Abstract
Objectives
We investigated the attitudes to change the frequency of menstrual bleeding by using combined hormonal contraception (CHC). Personality characteristics were also explored.
Methods
We conducted a cross-sectional study in two university hospitals in northern Italy. Current, past and never CHC users (n = 545; age 18–44 years) completed a self-administered semi-structured questionnaire and the Ten-Item Personality Inventory (TIPI).
Results
Forty-five percent of responders (n = 301) would prefer to change their bleeding frequency by using CHC. A flexible regimen was the preferred choice (n = 80; 33%) followed by extended regimens to bleed every 3 months (n = 54; 22%) or to never bleed (n = 43; 18%). The main positive reasons were to avoid dysmenorrhea (43%) and have more freedom in sexual (36%) and active (35%) life, whereas the main reason for a negative attitude was ‘menstrual rhythm is natural’ (59%). Age had a significant influence on women’s willingness to change menstrual frequency by using CHC [>39 years (57%), 30–39 years (31%) and <30 years (46%)] (χ2: 9.1; p = 0.01). Never users significantly reported a more negative attitude (71%) in comparison with past (51%) and current users (49%) (χ2: 18.7; p = 0.001). Personality traits played a role, with higher scores of openness (p = 0.005) and extraversion (p = 0.001) in women with a positive attitude.
Conclusions
Almost half of our study sample reported a preference for changing their menstrual pattern by using CHC. Flexibility was the preferred choice across age and use of CHC. Personality characteristics (openness and extroversion) might influence attitudes toward CHC-induced menstrual bleeding changes.
Introduction
There was a growing interest on the possible use of extended combined hormonal contraception (CHC) among women and health care providers (HCPs) [Citation1]. Monthly bleeding induced by CHC did not seem to be medically necessary, especially in women with specific needs, menstruation-related conditions and/or withdrawal symptoms, and even perceived costs of hygiene products [Citation2–6]. A real-world experience of women receiving extended-cycle combined oral contraception (COC) versus monthly-cycle COC in the United States found a preferential prescription for extended-cycle COC among those reporting more health-related diagnoses and poor health [Citation7]. Sexuality, social life, work and sporting activities were also key factors affecting women’s preference for reducing the frequency of menstrual bleeding in Europe [Citation8]. About 60% of women would like less frequent menstrual bleeding [Citation8], with a frequency ranging from once every 3 months (around 1 out of 5 women) to no periods at all (around 1 out of 4 women) [Citation9].
Individual and social influences shaped attitudes toward contraceptive-induced menstrual bleeding changes, which required a thorough counseling [Citation10]. Indeed, women needed extensive information about menstrual regulation and suppression before selecting a contraceptive method, even though CHC use seemed more convenient in comparison with long-acting reversible contraceptives (LARC) [Citation11]. Multiple safe and effective tailored combined contraceptive regimens were available [Citation12] and increasingly prescribed [Citation13]. The majority of products included monophasic combined oral contraception (COC) to avoid misuse, poor cycle control and side-effects [Citation1,Citation12]. However, off-label manipulation of 28-day CHC formulations may be provided also by using combined vaginal rings/patches with superimposable effects [Citation14]. Of note, flexible regimens might give women more control and overcome the irregular bleeding profile associated with extended and continuous regimens that affected the continuation rate [Citation12,Citation15]. However, in spite the preference to bleed less frequently and even accept CHC-related amenorrhea has been established at international level [Citation10,Citation11,Citation16], there was still much debate around tailored contraceptive regimes, which were underused [Citation12,Citation15]. Deviations from the regular menstrual self could be perceived as not natural and bleeding changes well accepted only when medical needs [Citation2–6] or personal benefits [Citation17] were identified. Therefore, counseling was essential to help women to make informed choices by taking into the account their biopsychosocial profile [Citation18].
In Italy, past surveys [Citation19,Citation20] have shown a positive preference for a reduced frequency of menstrual bleeding. Only 32% of women preferred to bleed monthly and the preferred frequencies in all age groups were 3-monthly (23.7%) or never (26%) [Citation19]. Given the choice, 28.5% of women without menstruation-related symptoms would desire amenorrhea and 27.8% would prefer a reduction in the frequency of menstrual periods [Citation20]. Of note, the majority of surveyed women declared that they would accept a drug to reduce menstrual frequency [Citation20]. Surprisingly, a recent internet-based anonymous questionnaire administered to 1072 well-educated Italian women (18 - 40 years of age) showed that half of the respondents ignored the existence of methods to suppress menstruation or reduce its frequency [Citation21]. Such disconnection between wishes, knowledge and behaviors needs further data in the clinical setting.
That being so, in the present study we explored attitudes of women of reproductive age about CHC-induced menstrual bleeding changes according to their experience of use in a clinical sample based in northern Italy. In addition, we investigated the possible role of personality traits in modulating women’s preference in the use of tailored contraceptive regimens.
Materials and methods
A cross-sectional study was carried out at the Unit of Gynaecological Endocrinology, IRCCS Policlinico San Matteo Foundation, University of Pavia, and at the Department of Obstetrics and Gynecology, Sant’Anna Hospital, University of Turin, Italy, over a six-month period. A self-administered questionnaire was filled in by a sample of healthy women, aged between 18 and 44 years, during annual gynecological checkup. Potential participants had the study explained to them while in the waiting room prior to their consultation. Out of 710 women seen consecutively, 603 Italian native speakers agreed to complete the questionnaire after signing informed consent. The study was approved by the local university ethics committee.
A semi-structured interview collected data on socio-demographic characteristics, type (pill, patch, ring) and standard use (current, past, never) of CHC. In addition, attitudes toward the frequency of bleeding by using CHC, taking into account the reasons behind women’s preferences, were investigated. The questionnaire was designed by two of the authors (REN and CB) based on the available literature and on their clinical experience. Moreover, in order to explore personality traits of the study sample we used the validated ten-item personality inventory (TIPI) which measured the big-five personality domains (extraversion, agreeableness, conscientiousness, neuroticism, openness to experience) [Citation22].
Only fully completed questionnaires (n = 545) were considered suitable for statistical analysis. Data were analyzed by using frequency tables, χ2 test and other statistics, as appropriate.
Results
Characteristics of the study sample
The majority of women within the study sample was under 30 years of age (n = 426; 78%) and was born in northern Italy (n = 452; 83%), with a high rate of education (n = 508; 93% at least 13 years of schooling). More than half of our study sample were in a stable sexual relationship (n = 309; 57%) and only few (n = 61; 11%) had at least one at term birth. The sample included current (n = 202; 37%) and past (n = 205; 38%) CHC users, whereas 138 women (25%) were never users. CHC was prescribed only for contraceptive needs at present or in the past in 60% of the cases (n = 246), whereas for beneficial effects on menstrual disturbances and/or hyperandrogenic signs in 161 women (40%).
CHC was used orally by 82.2% (n°=166), whereas vaginally and transdermally by 14.8% (n°=30) and 3% (n°=6), respectively.
General attitudes toward CHC-induced menstrual bleeding changes
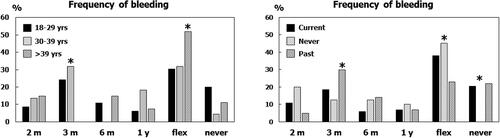
The percentage of women that would like to change the menstrual bleeding frequency by using CHC was 45% (n = 244) and of those who would not was 55% (n = 301) (, top panel). Among those women who selected the option of using CHC in order to modify their bleeding pattern (, bottom panel), a flexible regimen was the first choice (n = 80; 33%) followed by extended regimens designed to bleed every 3 months (n = 54; 22%) and to never bleed (n = 43; 18%). showed the main reasons behind the preference of women to change or not to change the pattern of their menstrual bleeding. Dysmenorrhea was on top of the list (n = 105; 43%) in women who indicated to prefer modifying their bleeding frequency, whereas the item ‘menstrual rhythm is natural’ was on top of the list in the group who did not (n = 177; 59%).
Figure 1. Attitudes toward changing the menstrual bleeding frequency by using CHC (top) and type of menstrual bleeding frequency (bottom).
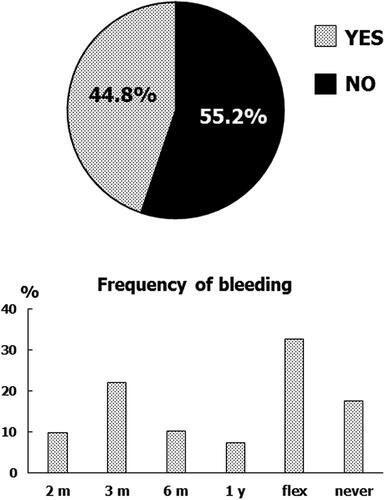
Table 1. Reasons why women would like to change or not to change the pattern of menstrual bleeding by using CHC (multiple choices were allowed).
The majority of responders (n = 397; 73%) believed it was important to predict the withdrawal bleeding date when using CHC, without any difference according to the experience of contraceptive use. Indeed, only 16% would not bother at all about the expected date of bleeding, whereas 11% of the study sample declared that spotting/breakthrough bleeding was irrelevant. Forty percent (n = 162) of current and past CHC users declared they have postponed withdrawal bleeding at least once by using additional pills/patches/rings.
Influence of women’s age and CHC use on attitudes toward CHC-induced menstrual bleeding changes
Women older than 39 years (n = 47; 9%) were significantly more likely to prefer to change their bleeding pattern (57%), whereas women in the age range between 30 and 39 years (n = 72; 13%) did less (31%) in comparison to women younger than 30 years (46%) (n = 426; 78%) (χ2: 9.1; p = 0.01). On the other hand, never-users reported a negative attitude to change their bleeding pattern (71%) more frequently than did past (51%) and current users (49%) (χ2: 18.7; p = 0.001). Interestingly enough, age seemed to be an important determinant of women’s attitudes according to the experience of contraceptive use. Indeed, only never users younger than 30 years considered the possibility to change the frequency of menstrual bleeding by using CHC (34%) in comparison to other age groups (30–39 years and >39 years; 0% for both). On the other hand, current and past CHC users displayed a similar positive attitude to change their bleeding pattern both in the older (>39 years: 69% and 76%, respectively) and in the younger group (<30 years: 49% and 51%, respectively).
showed women’s multiple choices about the menstrual bleeding frequency according to age range (left) and use of CHC (right). Women younger than 30 years of age preferred ‘to bleed in a flexible way’ (30%) followed by ‘to bleed every 3 months’ (24%). Women older than 39 years preferred ‘to bleed in a flexible way’ (52%), whereas women between 30–39 years of age ‘to bleed every 3 months’ and ‘to bleed in a flexible way’ (32% for both) (χ2: 22.0; p = 0.01). Interestingly, never users were completely not open ‘to never bleed’ (0%), whereas their preferred frequency was ‘to bleed in a flexible way’ (45%), which was also the preferred option by current users (38%); past users preferred ‘to bleed every 3 months’ in 30% of the cases (χ2: 29.7; p = 0.001).
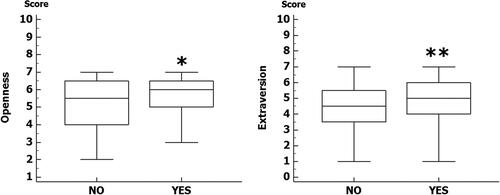
Influence of personality traits on attitudes toward CHC-induced menstrual bleeding changes
The analysis of the median scores of the big five dimensions of personality demonstrated that extraversion was significantly lower in never users of CHC in comparison with current and past users (p = 0.001). Current users displayed less variable scores for conscientiousness in comparison to never users (p = 0.003), whereas more variable scores were evident for past users (p = 0.02). In addition, past users had significantly higher score for agreeableness in comparison to current (p = 0.02) and never users (p = 0.004) (). Scores of emotional stability and openness were not different according to CHC use.
No significant personality differences were evident according to the age range. Interestingly enough, attitudes toward contraceptive-induced menstrual bleeding changes were more present in women with higher scores of openness (p = 0.005) and extraversion (p = 0.001) ().
Discussion
We observed that, in a sample of mostly young and highly educated healthy women residing in northern Italy, almost half of responders would like to modify the frequency of their bleeding pattern by using CHC. Interestingly, women in the typical reproductive age (30–39 years) and those who have never used CHC were less likely to report such preference. However, younger (<30 years) never users were more likely to consider the possibility to change the frequency of menstrual bleeding. ‘To bleed in a flexible way’ was the preferred choice across age and use of CHC. Menstrual pain was the major cause for wishing to reduce the frequency of bleeding, whereas the construct of menstruation as a natural event was the major reason for not wishing to modify menstrual pattern. Finally, extraversion was the personality trait associated with the experience of using CHC and most importantly, along with openness, to the positive attitude toward CHC-induced menstrual bleeding changes.
Our findings were in line with previous surveys in Italy [Citation19,Citation20] and other European countries [Citation8,Citation9], even though some cross-cultural differences emerged. For instance, in an early study of Dutch women’s preferences, about 70% of responders would prefer to modify their menstrual cycle frequency [Citation23], and approximately two-thirds of reproductive-aged women surveyed in Germany would prefer to bleed less frequently than monthly or never to bleed [Citation24]. Swiss women reported attitudes more similar to our data, supporting that the predictability of bleeding seemed more important than the possibility to postpone it [Citation25]. Indeed, women wished to control their bleeding, mainly because of its negative impact on their daily life, and 50% of women in Europe, North America and Latin America preferred flexibility to determine when menstrual bleeding starts [Citation26]. In a recent epidemiological, cross-sectional, multicenter study to determine women’s acceptance of a flexible continuous CHC regimen versus a cyclical regimen (FLEXO study), after receiving standardized information during contraceptive counseling in Spain, the main reasons for flexibility were relieving or eliminating discomfort related to menstruation by reducing the number of menstrual episodes [Citation27].
Experiences to alter scheduled bleeding pattern by deviating from package instruction were reported in 40% of current and past CHC users in our study, indirectly confirming that women who have received contraceptive counseling were reassured regarding the safety of this approach [Citation14,Citation16]. However, the evidence that in our sample of younger women who did not have any experience of CHC use 34% considered the possibility to change the frequency of menstrual bleeding by using a CHC further corroborated the crucial role of counseling to empower any woman in her contraceptive choice [Citation28]. Adequate training of HCPs to discuss tailored combined contraceptive regimens seems necessary because even some family planning specialists in the UK admitted feeling more comfortable when prescribing standard contraceptive regimens [Citation29].
An interesting qualitative UK study showed that in young women the idea of selecting contraceptive hormones that might stop the bleeding was more popular in presence of painful natural menstruation [Citation30]. Moreover, it confirmed that cyclic bleeding still holds a symbolic function for women and, therefore, HCPs should consider the importance of perceiving ‘a natural body’ [Citation30] because it counteracts fears of infertility commonly associated with the use of CHC [Citation31] or with CHC-induced menstrual bleeding changes [Citation16,Citation32]. Only 18% of our study sample preferred ‘to never bleed’, a choice that was completely absent in never CHC users, supporting previous knowledge across the world [Citation16] and beliefs of women with different contraceptive attitudes about the importance of having monthly menstruation [Citation33].
In agreement with the literature [Citation1], main reasons to change the pattern of menstrual bleeding by using CHC were symptoms associated with menstruation. However, preferences for less frequent bleeding were not limited to negative menstrual experiences and included more freedom in sexual life (36%) and improvement in daily activities (35%) and quality of life (35%). In another Italian study, 76% of women without menstrual symptoms reported that menstrual periods interfered with their sexual life, 48% felt that menstruation interfered with their sporting activities and 29% preferred not having their period at work [Citation20]. In our study, only few women (9%) considered ‘better contraceptive efficacy’ as a reason to prefer changing the frequency of menstrual bleeding by using CHC. Even though not well proven in randomized controlled trials comparing continuous or extended-cycle versus traditional cyclic administration [Citation14], it was conceivable that extended cycle CHC might have increased efficacy compared with traditional cyclic CHC [Citation34]. When extended COC regimens were used to avoid menstruation for convenience or personal preference, they could led to improved adherence and greater user satisfaction [Citation35,Citation36]. Our sample of Italian women confirmed that reasons to prefer not changing the frequency of menstrual bleeding were ‘the menstrual rhythm is natural’ (59%) and ‘important for health’ (27%), as well as fear of adverse events (23%), getting pregnant (20%) or become infertile (8%). In a past anonymous survey, also few HCPs believed extended COCs increased the risk of thrombosis (14%), cancer (8%) and infertility (4%) if compared with standard COC regimens [Citation13]. However, no signals in the literature indicated that users of extended-regimen COCs appear to have an increased risk of breast cancer, infertility, or thrombosis beyond conventional 28-day regimens [Citation13]. For instance, a recent study comparing the use of 28-day standard COC with the use of 91-day extended COC containing levonorgestrel (LNG) did not show any significant differences in risk of venous and arterial thromboembolism [Citation37].
Among the multitude of factors influencing contraceptive choice [Citation18,Citation38], the influence of personality has been mainly studied in risky sexual behaviors [Citation39]. However, personality characteristics of women might play a role in influencing views, expectations, mood, ability to cope with side effects or unexpected events, along with social interactions and effective communication with HCPs [Citation40]. A well-powered study did not find personality differences between users and not users of CHC [Citation41], whereas another study linking personality to contraception suggested that some characteristics (agreeableness and extraversion) were more strongly associated to the choice of contraceptive type rather than the choice between hormonal and non-hormonal options [Citation40]. According to our data, influence of conscientiousness needed to be further explored in current, past and never CHC users. Interestingly, higher levels of openness and extroversion were associated with the preference of changing the frequency of menstrual bleeding by using CHC, where extraversion could be associated with contraceptive experience. Taking into account these user’s personality characteristics might be relevant in contraceptive counseling and deserved well-designed studies with tailored contraceptive regimens.
Strengths of our study included the involvement of a large sample of well-educated healthy women of childbearing age recruited at two university hospitals with similar socio-cultural backgrounds interviewed also with a validated psychometric questionnaire. In addition, our findings might be a starting point to design strategies of counseling adequate to tailored contraceptive regimens, which should take into account also personal characteristics of the individual woman in a biopsychosocial perspective [Citation18]. The study had also limitations, mainly related to the overrepresentation of nulliparous young women that prevented the possibility to generalize our findings to women during the entire reproductive life span.
In conclusion, 45% of women in our study sample reported a preference for changing their menstrual pattern by using CHC and flexibility was the preferred choice across age and use of CHC. Personality characteristics (openness and extroversion) might influence attitudes toward CHC-induced menstrual bleeding changes.
Acknowledgments
The authors are grateful to Bayer Pharma – Italy for an unrestricted University Grant in order to support this project.
Disclosure statement
Prof Rossella E. Nappi had past financial relationships (lecturer, member of advisory boards and/or consultant) with Boehringer Ingelheim, Ely Lilly, Endoceutics, Merck Sharpe & Dohme, Palatin Technologies, Pfizer Inc, Procter & Gamble Co, TEVA Women’s Health Inc and Zambon SpA. At present, she has ongoing relationship with Astellas, Bayer HealthCare AG, Exceltis, Fidia, Gedeon Richter, HRA Pharma, Novo Nordisk, Organon & Co, Shionogi Limited and Theramex, outside the submitted manuscript. Other authors reports no conflicts of interest in this manuscript.
Additional information
Funding
References
- Nappi RE, Kaunitz AM, Bitzer J. Extended regimen combined oral contraception: a review of evolving concepts and acceptance by women and clinicians. Eur J Contracept Reprod Health Care. 2016;21(2):1–6.
- Wiegratz I, Kuhl H. Long-cycle treatment with oral contraceptives. Drugs. 2004;64(21):2447–2462.
- MacGregor EA, Guillebaud J. The 7-day contraceptive hormone-free interval should be consigned to history. BMJ Sex Reprod Health. 2018;44(3):214–220.
- Hardy E, Hebling EM, de Sousa MH, et al. Association between characteristics of current menses and preference for induced amenorrhea. Contraception. 2009;80(3):266–269.
- Kirkham YA, Ornstein MP, Aggarwal A, et al. Menstrual suppression in special circumstances. J Obstet Gynaecol Can. 2014;36(10):915–924.
- Trego LL, Jordan PJ. Military women’s attitudes toward menstruation and menstrual suppression in relation to the deployed environment: development and testing of the MWATMS-9 (short form). Womens Health Issues. 2010;20(4):287–293.
- Nappi RE, Lete I, Lee LK, et al. Real-world experience of women using extended-cycle vs monthly-cycle combined oral contraception in the United States: the national health and wellness survey. BMC Womens Health. 2018;18(1):22.
- Fiala C, Chabbert-Buffet N, Häusler G, et al. Women’s preferences for menstrual bleeding frequency in 12 european countries: the inconvenience due to women’s monthly bleeding (ISY) survey. Eur J Contracept Reprod Health Care. 2017;22(4):268–273.
- Nappi RE, Fiala C, Chabbert-Buffet N, et al. Women’s preferences for menstrual bleeding frequency: results of the inconvenience due to women’s monthly bleeding (ISY) survey. Eur J Contracept Reprod Health Care. 2016;21(3):242–250.
- Polis CB, Hussain R, Berry A. There might be blood: a scoping review on women’s responses to contraceptive-induced menstrual bleeding changes. Reprod Health. 2018;15(1):114.
- DeMaria AL, Sundstrom B, Meier S, et al. The myth of menstruation: how menstrual regulation and suppression impact contraceptive choice. BMC Womens Health. 2019;19(1):125.
- Benson LS, Micks EA. Why stop now? Extended and continuous regimens of combined hormonal contraceptive methods. Obstet Gynecol Clin North Am. 2015;42(4):669–681.
- Seval DL, Buckley T, Kuehl TJ, et al. Attitudes and prescribing patterns of extended-cycle oral contraceptives. Contraception. 2011;84(1):71–75.
- Edelman A, Micks E, Gallo MF, et al. Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception. Cochrane Database Syst Rev. 2014;2014(7):CD004695.
- Percy L, Mansour D. Tailoring oral contraceptive pills to meet the needs of women. J Fam Plann Reprod Health Care. 2013;39(4):237–240.
- Glasier AF, Smith KB, van der Spuy ZM, et al. Amenorrhea associated with contraception-an international study on acceptability. Contraception. 2003;67(1):1–8.
- Lakehomer H, Kaplan PF, Wozniak DG, et al. Characteristics of scheduled bleeding manipulation with combined hormonal contraception in university students. Contraception. 2013;88(3):426–430.
- Bitzer J, Marin V, Lira J. Contraceptive counselling and care: a personalized interactive approach. Eur J Contracept Reprod Health Care. 2017;22(6):418–423.
- Fruzzetti F, Paoletti AM, Lombardo M, et al. Attitudes of italian women concerning suppression of menstruation with oral contraceptives. Eur J Contracept Reprod Health Care. 2008;13(2):153–157.
- Ferrero S, Abbamonte LH, Giordano M, et al. What is the desired menstrual frequency of women without menstruation-related symptoms? Contraception. 2006;73(5):537–541.
- Bastianelli C, Grandi G, Farris M, et al. Attitudes towards menstruation: what women want? An Italian National Survey. Eur J Contracept Reprod Health Care. 2022;1:1–8.
- Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the big-five personality domains. J Res Personality. 2003;37(6):504–528.
- den Tonkelaar I, Oddens BJ. Preferred frequency and characteristics of menstrual bleeding in relation to reproductive status, oral contraceptive use, and hormone replacement therapy use. Contraception. 1999;59(6):357–362.
- Wiegratz I, Hommel HH, Zimmermann T, et al. Attitude of german women and gynecologists towards long-cycle treatment with oral contraceptives. Contraception. 2004;69(1):37–42.
- Merki-Feld GS, Breitschmid N, Seifert B, et al. A survey on swiss women’s preferred menstrual/withdrawal bleeding pattern over different phases of reproductive life and with use of hormonal contraception. Eur J Contracept Reprod Health Care. 2014;19(4):266–275.
- Szarewski A, von Stenglin A, Rybowski S. Women’s attitudes towards monthly bleeding: results of a global population-based survey. Eur J Contracept Reprod Health Care. 2012;17(4):270–283.
- Lete I, Calleja J, Pérez-Campos E, et al. Cross-sectional evaluation of the impact of information on flexible extended regimens of oral contraceptives in the choices made by women seeking contraceptive counselling: the FLEXO study. Eur J Contracept Reprod Health Care. 2018;23(4):260–264.
- Bitzer J, Gemzell-Danielsson K, Roumen F, et al. The CHOICE study: effect of counselling on the selection of combined hormonal contraceptive methods in 11 countries. Eur J Contracept Reprod Health Care. 2012;17(1):65–78.
- Sauer U, Mann S, Brima N, et al. Offering extended use of the combined contraceptive pill: a survey of specialist family planning services. Int J Womens Health. 2013;5:613–617.
- Newton VL, Hoggart L. Hormonal contraception and regulation of menstruation: a study of young women’s attitudes towards ‘having a period. J Fam Plann Reprod Health Care. 2015;41(3):210–215.
- Nappi RE, Pellegrinelli A, Campolo F, et al. Effects of combined hormonal contraception on health and wellbeing: women’s knowledge in Northern Italy. Eur J Contracept Reprod Health Care. 2015;20(1):36–46.
- Estanislau do Amaral MC, Hardy E, Hebling EM, et al. Menstruation and amenorrhea: opinion of Brazilian women. Contraception. 2005;72(2):157–161.
- Thomas SL, Ellertson C. Nuisance or natural and healthy: should monthly menstruation be optional for women? Lancet. 2000;355(9207):922–924.
- Steinauer J, Autry AM. Extended cycle combined hormonal contraception. Obstet Gynecol Clin North Am. 2007;34(1):43–55.
- Mendoza N, Lobo P, Lertxundi R, et al. Extended regimens of combined hormonal contraception to reduce symptoms related to withdrawal bleeding and the hormone-free interval: a systematic review of randomised and observational studies. Eur J Contracept Reprod Health Care. 2014;19(5):321–339.
- Panicker S, Mann S, Shawe J, et al. Evolution of extended use of the combined oral contraceptive pill. J Fam Plann Reprod Health Care. 2014;40(2):133–141.
- Kaplan S, Bertoia ML, Wang FT, et al. Long-term safety of extended levonorgestrel-containing oral contraceptives in the United States. Contraception. 2022;105:26–32.
- Yeh PT, Kautsar H, Kennedy CE, et al. Values and preferences for contraception: a global systematic review. Contraception. 2022;111:3–21.
- Ruiz-Palomino E, Ballester-Arnal R, Gil-Llario MD. Personality as a mediating variable in condom use among spanish youth. J Health Psychol. 2017;22(5):537–547.
- Pletzer B, Lang C, Derntl B, et al. Weak associations between personality and contraceptive choice. Front Neurosci. 2022;16:898487.
- Beltz AM, Loviska AM, Kelly D. No personality differences between oral contraceptive users and naturally cycling women: implications for research on sex hormones. Psychoneuroendocrinology. 2019;100:127–130.