Abstract
After three decades of action research (AR) there are still questions about its application and contribution in comparison to traditional research methods. The aim of this paper is to explore and critique how two action research frameworks can be employed when improving healthcare processes. We also investigate the role of the Researcher in Residence when using AR in health operations management. Using Problem Resolving Action Research and Collaborative Action Research models we identify the benefits and challenges of conducting AR. To improve the reporting of action research we offer revised guidelines developed within the context of healthcare improvement that will assist both academics and practitioners when undertaking AR. The study also clarifies the important role of the researcher in residence which will assist academics and practitioners by providing consistency to terminology and understanding when undertaking AR research.
Introduction
Nearly three decades ago action research (AR) was introduced as a new paradigm for operations management research (Coghlan Citation1994; Westbrook Citation1995). AR is a research approach which originates from social psychology, where the researcher acts as a change agent (Lewin Citation1946) to help organisations to solve real-life problems (Altrichter et al. Citation2002). Similarly, Dickens and Watkins (Citation1999) position action research as a participative approach to addressing real world problems. Westbrook (Citation1995) purported AR was an approach that could address what he terms as three deficiencies associated with ‘traditional research topics and methods’. First was the relevance to practice. Second was how AR can be applied to developing, unstructured and integrative issues. Third was how AR can make a sound contribution to theory. Drawing on previous research, Coughlan and Coghlan (Citation2002) helpfully define the key characteristics of AR as being research in action, participative, happening at the same time as action and a defined approach to problem solving. AR is generally conducted in real time and ideally written as a live case study as it unfolds (Coughlan and Coghlan Citation2002). AR cases are interventions which aim to promote reflection and learning (Kleiner and Roth Citation1997) and more specifically where research informs practice, and practice informs research (Näslund Citation2002). This dual purpose of AR studies relies on a number of critical factors that must be considered by the researcher before undertaking an AR study (Coughlan and Coghlan Citation2016). These factors include:
a collaborative design involving practitioners and researchers,
iterative phases of the project which enables the researchers time to reflect and analyze the impact of the project on the organization, and for both researchers and practitioners to plan new action phases.
skilled team members (research and in practice) to actively manage the relationship and expectations between the practitioners and researchers.
Study aims and research questions
This paper specifically examines the role of AR in healthcare operations management. Early research in healthcare operations management relied on transferring models, applications and learning from manufacturing and services to various healthcare settings particularly to improve patient flow and scheduling (Singh, Scholtes, and Terwiesch Citation2020). More recently as the challenges within healthcare operations have been better understood, approaches and models have become bespoke to the sector. There has long been a call to shift from solely focusing on distinct parts of the healthcare system (e.g. waiting lists) to implementing whole system improvement (Costa and Filho Citation2016; Rich and Piercy Citation2013). From a recent review of 70 healthcare operations management papers, Singh, Scholtes, and Terwiesch (Citation2020) define five key areas which have attracted most attention. The first being operational variables for example how workload and arrival times of ED patients impact the delivery of care and patient outcomes. Second, the volume of activity and how this impacts cost, outcomes and service levels. Third, the streaming and directing of patients through patient pathways and the healthcare system, for example, getting the right patient, to the right place, at the right time. Fourth is patient safety and operational management and identifying how well placed these are to study system failures. Finally, process and system improvement which can encompass technology and innovation. It is this latter area which is the focus of this paper. We aim to further the understanding of using AR projects when improving healthcare systems and processes. Through the provision of two quality improvement cases, we examine how to guide the alignment of research and practice priorities in relation to an Action Research project on Healthcare Operations Management. In doing so we demonstrate the: Theoretical novelty; Research rigour; Practical relevance and usefulness; Applicability of the findings in other situations. It is not the intention to report the details of the improvement cases but examine the action research approach employed, the role of the researcher in residence and the interaction between the researcher and practitioners.
The article starts by exploring how AR has been applied within healthcare operations management. We then examine in more detail two action research models, Problem Resolving Action Research (PRAR) and collaborative action research (CAR) in order to clearly position the theoretical and methodological characteristics of the case activities introduced later in the paper. A presentation of the results follows, illustrating the application of both AR models. In the subsequent discussion section, we contend that there is a need to develop concepts that acknowledge the important role of the embedded researcher in residence and the nature of collaborative working with multi-professional partners. We emphasize the importance of protected time and space in which to undertake action research within contemporary, complex environments such as healthcare operations. In the final part of the paper, we provide some recommendations in which to improve the ways we undertake action research to improve the rigour and robustness of this important methodological approach which is often overlooked and not always considered scientific (Morrison and Lilford Citation2001) as mainstream or traditional research. Some proponents of action research are keen to distance AR from mainstream research and argue it is respectable and acceptable to engage in an iterative enquiry which brings about beneficial change sensitive to the context and increases understanding as it unfolds. Rather than mapping out everything from the start as with many traditional methods (Koshy, Koshy, and Waterman Citation2011). We also offer an adaptation of existing guidelines provided to report AR research for use in healthcare improvement.
Literature review: action research in healthcare operations management
Although we have seen an exponential increase in writing associated with service operations (Akmal et al. Citation2018) and specifically healthcare operations management over the last decade or so (Singh, Scholtes, and Terwiesch Citation2020), surprisingly the use of AR within the sphere of healthcare operations management research has not been given the same attention. This omission could reflect the fast pace and dynamic nature of healthcare and the often long and complicated governance requirements for researchers to undertake AR. AR within healthcare tends to focus on areas specific to the work context of the participants and the current problems and issues they are trying to solve such as defining and incorporating roles such as caregivers into a care pathway or it has focused on improving collaboration, engagement, or person-centred care. However, it is useful to review what areas of healthcare have been the subject of AR and what methodological approaches and frameworks have been developed and implemented.
Visintin et al. (Citation2017) undertook a multi-year research collaboration between the Department of Industrial Engineering of the University of Florence, and the Meyer Hospital. This AR study was commissioned by the senior team at the hospital with the objective of the performance of their operating theatres and increasing the competence of staff in healthcare operations management. The collaborative improvement project specifically examined the surgical scheduling process to develop skills and tools to aid the decision-making around scheduling and resource utilization. The team included in this AR project included academics and a multi-disciplinary team from the hospital which included senior managers such as general director, medical director, and the head of the planning department. A multi-method approach was taken which included direct observation, interviews, querying databases and analysis of internal documentation. This study reports on the outcomes of the AR collaboration which included reengineering the hospital’s surgical process and by developing and implementing a master surgical scheduler which also enhanced the skills and competences of the hospital staff (Visintin et al. Citation2017).
Marin-Garcia et al. (Citation2020) report on the first stages of an AR project designed to plan and schedule health resources in scenarios derived from the COVID-19 outbreak. They propose traditional approaches such as materials resource planning systems (MRP) used within manufacturing are unlikely to be able to cope with the complexity of healthcare. Therefore, the authors advocate for medical resource planning tools to be adapted for the uncertainty that characterizes a pandemic. They suggest simulation could be used to estimate the needs along with optimization models to plan resources. This paper only reports on the action planning of the AR project and not the implementation.
A more recent study by Van Heerden, Janse van Rensburg, and Maree (Citation2021) employed the Problem Resolving Action Research (PRAR) model (Piggot-Irvine Citation2009) to develop strategies to sustain a quality improvement initiative in neonatal resuscitation in a maternity section of a South African district hospital. The PRAR model consists of cycles of planning, acting, observing, and reflecting. The cycles of change aim to continuously improve the process or context in which it is being employed through the knowledge gained from observation and reflection. The participatory nature of the model promotes collaboration and ownership of the participants involved in bringing about change in their own practice and hence reducing the gap between theory and practice (Piggot-Irvine Citation2009). As a result of three cycles of change, the study showed practice was transformed and improvements were made in neonatal resuscitation skills. Health professionals were empowered through active participation in the study.
Buonaccorso et al. (Citation2022) also adopted a participatory approach to AR for a training experience (Smith, Rosenzweig, and Schmidt Citation2010) within a Specialized Palliative Care Service (SPCS) at an Italian hospital. An assessment test of an open-ended questionnaire was administered both pre-and post-training. The authors describe their approach as a ‘professionalizing type’ of AR (Hockley and Froggatt Citation2006) which aimed to respond to a problem defined by a professional group and relate to a behaviour of practitioners (Hockley and Stacpoole Citation2014; Smith, Rosenzweig, and Schmidt Citation2010). Given the sensitivity of the area of training the authors concluded that AR may be an effective way of improving programs that are to have a real impact on professionals’ practice in accordance with available resources and local context’s needs.
Integrating system dynamics (simulation) into AR was reviewed by Holmström et al. (Citation2022) through analyzing five improvement projects within healthcare. The authors analyzed the cases using a framework based on Rowbottom’s (Citation1977) original four AR related questions which examine what is known, assumed, extant and requisite about the situation. From their analysis of integrating systems dynamics with AR it was possible to achieve more useful and comprehensive outcomes than applying either one in isolation. AR assisted with the engagement of participants and the ownership of results than what was achievable by systems dynamics alone.
Interestingly, none of the papers reviewed here mention the specific role of the researcher and whether embedded within the research environment. The focus is more on reporting the action research study and the associated outcomes rather than a critical analysis of the methodology itself.
Action research and quality improvement in healthcare
As part of improving healthcare operations, we have seen a growing interest and application of quality improvement. Due to the applied and collaborative nature of quality improvement (QI) we feel AR has an important role to play and is the focus of this paper. QI focuses on making changes that will lead to better patient outcomes (health), better system performance (care) and better professional development (Batalden and Davidoff Citation2007). Crucially QI centres on the application of research evidence to improve health care practice.
There is a growing body of evidence of how quality improvement has been applied within acute (hospital) care, as this was the setting for several of the early national improvement programmes (e.g. Productive Ward – see Sarre et al. Citation2019). To extend the literature closer to the context of our research, here we review some of the limited examples of action research and quality improvement in healthcare. For example, Mosadeghrad and Afshari (Citation2021) examined the effects of a quality management model on a hospital’s operating theatre’s productivity levels using participatory action research. The authors describe the participatory action research (PAR) approach they took by a formal multi-disciplinary QI team who improved the occupational therapy operational processes using an eight-step quality management model known as the strategic collaborative quality management (SCQM). The design was described as an uncontrolled before-after study and PAR was used for the intervention along with insider action research (IAR) as one of the researchers worked for the hospital and was also a MSc student. The other researcher was the student’s academic supervisor who advised and supported the student throughout the research project. The PAR for the study was guided by Mosadeghrad’s (Citation2013) eight-step SCQM model which included standardizing work processes, setting objectives for processes, analyzing the processes to identify problems, developing solutions, planning changes, implementing improvement plans, evaluation outcomes and actioning results and standardizing processes. Outcomes of the project are provided which include increased productivity, reduction in cancellations, improved staff satisfaction and a reduction in patient complaints (Mosadeghrad and Afshari Citation2021). The PAR methodology, which is essentially following the SCQM model, is described as being systematic and robust for applying changes to real problems, with the recommendation to be applied by healthcare managers and practitioners. Again, no information is provided on the role of the researchers and what criteria were used to judge the rigour and robustness of the PAR methodology.
Action research and (embedded) researchers in residence
For the purposes of this paper, we draw on the collaborative and participatory nature of the AR method where researchers engage with health professionals longitudinally in the design and implementation of research, working with them as opposed to externally studying them (Jagosh et al. Citation2012; Meyer Citation2000). This symbiotic role is situated at the nexus of needs of the health service with academic knowledge and expertise. As such real-life experiential expertise (clinical and/or patient) is introduced to frame research questions that matter to the health service combining with empirical and scientific knowledge that will facilitate scaling up and sustainability. Churruca et al. (Citation2019) helpfully review the benefits and challenges of embedded research within the context of implementation research and improving healthcare services. They present a model of four approaches ranging from dichotomized research-practice, where the researchers and implementers work completely separately with little to no communication to deep immersion, which brings together clinicians, researchers and clinician-researchers all working in one health care system. The benefits of the embedded approaches are reported as improved buy-in and access, ensuring rigour, ability to assess change and the approaches used, understanding context, sharing knowledge, expertise and skills, and jointly ensuring the success of the project. Whereas the challenges to undertaking embedded research include possible compromising objectivity, working to differing agendas, various ways of working, cultural differences, varying timelines and differing views on performance and long-term goals (Churruca et al. Citation2019; Marshall et al. Citation2016; Vindrola-Padros et al., Citation2019).
In summary the aim of this paper is to explore how two AR frameworks can be employed when improving healthcare processes. We also investigate the role of the Researcher in Residence when using AR in health operations management.
Materials and methods
Materials – two cases
Two healthcare cases conducted over a two-year period (2020–2022) were studied. A summary of the case characteristics is given below. The cases were selected on the involvement and experiences of one of the authors. Both cases focus on improving healthcare processes, Case 1 is based in Children Services and Case 2 Early Years Therapies. Both were aiming to improve healthcare operations and the redesign of services. The selection criteria for the cases were:
Defined project as part of an improvement collaborative.
The project followed a structured approach e.g. Plan Do Study Act (PDSA) cycle (Deming Citation1982).
Duration was at least 9 months.
Project team was multi-professional and included a researcher in residence.
AR methodology was appropriate for the project and was able to provide actionable solutions to the problems proposed by the project teams.
Case 1 was undertaken with a University Health Board located in Wales, UK (for more detail see Griffiths et al. Citation2022). The improvement project was part of a 9-month quality improvement collaborative. The team represented children services and the problem was identified as the need to improve the quality of referrals to their service. Using PDSA cycles the team worked with several of their key referrers in awareness raising and education sessions to improve the quality of referrals.
Case 2 follows on from the first case by focusing on one key referrer, health visitors to the early years’ therapists’ team. Again, a multi-disciplinary team of therapists worked with an embedded researcher in residence to equip health visitors with the knowledge of the therapy services and the resources to ensure requests for help are appropriate and right first time to reduce non-value adding time of triaging inappropriate referrals.
We selected two cases that were similar in context to allow comparisons to be drawn in relation to the use of action research within these improvement projects and to assess the role and interaction with the embedded researcher in residence.
Data analysis
All data collected during the ‘real life’ case studies were reviewed. These included notes from project meetings, outputs from using quality improvement tools and techniques and the role of the researcher in residence.
The AR analysis of the cases was conducted by both authors. We used Deming’s (Citation1982) PDSA cycle to review the studies along with two AR frameworks. The PDSA cycle provided a structured approach in which to present the project data and the two AR frameworks enabled us to review the role of the researchers in residence within the project along with understanding the wider implications of using AR to improve the operations of healthcare.
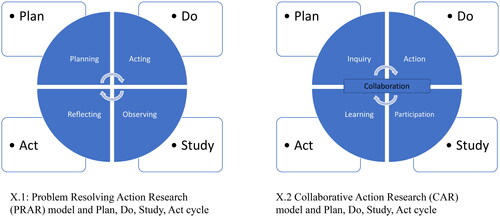
The first case was analyzed using the PRAR framework (Piggot-Irvine Citation2009). This model consists of three iterative cycles that start with defining the issues. Each cycle consists of four stages – observe, reflect plan and act (). The first cycle examines the existing situation and may result in spin off cycles to ensure there is a good understanding of current practice and any issues that may thwart making improvements. The second cycle focuses on implementation change and again may result in spin off cycles before reaching the final cycle which evaluates the change(s) which have been implemented. This final cycle can lead to further reflection, reporting and continued action. The model is designed to enhance collaboration between researchers and practitioners and focus on enabling change (Pirgot-Irvine, 2009). The following key steps are used to operationalize PRAR:
Figure 1. Aligning problem resolving action research (PRAR) model (Piggot-Irvine Citation2009) and collaborative action research (CAR) model (Kemmis and McTaggart Citation2005) with the plan, do, study, act cycle. X.1: Problem Resolving Action Research (PRAR) model and Plan, Do Study, Act cycle. X.2 Collaborative Action Research (CAR) model and Plan, Do Study, Act cycle.
Identifying the research problem or issue to be addressed: This can be done through discussions with team members, stakeholders, and researchers.
Planning and designing the research: The next step is to plan and design the research study. This involves selecting appropriate research methods, data collection techniques, and analysis tools.
Collecting data: The data collection involves collecting data from multiple sources. This can be done through interviews, focus group discussions, surveys, and other methods.
Analysing data: The next step is to analyse the data. This involves using appropriate analytical tools and techniques to identify patterns, trends, and themes in the data.
Developing and implementing action plans: Based on the findings of the data analysis, action plans are developed and implemented. These plans are developed in collaboration with team members, stakeholders, and researchers to ensure that they are relevant and effective.
Evaluating the outcomes: The final step in PRAR action research is to evaluate the outcomes of the action plans. This involves assessing whether the action plans were effective in addressing the research problem and achieving the desired outcomes (Greenwood and Levin Citation2007; Pirgot-Irvine, 2009; Reason and Bradbury Citation2008).
For the second case we follow a similar process but use the CAR framework. Like PRAR, CAR involves collaboration between researchers and participants to identify problems, develop and implement interventions and evaluate outcomes. It encourages the involvement of participants at all stages of the research process (Stringer Citation2013). The key stages of CAR are noted as:
Collaboration: active engagement of participants/stakeholders from defining the problem to evaluating the outcomes.
Inquiry: iterative process which encourages ongoing inquiry and reflection from the researchers and the participants/stakeholders
Action: production of tangible outcomes and promoting change and improvement
Participation: active participation from researchers and participants in all stages of the research process
Learning: promote learning and development among participants and researchers (Kemmis and McTaggart Citation2005).
CAR requires researchers to become gatekeepers, build relationships, seek legitimacy, navigate power, and impart traditional and technical research skills (Bennett and Brunner Citation2022).
Ethical considerations
Because both projects addressed evaluating and improving the quality of services, the case organization did not require ethics approval or specific informed consent procedures. Nevertheless, all participants were informed about the improvement projects, the purpose of the data collection and information was handled as confidential and reported anonymously.
Results
It is not the intention to report in detail the results of the cases as the focus of this paper is to assess the application of AR and the role of the researcher in residence. Therefore we report on the results of the study by first providing a brief overview of the two QI cases (). We then go on to discuss the application of AR.
Table 1. Overview of QI cases.
Application of the PRAR model
We use the PRAR model which is aligned well to the PDSA approach employed by the participants to share the learning captured by the researcher in residence to capture the application of AR in both cases. The researcher in residence was on a secondment with the case organization with a remit to support the quality improvement team in their endeavours to work with frontline teams wishing to improve systems and processes within their clinical areas. As part of the first case organization’s nine-month quality improvement collaborative, the researcher was allocated to facilitate the Case 1 team () in their pursuit to improve the quality of referrals to children services. The PRAR model encourages collaboration between the researcher, the frontline team, other staff members and the QI team. As part of the first PRAR cycle of defining the issue and examining the existing situation, the facilitation at this early stage of the improvement project enabled the researcher to encourage the project team to consult the relevant published academic and grey literature. This review informed the design of the cycles of change in terms of what improvements had been used in similar services or situations. Baseline data were collected during this first PRAR cycle. In some instances, data were readily available to the team from existing IT systems, in other instances it was necessary to conduct manual audits in order to capture information about returned inappropriate or incomplete referrals. These data needed to be collected by the project team as the researcher in residence was unable to access the organization’s IT systems. This was mainly due to data sharing agreements and the governance around confidentiality of patient data and GDPR. Similar issues also occurred with the use of portals to share project documentation. An extended process was required for IT to grant external users such as the researcher in residence.
Reflection plays an important part in the PRAR cycle. Project time within the collaborative programme was the opportunity for the practitioners to reflect on their projects and progress made to date. Once returned to operational roles reflection was largely for the researcher in residence to review actions and next steps. Busy practitioners were usually time poor and the opportunity to reflect on improvement outcomes and opportunities was limited unless part of protected time as part of a formal programme or continual professional development. The researcher in residence assumed the role of presenting anonymised data in a format (e.g. run charts) that was appropriate to the improvement project and recording details of the small cycles of change undertaken by the team. It was imperative these data were recorded as the project progressed to ensure accuracy, transparency and rigour of the iterative PDSA cycles and improvements made.
A robust approach to collecting data is also important to the rigour of AR. The collaborative element of the action research ensured data were captured at the time of each cycle and reducing the need for team members to recall activities and outcomes. The researcher also imparted knowledge on research design in terms the structuring PDSA cycles and iterative changes. Often practitioners did not fully recognize the real value of the research they were conducting or the fact it as considered to be action research. Most of the team members understanding of research was closer to medical science in relation to randomized control trials and before and after studies. Understandably efforts were more focused on making improvements and improving outcomes for patients and their families than identifying research outcomes. It was the role of the researcher to explore how the data compared with previous research and encourage discussions with the practitioners about the implications of the findings in terms of practice within the organization and possibly other stakeholders (e.g. families).
Application of the CAR model
For the second case we employed the CAR model which first focuses on gaining active engagement and collaboration from the participants. The researcher in residence was not previously known to the team. Therefore prior to the collaborative programme starting the researcher organized an online meeting to meet the team and outline the programme. This also helped the researcher to understand what the team members hoped to achieve by attending the programme and their project. The PDSA format encouraged the team to carefully define their problem statement and predict the desired outcomes. Similar to the first case, it was the PDSA cycles that prompted the ongoing inquiry of the team as they implemented small cycles of change. Teams were guided by the researcher to ensure only one change was trialled at a time and that the changes remained manageable within the timescale of the project. Much of the initial discussions focused on narrowing the scope of the improvement project to something that was within the control of the multi-professions represented within the team.
The researcher encouraged the team to capture the learning after each PDSA cycle which led to the awareness raising and education sessions being redesigned based on feedback received from HVs. The development of the online app was a good tangible outcome for the team which has promoted change and improvement in the quality of requests for help.
There was active participation between the researcher and the practitioners throughout the QI collaborative programme and beyond. The researcher was able to share knowledge and experience of undertaking QI within healthcare, but it was the team that had the in-depth knowledge of the context and which community teams to approach to be involved in pilot activities and cycles of change. The researcher continually encouraged the team to record their learning of QI tools and techniques and how they might use these in a wider context outside of their improvement project. Several of the practitioners reported using their learning with other colleagues outside of the immediate QI team. One team member also registered to become a QI buddy coach by joining the next cohort of the QI collaborative.
Having a researcher in residence involved in the study enabled practitioners to protect their project time and fully engage with the QI project. It was the researcher who set up and chaired project meetings. The project being formally recognized as part of the organization’s quality strategy also legitimized the researcher’s role and the practitioners’ efforts.
Action research and healthcare improvement
Drawing on our analysis we can see there are similarities but there are also some subtle differences when using PRAR and CAR (). By employing both models in our case analysis, we have provided a broader critique of AR more generally.
Table 2. Similarities and differences between PRAR and CAR models.
PRAR places more emphasis on problem definition, action planning and evaluating outcomes, all of which are central to QI. Whereas the defining attributes of CAR are the promotion of learning and development and promoting change and improvement, key for improving healthcare systems. The iterative nature of the PRAR and CAR aligns well with the PDSA cycle used to drive improvement of the healthcare cases (). From our application of PRAR and CAR we have identified the benefits and challenges of employing AR in healthcare improvement () which includes the role of researcher in residence. We therefore suggest that a combination of both models could improve the way in which we approach AR in quality improvement.
Table 3. Benefits and challenges of using AR in healthcare improvement.
Discussion
Participatory research, such as action research, aims to transform power relations. By challenging conventional processes of knowledge production, while maintaining a standpoint of researching with, rather than researching on, communities (Boser Citation2006). To examine how AR has been applied within healthcare operations management, two AR models were used to report on the learning from two quality improvement projects. Both project teams were multi-professional and included a researcher in resident as their QI coach. The knowledge of QI methods was shared by the researcher but the knowledge of context in which these were employed was held by the practitioners. The well-established PDSA framework was introduced by the researcher with the application in practice being led by the practitioners. The researcher encouraged collection of baseline data with the actual interrogation of IT systems to access the data being undertaken by the practitioners. The ability to share knowledge that is accessible to both researchers and practitioners is crucial to managing the power relations and the collaboration between academic and non-academic partners (Bergold and Thomas Citation2012). Some scholars have questioned whether AR and other participatory methods have led to equitable power relations (Gaventa and Cornwall Citation2008). Although in both cases the researcher was embedded in the organization, this does not appear to be a sufficient substitute for the contextual knowledge held by the practitioners. This may reflect the complexities that often bestow healthcare systems and processes. It is unlikely that researchers could be embedded within a healthcare organization for an extended period needed to fully appreciate the context in which improvements are being made. Therefore, it is important to formally acknowledge the expertise and value each group brings. Previous research has positioned AR as being able to challenge how knowledge is conventionally produced by being able to research with communities and practitioners (Boser Citation2006). The strengths of AR are combining the professional and experiential knowledge of practitioners and researchers along with ensuring knowledge sufficiency in other areas (e.g. context for researchers, methods for practitioners), which may develop over the period of the project.
Both action research models employed within this study include a reflective cycle which involves close exchanges between practitioners and researchers (Cullen Citation1998). Such exchanges also promote the connection between objectivity and subjectivity. Embedding well-established frameworks within the AR models assists practitioners in understanding and defining objective measures, data, and outcomes and with the assistance and often challenge from the researcher what might be considered as being more subjective. This process can be assisted with the availability of data and the reviewing of previous research which is often promoted by the researcher in residence. This role of the researcher of bringing together knowledge generation and evidence is paramount for improving healthcare systems and processes, along with the need to encourage reflection and challenge to the practitioners (Phillips, Kristiansen, and Vehviläinen Citation2013).
Earlier we noted the limited detail of the specific roles of practitioners and researchers within action research. Previous AR has also questioned the balance of power between these two parties. As a result of our analysis, we propose a framework () that suggests how academics, especially researchers in residence, and practitioners need to collaborate to enhance the quality of AR. We suggest during the early stages of the AR project that the theoretical novelty is defined. This is a collaborative process which may involve the researcher instigating a review of previous research and the outcome informs the study design which is jointly developed by the practitioners and the researcher. This process creates new social structures and relationships, as well as stimulating debate about key methodological issues such as positionality, ethics/governance, and research design (Avgitidou Citation2009; Platteel et al. Citation2010).
We suggest that the rigour of the AR design is mainly developed by the researcher through employing appropriate research methods to the defined problem. In the case of the two cases the PDSA cycles provided a framework which the practitioners could follow. Focus groups were also employed in one of the cases to supplement baseline data collected by the practitioners. Guidance from the embedded researcher ensured that project activities were undertaken with rigour and recorded appropriately for a research project. The practical relevance of the project and its outcomes was the work of the practitioners. Sometimes this might require some translation from the theoretical underpinnings established by the researcher when instigating the review of previous research. The applicability of the results was led by the practitioners, whereas the contribution to knowledge was left to the researcher to define.
As to whether the results of the improvement projects were applicable to other situations. This was partially led by the practitioners who were able to identify areas within the case organization to spread the improvement (e.g. to other sites and other children services which received request for help).
Role of the researcher in residence
Previous research has described the various traditional roles undertaken by AR researcher (e.g. Bennett and Brunner Citation2022) which include gatekeeper, negotiator and, relationship builder and researcher. Our findings indicate that a researcher in residence has some additional roles to play when involved in collaborative improvement work which are: translator (of academic terminology), theorist, facilitator/coach and critical friend ().
Table 4. Role of the researcher in residence.
When researchers are embedded in the organization there are clear benefits in terms of gaining access, levels of collaboration, shared language, and improved communication. However, this blurring of academic and practice boundaries could impact objectivity. Employing AR models and frameworks will guide AR researchers when setting up and undertaking their research limiting the effect of impacted objectivity and so delivering more impactful outcomes. The use of recognized guidelines will also help when reporting and publishing AR as it does not necessarily conform to established report writing conventions (Smith, Rosenzweig, and Schmidt Citation2010), leaving researchers to their own devices and possibly trying to force fit their results to existing reporting and publishing mechanisms. Developing consistency in reporting is essential to maintain and promote the undertaking of high-quality AR studies.
Recommendations for reporting AR studies
There appears to be limited availability of existing guidelines to report AR studies. Smith, Rosenzweig, and Schmidt (Citation2010) provide best practice guidelines in the reporting of participatory action research operationalized within the area of counselling and psychology. From comprehensively studying the participatory AR and community-based participatory literature the authors developed best practice guidelines for reporting of participating AR (Smith, Rosenzweig, and Schmidt Citation2010). As a result of our analysis of using AR in improving healthcare operations we have reviewed and adapted these reporting guidelines to reflect doing AR within a healthcare operations management context which includes an embedded researcher. We have merged our recommendations () with the existing Standards for Quality Improvement Reporting Excellence (SQUIRE) 2.0 guidelines (Ogrinc et al. Citation2016) which are used to report new knowledge about how to improve healthcare.
Table 5. Reporting guidelines for action research in healthcare operations management.
When planning the AR project plan, the structure and organization of the report or article to be written, this may require the adaptation of conventional headings used for organizational reporting (e.g. Situation, Background, Assessment and Recommendations (SBAR) – used extensively in healthcare) or academic journals. Details of the AR methodology employed need to be described and justified in particular any ethical and governance considerations. The role of the (embedded) researcher should be clarifed and the interaction with the case organization(s). Timelines for the AR should be given along with details of the iterative nature of data collection and analysis. Providing greater clarity of the methodology employed and the reflective learning and how this is reported will enhance the rigour and novelty of AR studies and identify the contributions to knowledge.
Conclusion
The aim of this study was to guide the alignment of research and practice priorities in relation to two cases which focused on improving healthcare systems and processes. We have provided the benefits and challenges of applying AR within healthcare operations management, along with examining the practical relevance and usefulness of AR specifically within quality improvement. We have examined the role of the researcher in residence and extended what was seen as the traditional role of the AR researcher. Finally, we provide a revised version of reporting guidelines for AR research which we believe will improve the way in which AR is undertaken when improving healthcare operations management. These guidelines are for action researchers to test and adopt to suit other areas of operations management AR research.
The limitations of this study are the reflective nature of the case analysis. However, the study has enabled us to review the application of AR models, identify the synergies between two AR frameworks and recommend guidelines on how to report participatory action research in healthcare operations management. Further research is needed to test the guidelines with a view to these being employed by researchers and practitioner involved in AR. Building on the work of Smith, Rosenzweig, and Schmidt (Citation2010) we anticipate improving the rigour, transparency, and robustness of AR the guidelines will need to be established on a similar footing to other renown reporting guidelines such as COREQ which is used for reporting research using interviews and focus groups (Booth et al. Citation2014).
Implications for practitioners
Action research may not always be seen as the most credible methodological approach among healthcare practitioners and researchers. However, when applied with rigour it is certainly a plausible option particularly within the applied field of improving healthcare operations. To increase its application in practice this paper examines two frameworks which can be aligned to well-versed QI approaches such as the PDSA cycle. Practitioners need to recognize the value and the role that AR can play in improving healthcare operations and if executed well can be a good opportunity to publish their efforts. The two cases included in this paper illustrate the application of AR within the context of QI, which along with the guidelines provide a starting point and road map to enable practitioners to plan, implement and report their practice-based improvement research. The road map increases the accessibility to action research, promotes the usefulness of AR in practice (Coughlan and Coghlan Citation2002) and responds to the call to increase the practical relevance of OM research by assisting practitioners in their real problem-solving efforts (Childe Citation2011). Similarly, it helps to bridge the gap between theory and practice and demystifies how researchers and practitioners can work together to research and address real-life problems.
It is also important to note the realities of undertaking AR in healthcare and the fluidity of QI and other project teams due to resource constraints and staff shortages. This often results in different projects and tasks being shared across members of the team. Having clarity on how to conduct and report AR projects provides a road map for completion.
Implications for researchers
Here we note the importance of the researcher in residence role which provides methodological insight and rigour to both improvement and action research. We have extended the traditional action researcher’s role to reflect the embedded nature of the researcher in residence post particularly within the context of improving healthcare systems and processes. This is important as we note the possible fluidity of the project team with the role of the researcher in residence therefore providing constancy and continuity to the AR project.
This study uncovers some of the myths around the research in residence role for both academics and practitioners and provides greater clarity as to how AR can be implemented when improving healthcare operations. We anticipate this level of clarity will also facilitate the engagement of healthcare professionals and managers and enhance the importance of patient engagement in AR. Further testing of the guidelines is needed in healthcare and other public service settings. It is anticipated using these guidelines will enhance the rigour and transparency of AR research along with improving the way that we report this research.
As with practitioners, we hope the road map will increase the use of AR among academics especially those occupying hybrid and seconded roles which support practitioners in their improvement and research efforts.
Acknowledgements
We would like to thank the healthcare staff and colleagues involved in both cases.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The author has chosen a standard agreement for this article and will not push through with open access.
Additional information
Notes on contributors

Stephanie Best
Stephanie Best is an associate Professor and an implementation scientist based at the University of Melbourne. She is the senior implementation science research lead at Peter MacCallum Cancer Centre and Australian Genomics. She has an extensive international clinical and health care management background as a Chartered Physiotherapist. Stephanie has more than a decade of research experience in implementation, working with a wide range of health and social care practitioners and other stakeholders. A/Prof Best has a track record of designing and delivering international, national and state-wide implementation projects. She has extensive leadership and health service experience e.g. senior fellow of the Higher Education Academy (UK), co-chair Melbourne Academic Centre for Health Implementation Science committee and associate editor for BMC Health Services Research. Stephanie is a member of the Swansea Centre for Improvement and Innovation in Health & Social Care. Her research interests include Implementation of complex interventions, Clinical Genomics, Professional Identity, Equity and Cancer Care.

Sharon J. Williams
Sharon J. Williams is a Professor with the School of Health and Social Care, Swansea University where she leads the Swansea Centre for Improvement and Innovation in Health & Social Care. She is also on a part-time secondment with a Welsh Health Board as a Professor in Quality Improvement and Patient Experience. Formerly, Sharon was an Improvement Science Fellow with the Health Foundation. She has a background in operations management, supply chain management and quality improvement. Sharon teaches and supervises students on Swansea’s MSc in Health Care Management. She completed her PhD with the Lean Enterprise Research Centre at Cardiff Business where she also undertook research within various industries. Her research interests include Quality improvement, Pathway redesign, Co-production/Co-design, Evaluations, Professional identity and integrated teams in health and social care.
References
- Akmal, A., N. Podgorodnichenko, R. Greatbanks, and A. M. Everett. 2018. “Bibliometric Analysis of Production Planning and Control (1990–2016).” Production Planning & Control 29 (4): 333–351. https://doi.org/10.1080/09537287.2018.1429030
- Altrichter, H., S. Kemmis, R. McTaggart, and O. Zuber-Skerrit. 2002. “The Concept of Action Research.” The Learning Organization 9 (3): 125–131. https://doi.org/10.1108/09696470210428840
- Avgitidou, S. 2009. “Participation, Roles and Processes in a Collaborative Action Research Project: A Reflexive account of the Facilitator.” Educational Action Research 17 (4): 585–600. https://doi.org/10.1080/09650790903309441
- Batalden, P., and F. Davidoff. 2007. “What is “Quality Improvement” and How Can It Transform Healthcare?” Quality & Safety in Health Care 16 (1): 2–3. https://doi.org/10.1136/qshc.2006.022046
- Bennett, H., and R. Brunner. 2022. “Nurturing the Buffer Zone: conducting Collaborative Action Research in Contemporary Contexts.” Qualitative Research 22 (1): 74–92. https://doi.org/10.1177/1468794120965373
- Bergold, J., and S. Thomas. 2012. “Participatory Research Methods: A Methodological Approach in Motion.” Forum: Qualitative Social Research 13 (1): 30.
- Booth, A., K. Hannes, A. Harden, J. Noyes, J. Harris, and A. Tong. 2014. “COREQ (Consolidated Criteria for Reporting Qualitative Studies).” In Guidelines for Reporting Health Research: A User’s Manual, edited by D. Moher, D. Altman, K. Schult, I. Simera, and E. Wager. New York: John Wiley & Sons Ltd.
- Boser, S. 2006. “Ethics and Power in Community-Campus Partnerships for Research.” Action Research 4 (1): 9–21. https://doi.org/10.1177/1476750306060538
- Buonaccorso, L., S. Tanzi, S. Sacchi, S. Alquati, E. Bertocchi, C. Autelitano, E. Taberna, and G. Martucci. 2022. “Self-Care as a Method to Cope with Suffering and Death: A Participatory Action-Research Aimed at Quality Improvement.” Frontiers in Psychology 13: 769702. https://doi.org/10.3389/fpsyg.2022.769702
- Childe, S. 2011. “What Are the Hot Topics in the Management of Operations, Editorial.” Production Planning & Control 22 (7): 611–611. https://doi.org/10.1080/09537287.2011.619333
- Churruca, K., K. Ludlow, N. Taylor, J. Long, S. Best, and J. Braithwaite. 2019. “The Time Has Come: Embedded Implementation Research for Health Care Improvement.” Journal of Evaluation in Clinical Practice 25 (3): 373–380. https://doi.org/10.1111/jep.13100
- Coghlan, D. 1994. “Research as a Process of Change: Action Science in Organisations.” Irish Business and Administrative Research 15: 119–130.
- Costa, L. B. M., and M. G. Filho. 2016. “Lean Healthcare: Review, Classification and Analysis of Literature.” Production Planning & Control 27 (10): 823–836. https://doi.org/10.1080/09537287.2016.1143131
- Coughlan, P., and D. Coghlan. 2002. “Action Research for Operations Management.” International Journal of Operations & Production Management 22 (2): 220–240. https://doi.org/10.1108/01443570210417515
- Coughlan, P., and D. Coghlan. 2016. “Action Research.” In Research Methods for Operations Management, edited by C. Karlsson, 233–267. Abingdon, Oxfordshire: Routledge Publishers.
- Cullen, J. 1998. “The Needle and the Damage Done: Research, Action Research and the Organizational and Social Construction of Health in the “Information Society.” Human Relations 51 (12): 1543–1564. https://doi.org/10.1177/001872679805101207
- Deming, W. Edwards. 1982. Out of the Crisis, Center for Advanced Engineering Study. Cambridge, Massachusetts: Massachusetts Institute of Technology.
- Dickens, L., and K. Watkins. 1999. “Action Research: Rethinking Lewin.” Management Learning 30 (2): 127–140. https://doi.org/10.1177/1350507699302002
- Gaventa, J., and A. Cornwall. 2008. “Power and Knowledge.” In The SAGE Handbook of Action Research: Participative Enquiry and Practice, edited by P. Reason and H. Bradbury, 172–189. Los Angeles, USA: Sage Publications Ltd.
- Greenwood, D., and M. Levin. 2007. Introduction to Action Research: Social Research for Social Change. London, UK: Sage Publications Ltd.
- Griffiths, S., P. Large, T. Lewis, A. Smiriglia, C. Thomas, K. Thomas, S. Waters-Foster, L. Watkins, S. Willard, and S. Williams. 2022. “Implementing the Care Aims Approach in Children’s Services: A Quality Improvement Pilot Study.” British Journal of Healthcare Management 28 (7): 190–195. https://doi.org/10.12968/bjhc.2020.0183
- Hockley, J., and K. Froggatt. 2006. “The Development of Palliative Care Knowledge in Care Homes for Older People: The Place of Action Research.” Palliative Medicine 20 (8): 835–843. https://doi.org/10.1177/0269216306073111
- Hockley, J., and M. Stacpoole. 2014. “The Use of Action Research as a Methodology in Healthcare Research.” European Journal of Palliative Care 21: 110–114.
- Holmström, P., T. Björk-Eriksson, P. Davidsen, F. Bååthe, and C. Olsson. 2022. “Insights Gained from a Re-Analysis of Five Improvement Cases in Healthcare Integrating System Dynamics into Action Research.” International Journal of Health Policy and Management 11 (11): 2707–2718. https://doi.org/10.34172/ijhpm.2022.5693
- Jagosh, J., A. Macaulay, P. Pluye, J. Salsberg, P. Bush, J. Henderson, E. Sirett, et al. 2012. “Uncovering the Benefits of Participatory Research: Implications of a Realist Review for Health Research and Practice.” The Milbank Quarterly 90 (2): 311–346. https://doi.org/10.1111/j.1468-0009.2012.00665.x
- Kemmis, S., and R. McTaggart. 2005. “Participatory Action Research: Communicative Action and the Public Sphere.” In The Sage Handbook of Qualitative Research, edited by N. K. Denzin and Y. S. Lincoln, 559–604. London: Sage Publications.
- Kleiner, C., and G. Roth. 1997. “How To Make Experience Your Company’s Best Teacher.” Harvard Business Review 75 (5): 172–177.
- Koshy, E., V. Koshy, and H. Waterman. 2011. Action Research in Healthcare. London: Sage Publications Ltd.
- Lewin, K. 1946. “Action Research and Minority Problems.” Journal of Social Issues 2 (4): 34–46. https://doi.org/10.1111/j.1540-4560.1946.tb02295.x
- Malcomess, K. 2005a. “The Care Aims Framework.” Accessed April 23, 2023. https://careaims.com/about-care-aims/the-care-aims-framework/.
- Malcomess, K. 2005b. “The Care Aims Model.” In Speech and Language Therapy: Issues in Professional Practice, edited by C. Anderson and A. Van der Gaag. London, UK: Whurr Publishers.
- Marin-Garcia, J., J. Garcia-Sabater, A. Ruiz, J. Maheut, and J. Garcia-Sabater. 2020. “Operations Management at the Service of Health Care Management: Example of a Proposal for Action Research to Plan and Schedule Health Resources in Scenarios Derived from the COVID-19 Outbreak.” Journal of Industrial Engineering and Management 13 (2): 213–227. https://doi.org/10.3926/jiem.3190
- Marshall, M., L. Eyre, M. Lalani, S. Khan, S. Mann, D. de Silva, and J. Shapiro. 2016. “Increasing the Impact of Health Services Research on Service Improvement: The Researcher‐in‐Residence Model.” Journal of the Royal Society of Medicine 109 (6): 220–225. https://doi.org/10.1177/0141076816634318
- Meyer, J. 2000. “Using Qualitative Methods in Health-Related Action Research.” British Medical Journal 320 (7228): 178–181. https://doi.org/10.1136/bmj.320.7228.178
- Morrison, B., and R. Lilford. 2001. “Action Research and Health Services: Theory and Application.” Qualitative Health Research 11 (4): 436–449. https://doi.org/10.1177/104973201129119235
- Mosadeghrad, A. 2013. “Verification of a Quality Management Theory: Using a Delphi Study.” International Journal of Health Policy and Management 1 (4): 261–271. https://doi.org/10.15171/ijhpm.2013.55
- Mosadeghrad, A., and M. Afshari. 2021. “Quality Management Effects on Operating Theater’s Productivity: A Participatory Action Research.” The TQM Journal 33 (4): 882–895. https://doi.org/10.1108/TQM-04-2020-0083
- Näslund, D. 2002. “Logistics Needs Qualitative Research–Especially Action Research.” International Journal of Physical Distribution & Logistics Management 32 (5): 321–338. https://doi.org/10.1108/09600030210434143
- Ogrinc, G., L. Davies, D. Goodman, P. Batalden, F. Davidoff, and D. Stevens. 2016. “SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence): Revised Publication Guidelines from a Detailed Consensus Process.” BMJ Quality & Safety 25 (12): 986–992. https://doi.org/10.1136/bmjqs-2015-004411
- Phillips, L., Kristiansen, M., Vehviläinen, M. (eds) 2013. Knowledge and Power in Collaborative Research. London, UK: Routledge Publishers.
- Piggot-Irvine, E. 2009. Action Research in Practice. Wellington, New Zealand: NZCER Press.
- Platteel, T., H. Hulshof, P. Ponte, J. van Driel, and N. Verloop. 2010. “Forming a Collaborative Action Research Partnership.” Educational Action Research 18 (4): 429–451. https://doi.org/10.1080/09650792.2010.524766
- Reason, P. & Bradbury, H. (Eds.). 2008. The SAGE Handbook of Action Research: Participative Inquiry and Practice. 2nd ed. London: Sage Publications Ltd.
- Rich, N., and N. Piercy. 2013. “Losing Patients: A Systems View on Healthcare Improvement.” Production Planning & Control 24 (10–11): 962–975. https://doi.org/10.1080/09537287.2012.666911
- Rowbottom, R. 1977. Social Analysis: A Collaborative Method of Gaining Usable Scientific Knowledge of Social Institutions. London: Heinemann Educational.
- Sarre, S., J. Maben, P. Griffiths, R. Chable, and G. Robert. 2019. “The 10-Year Impact of a Ward-Level Quality Improvement Intervention in Acute Hospitals: A Multiple Methods Study.” Health Services and Delivery Research 7 (28): 1–172. https://doi.org/10.3310/hsdr07280
- Singh, D., S. Scholtes, and C. Terwiesch. 2020. “Empirical Research in Healthcare Operations: Past Research, Present Understanding and Future Opportunities.” Manufacturing & Service Operations Management 22 (1): 73–83. https://doi.org/10.1287/msom.2019.0826
- Smith, L., L. Rosenzweig, and M. Schmidt. 2010. “Best Practices in the Reporting of Participatory Action Research: Embracing Both the Forest and the Trees.” The Counseling Psychologist 38 (8): 1115–1138. https://doi.org/10.1177/0011000010376416
- Stringer, E. 2013. Action Research. London: Sage Publications Ltd.
- Van Heerden, C., E. Janse van Rensburg, and C. Maree. 2021. “Action Research as Sustainable Healthcare Quality Improvement: Advances in Neonatal Care Emphasising Collaboration, Communication and Empowerment.” Action Research 19 (4): 710–727. https://doi.org/10.1177/1476750319896839
- Vindrola-Padros, C., L. Eyre, H. Baxter, H. Cramer, B. George, L. Wye, N. J. Fulop, et al. 2019. “Addressing the Challenges of Knowledge co‐Production in Quality Improvement: learning from the Implementation of the Researcher‐in‐Residence Model.” BMJ Quality & Safety 28 (1): 67–73. https://doi.org/10.1136/bmjqs-2017-007127
- Visintin, F., P. Cappanera, C. Banditori, and P. Danese. 2017. “Development and Implementation of an Operating Room Scheduling Tool: An Action Research Study.” Production Planning & Control 28 (9): 758–775. https://doi.org/10.1080/09537287.2017.1310328
- Westbrook, R. 1995. “Action Research, a New Paradigm for Research in Production and Operations Management.” International Journal of Operations & Production Management 15 (12): 6–20. https://doi.org/10.1108/01443579510104466