LVAD implantation. Recently, Papathanasiou et al. reported that BNP was not associated with higher risk of mortality and hospitalization [Citation29]. Because NT-proBNP had negative predictive value in univariable analysis in our study, further study for the serial changes of NT-proBNP in larger group may be needed. In accordance with a previous study showing similar outcomes including post-HT dialysis, mortality, and hospital length of stay between Heartware HVAD and Heartmate II LVAD [Citation30], the type of LVAD machine did not affect postoperative kidney function in our study. Although the device strategy of bridge to HT was associated with higher eGFR after surgery in univariable analysis, it was not selected as variable for multivariable analysis.
This study has several limitations. First, potential hidden confounders might have intervened because of the retrospective study design. Though proteinuria has been known for a risk factor of KRT after LVAD [Citation31], UACR data were not available enough to analysis in our study. Because UACR measurement was not part of the diagnostic protocol for HF patients in the cardiology division. Nevertheless, we tried to include factors that potentially affect kidney function as much as possible. Second, the sample size was relatively small to sufficiently elucidate the effects of relevant factors in the multivariable analysis. Although there were no significant differences in the degree of eGFR decline and mortality between the two groups, the possibility of preoperative KRT as a risk factor for mortality cannot be excluded. Third, our results might be difficult to generalize, as it was a single-center study. However, we believe that our study is meaningful since reports regarding Asian HF patients with LVAD or HT are disproportionately sparse. HT reports from North America, where only 7.5% of the world population live, accounted for 55.8% of HTs in the 2012 International Society for Heart and Lung Transplantation registry, whereas reports from Asia, where 62.5% of the world population live, accounted for only 5.7% of all HTs [Citation32]. Therefore, our study analyzing kidney outcome in Korean HF patients after LVAD implantation has clinical value as it adds data for the Asian ethnicity and the clinical importance of CRS. Fourth, the 3-year follow-up period might be insufficient to evaluate the survival rate. However, even a higher mortality rate and decreased kidney function were reported within approximately 1–2 years after LVAD implantation in previous studies [Citation13,Citation14].
Conclusion
In our study, more patients progressed to ESKD, and mortality rate might be higher in the preoperative KRT group. However, mortality rate in the preoperative KRT group was much lower compared to previous studies. In addition, all patients requiring preoperative KRT were able to wean from KRT before discharge and the degree of eGFR decline over time was comparable regardless of preoperative KRT. Therefore, LVAD still may be considered as a treatment option in end stage HF patients with severe CRS requiring KRT, especially in younger patients and patients with no previous CKD.
Author contributions
H.J., J.J., and H.R.J. designed the study. H.J., J.J., and D.K. analyzed the data. H.J., J.J., D.K., Y.H.C., J.E.L., J.C., W.H., Y.K., E.J., and H.R.J. interpreted the data. H.J. and H.R.J. wrote the manuscript. K.L., J.J., and H.R.J. revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Acknowledgments
The authors would like to thank the KRT nursing team and transplantation team of Samsung Medical Center for their dedicated effort.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606–619.
- Park JJ, Choi DJ. Current status of heart failure: global and Korea. Korean J Intern Med. 2020;35(3):487–497.
- Lund LH, Khush KK, Cherikh WS, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-fourth Adult Heart Transplantation Report-2017; focus theme: allograft ischemic time. J Heart Lung Transplant. 2017;36(10):1037–1046.
- Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528.
- Rogers JG, Pagani FD, Tatooles AJ, et al. Intrapericardial left ventricular assist device for advanced heart failure. N Engl J Med. 2017;376(5):451–460.
- Rangaswami J, Bhalla V, Blair JEA, et al. Cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2019;139(16):e840–e878.
- Smith GL, Lichtman JH, Bracken MB, et al. Renal impairment and outcomes in heart failure: systematic review and meta-analysis. J Am Coll Cardiol. 2006;47(10):1987–1996.
- Dunlay SM, Weston SA, Jacobsen SJ, et al. Risk factors for heart failure: a population-based case-control study. Am J Med. 2009;122(11):1023–1028.
- Jankowski J, Floege J, Fliser D, et al. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation. 2021;143(11):1157–1172.
- Mehra MR, Canter CE, Hannan MM, et al. The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: a 10-year update. J Heart Lung Transplant. 2016;35(1):1–23.
- Singh M, Shullo M, Kormos RL, et al. Impact of renal function before mechanical circulatory support on posttransplant renal outcomes. Ann Thorac Surg. 2011;91(5):1348–1354.
- Kirklin JK, Naftel DC, Kormos RL, et al. Quantifying the effect of cardiorenal syndrome on mortality after left ventricular assist device implant. J Heart Lung Transplant. 2013;32(12):1205–1213.
- Asleh R, Schettle S, Briasoulis A, et al. Predictors and outcomes of renal replacement therapy after left ventricular assist device implantation. Mayo Clin Proc. 2019;94(6):1003–1014.
- Ajmal MS, Parikh UM, Lamba H, et al. Chronic kidney disease and acute kidney injury outcomes post left ventricular assist device implant. Cureus. 2020;12(4):e7725.
- Brisco MA, Kimmel SE, Coca SG, et al. Prevalence and prognostic importance of changes in renal function after mechanical circulatory support. Circ Heart Fail. 2014;7(1):68–75.
- Bansal N, Hailpern SM, Katz R, et al. Outcomes associated with left ventricular assist devices among recipients with and without end-stage renal disease. JAMA Intern Med. 2018;178(2):204–209.
- Levey AS, Stevens LA, Schmid CH, et al. New equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612.
- Rose EA, Gelijns AC, Moskowitz AJ, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001;345(20):1435–1443.
- Butler J, Geisberg C, Howser R, et al. Relationship between renal function and left ventricular assist device use. Ann Thorac Surg. 2006;81(5):1745–1751.
- Silver SA, Long J, Zheng Y, et al. Outcomes after left ventricular assist device implantation in patients with acute kidney injury. J Thorac Cardiovasc Surg. 2020;159(2):477–486.e3.
- Sandner SE, Zimpfer D, Zrunek P, et al. Renal function and outcome after continuous flow left ventricular assist device implantation. Ann Thorac Surg. 2009;87(4):1072–1078.
- Kirklin JK, Naftel DC, Pagani FD, et al. Sixth INTERMACS annual report: a 10,000-patient database. J Heart Lung Transplant. 2014;33(6):555–564.
- Thongprayoon C, Lertjitbanjong P, Cheungpasitporn W, et al. Incidence and impact of acute kidney injury on patients with implantable left ventricular assist devices: a meta-analysis. Ren Fail. 2020;42(1):495–512.
- Kormos RL, Cowger J, Pagani FD, et al. The Society of Thoracic Surgeons Intermacs database annual report: evolving indications, outcomes, and scientific partnerships. J Heart Lung Transplant. 2019;38(2):114–126.
- Miyamoto T, Karimov JH, Fukamachi K. Effects of continuous and pulsatile flows generated by ventricular assist devices on renal function and pathology. Expert Rev Med Devices. 2018;15(3):171–182.
- Muslem R, Caliskan K, Akin S, et al. Pre-operative proteinuria in left ventricular assist devices and clinical outcome. J Heart Lung Transplant. 2018;37(1):124–130.
- Ootaki C, Yamashita M, Ootaki Y, et al. Reduced pulsatility induces periarteritis in kidney: role of the local renin-angiotensin system. J Thorac Cardiovasc Surg. 2008;136(1):150–158.
- Sandner SE, Zimpfer D, Zrunek P, et al. Renal function after implantation of continuous versus pulsatile flow left ventricular assist devices. J Heart Lung Transplant. 2008;27(5):469–473.
- Papathanasiou M, Pizanis N, Tsourelis L, et al. Dynamics and prognostic value of B-type natriuretic peptide in left ventricular assist device recipients. J Thorac Dis. 2019;11(1):138–144.
- Topkara VK, O'Neill JK, Carlisle A, et al. HeartWare and HeartMate II left ventricular assist devices as bridge to transplantation: a comparative analysis. Ann Thorac Surg. 2014;97(2):506–512.
- Topkara VK, Coromilas EJ, Garan AR, et al. Preoperative proteinuria and reduced glomerular filtration rate predicts renal replacement therapy in patients supported with continuous-flow left ventricular assist devices. Circ Heart Fail. 2016;9(12):e002897.
- Sivathasan C, Lim CP, Kerk KL, et al. Mechanical circulatory support and heart transplantation in the Asia Pacific region. J Heart Lung Transplant. 2017;36(1):13–18.