ABSTRACT
Symptomatic HIV-associated neurocognitive disorder (HAND) is a complication of HIV (cognitive impairment, difficulties with everyday functioning). If detected early, interventions assist with optimizing care, avoiding rapid decline and enhancing coping. There remains inconsistency surrounding screening/diagnosis information within Australian healthcare professionals and community settings. A scoping review of academic literature, government policies and non-government organisations (NGOs) was conducted to map existing screening/diagnosis information using the guidelines of Joanna Briggs Institute. A literature search of EBSCOhost and Medline (dates: 2015–2021), the Australian government NGO web domains, Google and unpublished academic works was conducted (July 2021) and updated (December 2022) to identify Australian items (past 5 years). Seventeen items met the inclusion criteria. No government guidelines were identified. Various HIV-related organisations proposed different diagnostic guidelines. Most HAND research originated in Sydney. The most accessible information was from Dementia Australia, with some inaccuracies noted. There is scant Australian research/information on HAND screening/diagnosis. HAND translational research and screening/diagnosis standards are urgently needed to inform best practices. The Australian context is used to discuss international implications regarding higher-income countries with similar patterns/healthcare.
HIV-associated neurocognitive disorder (HAND) is an umbrella term regrouping mild to severe forms of neurocognitive complications in people living with HIV(PLHIV). In treated PLHIV, HIV-associated dementia is rare but mild forms of neurocognitive impairment can reach up to 40% depending on their previous HIV history, age, and comorbidities. Mild forms of HAND are characterised by mild to moderately impaired cognitive functions, especially for new learning, complex attention, executive functions, and processing speed. Sometimes mental health changes are characterized by apathy and social withdrawal (https://pubmed.ncbi.nlm.nih.gov/34081306). HAND can be diagnosed with (symptomatic) and without (asymptomatic) decline in independence in activities of daily living (Antinori et al., Citation2007; Obermeit et al., Citation2017). Worldwide, it is estimated that 42.6% of PLHIV have HAND (Wang et al., Citation2020). However, the prevalence is lower in virally suppressed PLHIV (∼30%). Further, it is increasingly clear that non-HIV causes of cognitive impairment are a significant component of the condition (Heaton et al., Citation2023) making the diagnostic process complex. There is no cure for HAND (Bougea et al., Citation2019), however, if diagnosed early, optimized antiretroviral therapy (Sacktor et al., Citation2016), exercise (Mapstone et al., Citation2013), and socio-psychological interventions targeting depression and coping (Tedaldi et al., Citation2015) can assist in avoiding rapid cognitive decline and maintain a maximum of independence in activities of daily living.
Early HAND diagnosis requires an awareness of signs and symptoms and knowledge of assessment services. In Australia, approximately 75% of PLHIV are aware of HAND however are hesitant to discuss HAND as they are fearful of their future (Cummins et al., Citation2018). Thus, it is important that PLHIV and those who support them receive consistent, stigma-free, accurate, and timely information about HAND, diagnostic pathways, and treatment from health professionals (Cummins et al., Citation2018). This is becoming increasingly important as aging is associated with an increased likelihood of HAND (Aung et al., Citation2023) and the HIV population is rapidly aging (The Kirby Institute, Citation2023). In addition, with successful viral suppression being common in Australian people living with HIV who are treated, conditions that impact on quality of life such as HAND are receiving greater attention (The Kirby Institute, Citation2023).
A HAND diagnosis may occur with and without a screening phase. The diagnosis phase is time-intensive, involves multiple specialists and exams, and is therefore relatively costly. A screening phase may assist in streamlining the diagnosis phase (Bloch et al., Citation2016) by initiating a referral to a neurologist for a more complex assessment. The streamlining of care for patients who are more in need of a neurology review is cost-effective. However, screening is not routinely available. Valid and reliable HAND screening tools are in development (Parry et al., Citation2017) so that trained support workers, nurses, and neuropsychology trainees may administer screening tests. Factors considered in selecting appropriate screening tools include the education level of PLHIV (Musso et al., Citation2018), the skill set of the tool administrators and interpreters (Kwasa et al., Citation2012), tool administration time, cost (Kamminga, Lal, et al., Citation2017), and psychometric properties (Kamminga, Bloch, et al., Citation2017). Therefore, screening tools and diagnostic pathways may vary within and between countries.
A HAND diagnosis involves a comprehensive neuropsychological assessment which is the current gold standard for the assessment of cognitive impairment to determine a HAND diagnosis, (Antinori et al., Citation2007; Underwood & Winston, Citation2016). Neuropsychologists are responsible for administering and interpreting the comprehensive neuropsychological assessment which includes assessments of cognitive, mental health and function. Neurologists are in charge of the final diagnosis. They will frequently also request an MRI, blood tests, and sometimes a lumbar puncture for a CSF exam and request a psychiatric evaluation. HIV specialists, primary physicians, and/or the neurologist also complete a medical history. A HAND diagnosis therefore represents a complex process requiring multi-disciplinary expertise, in addition to careful coordination and clear pathways to determine when tests are conducted, who conducts and interprets the tests, and who interprets all the results for the final diagnosis. In Australia, only a neurologist can diagnose HAND. Importantly, HAND is a diagnosis of exclusion, and HIV is required to be the cause (at least in part) for the cognitive and function changes for a HAND diagnosis.
The Australian National Strategy for the Diagnosis and Treatment of HIV highlights the need for clear and equitable protocols for coordinated access to diagnosis, care, and support (Australian Government Department of Health, Citation2018). Since HAND is a possible complication of HIV (Wang et al., Citation2020) it is reasonable to expect national uniformity regarding HAND diagnosis and access to care and support. However, HIV policy is under the jurisdiction of each state and the uniformity of diagnostic pathways and information surrounding care and support access is largely unknown. A starting point towards uniformity is mapping existing literature and resources to identify current state-based diagnostic practices and information sources available to healthcare professionals, PLHIV, and the carers/support people. Further, there is a large push internationally to move towards consensus recommendations surrounding screening, diagnosis, and treatment of HAND (Nightingale et al., Citation2023); with recent commentaries documenting unique challenges and complexities associated with HAND – in particular due to comorbidities with HIV, lack of health literacy and felt dismissal among PLHIV, lack of training among health professionals and inadequate health services (Cysique et al., Citation2024; Nightingale et al., Citation2024). However, much of the recent international focus is centred around higher-income Western countries.
Thus, this study reports a scoping review that systematically examined academic and grey literature on HAND screening and diagnosis to determine the type and quality of information available in Australia, which can also add valuable information to contemporary international conversations in this space. The synthesis of the results may inform HAND diagnostic pathway policy, identify where the quality of information could be improved, identify barriers to seeking HAND diagnosis, and guide future clinical research directions – both within Australia and potentially globally.
Review questions
The core aim of this scoping review was to determine current Australian HAND diagnostic guidelines and related information regarding HAND. The review questions (RQ) to be answered were:
RQ(a) Does each state and territory have a Health Department policy for HAND diagnosis?
RQ(b) Is there Australian academic research on HAND diagnosis? What is it recommended? Which state is it from?
RQ(c) Does Australian academic literature report specific HAND screening and diagnostic tools? Are the tools appropriate for all Australians including Australian Aboriginal and Torres Strait Islander peoples, and Australians with diverse cultural and linguistic backgrounds, sexual orientation, and/or gender?
RQ(d) What HAND screening and diagnosis information is available, who does it target, and who provides it?
RQ(e) Who are PLHIV referred to when concerned about their HAND status?
Materials and methods
The scoping review protocol development followed the Joanna Briggs Institute methodology for scoping reviews (Peters et al., Citation2015, Citation2020). The results report followed the PRISMA-ScR guidelines (Tricco et al., Citation2018). The protocol was developed and refined by the research team, key stakeholders, PLHIV, and a university health research librarian.
Inclusion criteria
Inclusion criteria were based on the Joanna Briggs Institute guidelines of participants, concept, and context (Peters et al., Citation2015).
Participants
The target population was PLHIV being screened for or diagnosed with HAND.
Concept
The central concepts were the screening and HAND diagnosis. Screening for cognitive change includes cognitive testing, and psychosocial and medical history (Ian et al., Citation2016). Diagnosis is defined as the neuropsychological assessment and neuromedical examination to exclude diseases and medical conditions that entail cognitive, brain, and functional change.
Context
This review searched for evidence of current Australian HAND screening and diagnostic pathways available to clinicians and all Australians. Current means academic papers published between January 2015 and July 2021, and grey literature accessible to all Australians on the internet regardless of publication date.
Search
An EBSCOhost Megafile Ultimate, Medline, domains gov.au and org.au, and the Google search occurred from 1 to 3 July 2021 and 16 December 2022.
A preliminary search of Google and EBSCOhost Megafile, and consultation with a university health research librarian and team members RW, AM (expertise in HIV/sexual health), SG, HG, and AP (expertise in HAND) determined the strings used in the database searches with input from PLHIV. The strings were (“HIV associated neurocognitive disorder” OR “HIV associated Dementia” OR “AIDS Dementia Complex”) AND (screening OR assessment OR test OR diagnosis OR tools OR refer* OR “referral process” OR “referral pathway” OR “care pathway”) and limited to 2015–2021.
Two Australian internet domains were searched using advanced Google search:.gov.au and.org.au. The.gov.au domain encompasses all government departments including the governments of New South Wales, (NSW), Queensland, Victoria, Tasmania, South Australia, Western Australia (WA), the Australian Capital Territory, and the Northern Territory. The.org.au domain encompasses all Australian registered not-for-profit organisations including support organisations for PLHIV and people with dementia.
There were two separate searches each for gov.au and org.au. The first search for each domain was: All these words “policy”, and all the terms “HIV associated neurocognitive disorder”. The second search was: All the words “report”, and all the terms “HIV associated neurocognitive disorder”. A general Google search using the terms HIV-associated neurocognitive disorder Australia was also completed. One researcher who appeared several times in academic literature was contacted seeking unpublished papers. Four papers were suggested: three were already reviewed and excluded, and the remaining paper (Cysique et al., Citation2012) was published before 2015 and was excluded.
Screening procedure
The screening procedures were reviewed by team members, AM and KD. The initial scoping literature searches were conducted on 1–3 July 2021 and the second in December 2022. The two literature searches were conducted to determine if there was an increase in the number of publications about HAND diagnosis in Australia. In 2021, the papers were imported into Endnote X9.3.3 referencing software (https://endnote.com). In 2022, the papers were imported into a separate folder in Endnote (Endnote 20.4.1) and although the screening procedure of 2021 was replicated in 2022, the 2021 folder was not opened until screening was completed, to minimise the risk of bias.
Database screening
As seen in and , the first step in the database search was to remove the duplicate records. In 2021, 865 papers were identified and 73 were duplicates, leaving 792 papers to screen (). In 2022, 1273 papers were identified and 338 were duplicates, leaving 936 papers to screen ().
Figure 1. PRISMA scoping review chart for the stages of screening for searches conducted on 1–3 July 2021.
Note: Records Screened = This was the first stage of screening and used exclusion criteria; Reports sought for retrieval: This was the second stage of screening, and the abstract was read for inclusion and exclusion criteria; Reports assessed for eligibility: this was the third stage of screening in which full text was read to determine if the paper was filled all the inclusion criteria. Database reports were excluded if (a) Reason 1 = Not Australian research; (b) Reason 2 = Australian research but did not satisfy all inclusion criteria; (c) Reason 3 = Full text not available. Google reports were excluded if (d) Reason 1 = did not include HAND diagnosis or testing; (e) full text was not available, (f) duplication academic database search. is based on Haddaway et al. (Citation2021).
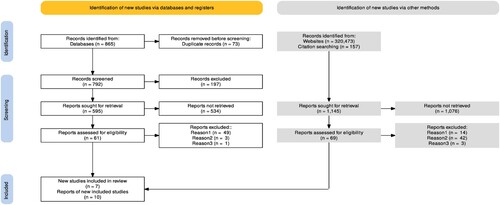
Figure 2. PRISMA scoping review chart for the stages of screening for searches conducted on 16 December 2022.
Note: Records Screened = This was the first stage of screening and used exclusion criteria; Reports sought for retrieval: This was the second stage of screening, and the abstract was read for inclusion and exclusion criteria; Reports assessed for eligibility: this was the third stage of screening in which full text was read to determine if the paper was filled all the inclusion criteria. Reports were excluded if (a) Reason 1 = Not Australian research; (b) Reason 2 = Australian research but did not satisfy all inclusion criteria; (c) Reason 3 = Full text not available. is based on Haddaway et al. (Citation2021).
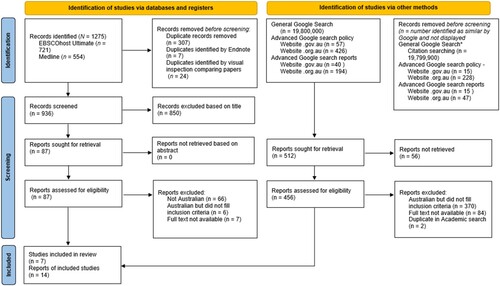
Next, the titles of all the remaining papers were screened for exclusion. These included the words risk, prevalence, treatments (e.g., mindfulness, medication), gene, telomere, references to brain and nerve biology, monitoring, and validation in countries other than Australia were excluded. In 2021, 197 of 865 papers were excluded because their titles included exclusion criteria leaving 595 for possible retrieval (). In 2022, 850 of 936 papers were excluded because their titles included exclusion criteria, leaving 87 for possible retrieval ().
In the third step, the abstracts in the remaining reports were read to determine if the reports included information on HAND screening, testing, or diagnosis. If HAND screening or diagnostic protocols were unclear, the materials section was searched for evidence. In 2021, 534 of 595 remaining papers did not include inclusion criteria and were not retrieved for further screening (). In 2022, none of the 87 papers were excluded as they included inclusion criteria ().
In the final step, the full text was to be read to determine if it was about HAND diagnosis or testing in Australia so it could be included in the review. In 2021, the full text of one paper could not be retrieved, 49 of the 61 papers were not Australian, and 2 of the 61 did not include information about HAND diagnosis or testing in Australia, leaving 7 papers about HAND diagnosis or testing in Australia (). In 2022, the full text of seven papers could not be retrieved, 66 of the 87 papers were not Australian, and 6 of the 87 did not include information about HAND diagnosis or testing in Australia, leaving 7 papers about HAND diagnosis or testing in Australia ().
Google search
In the domain.gov.au policy,.gov.au report,.org.au policy, and.org.au report searches, the first 30 hits of each search were screened as the subsequent hits did not meet inclusion criteria. In a basic Google search, the first 70 hits were screened to reduce the risk of missing items for review. Reports were excluded if they did not include HAND diagnosis. In 2021, 1076 out 1145 reports that did not have information about diagnosing or screening were excluded leaving 69 reports (). In 2022, 56 out of 512 reports that did not have information about diagnosing or screening were excluded leaving 456 reports ().
In the next stage, the reports were read to determine if their legibility was to be included in the review. In 2021, of the 69 reports read, 14 did not include information on HAND diagnosis or testing, 42 and 3 were duplicates of papers in the academic database search, resulting in 10 non-academic reports to be reviewed (). In 2022, of the 456 reports that were read in full to assess eligibility, 370 did not include information on HAND diagnosis or testing, the full text of 84 reports was not available, and 2 were duplicates of academic research that were already included in the review, leaving 14 non-academic reports to review ().
In summary, there were more academic papers, and advanced and basic Google search hits in 2022 compared to 2021. However, the searches identified the same seven academic papers for review and 10 reports. A key development was that in 2022, an additional 4 non-academic reports were identified. The additional reports were published after the 2021 review.
Results
The first scoping review in 2021 identified 17 articles which were categorised as academic articles, not-for-profit articles, or education resources. The follow-up scoping literature search in 2022 found an additional four not-for-profit organisation whose web sites referred to HAND diagnosis. The items were from the Australasian Society for HIV, Viral Hepatitis, and Sexual Health Medicine (ASHM, Citation2022), Queensland Positive People (Citation2022), Neuropsychologist (Citationn.d.), and Turning Point (Manning et al., Citation2021).
Intended audience
Academic papers focused on assessment and screening, targeting university-trained health professionals who diagnose HAND (Bloch et al., Citation2016; Cummins et al., Citation2017, Citation2018, Citation2019; Herrmann et al., Citation2019; Ian et al., Citation2016; Kamminga, Bloch, et al., Citation2017; Kamminga, Lal, et al., Citation2017; Underwood & Winston, Citation2016). The papers reviewed previous research, ASHM teaching web site, and HAND symptomatology and monitoring (Cummins et al., Citation2019).
The not-for-profit organisation publications had different target populations. Brew et al. (Citation2016a) targeted only PLHIV. Brew et al. (Citation2016b) and Dementia Australia (Citation2014a, Citationn.d.), a peak body for dementia research, education, and support in Australia published booklets targeted partners, family, friends, and carers of PLHIV Brew et al. (Citation2016b). and targeted community care workers (Dementia Australia, Citation2014b). The booklets described HAND, signs and symptoms, screening, diagnosis, treatment, and practical support for PLHIV. A key difference between Brew et al. and Dementia Australia is that Brew et al. (Citation2016a, Citation2016b) emphasised that symptoms can be normal and early treatment is key to living a normal life, however, this was not included in Dementia Australia publications. In contrast, Neuropsychology (Citationn.d.), Queensland Positive People (Citation2022), and ASHM (Citation2022), appeared to target the general population and PLHIV by clearly describing standards and policies for psychological support people PLHIV. Turning Point (Manning et al., Citation2021), a research and support organisation for alcohol and other drugs of addiction, targeted health professionals. Two blogs targeted PLHIV and encouraged early diagnosis (Crawford, Citation2016, Citation2017).
Academic articles
Of seven academic papers, six were Australian, with one from the Asia-Pacific region. Five papers collected data in Sydney, the capital city of New South Wales (Bloch et al., Citation2016; Cummins et al., Citation2017, Citation2019; Kamminga, Bloch, et al., Citation2017; Murray et al., Citation2016; Underwood & Winston, Citation2016) and one collected data in Perth, the capital city of Western Australia (Herrmann et al., Citation2019).
Three papers were reviewed. Two made recommendations for clinical guidelines for HAND diagnosis in the Asia-Pacific region (Ian et al., Citation2016), and New South Wales (Cummins et al., Citation2018), and the third was a critical review of the effects of repeated screening on test results among PLHIV (Kamminga, Lal, et al., Citation2017). Four papers validated screening instruments in the Australian context (Bloch et al., Citation2016; Cummins et al., Citation2017; Herrmann et al., Citation2019; Kamming, Lal, et al., Citation2017). Two papers included flowcharts for diagnosis, although the details differed between the flowcharts (Cummins et al., Citation2019; Ian et al., Citation2016).
Two papers suggested that home-based assessments may be key to early detection of cognitive change in PLHIV. Murray et al. (Citation2016) found that informal caregivers were more likely to report changes in cognition than PLHIV and therefore play an important role in early detection of HAND. Cummins et al. (Citation2019) recommended initial home-based assessments by multidisciplinary staff, annual HAND risk assessment, and referral to occupational therapists or nurses for ongoing monitoring, particularly as HAND symptoms emerge (and then to a medical doctor and/or a neuropsychologist; Ian et al. (Citation2016)) recommended HAND screening commence when depressive symptoms are detected in a routine administration of the Hospital Anxiety Depression Scale (Zigmond & Snaith, Citation1983) and then referral to a neuropsychologist for neuropsychological testing at the emergence of HAND symptoms. However, service provision also needs to be considered within the context of health services and health economics – which is beyond the scope of the current scoping review.
The academic papers stated that the “gold standard” was neurocognitive testing conducted by neuropsychologists (). Bloch et al. (Citation2016) stated staff were trained to conduct a medical history and trained by a neuropsychologist to administer the CogState Screen (Cysique et al., Citation2006). Ian et al. (Citation2016) reported neuropsychologists interpret the tests, and Kamminga, Lal, et al. (Citation2017) indicated neuropsychologists administer, score, and interpret tests.
Table 2. Nursing assessment questions for caregivers of people with HIV as suggested by ASHM (Cummins, Citation2019).
Training resources
The Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM) Queensland Sexual Health Research Fund (SHRF) HAND information was part of an online learning HIV course for Australian and New Zealand nurses written by clinical nurse consultants, nurse practitioners, and managers (Cummins et al., Citation2019). They recommended that the Montreal Cognitive Assessment (MoCA; Cummins, Citation2019) International HIV Dementia Scale (Nasreddine et al., Citation2005) and CogState Battery (Cysique et al., Citation2006) be used by trained personnel to monitor cognitive change, and specialist neuropsychologists conducted neuropsychological testing. They encouraged nurses to ask PLHIV and support persons about changes in activities of daily living, forgetfulness, personality, and organisational ability of the PLHIV. lists the questions included.
Table 1. Nursing assessment questions for people with HIV as suggested by ASHM (Cummins, Citation2019).
Not-for-profit organisation articles
The 14 not-for-profit articles represented organisations supporting PLHIV: New South Wales Health’s Adaphs program (previously known as the AIDS Dementia and HIV Psychiatry Service), Positive Life, Queensland Positive People (QPP), the Australian Federation of AIDS Organisations (AFAO), and the National Association of People with HIV Australia (NAPHA); and Dementia Australia. Six articles were booklets developed as joint projects between Australian not-for-profit organisations supporting PLHIV such as AFAO, Positive Life, NAPHA, and ASHM (Australian Federation of AIDS Organisations, Citation2015; Brew et al., Citation2016a, Citation2016b; Dementia Australia, Citation2014a, Citation2014b). The booklets briefly describe HAND and list support organisations. Information regarding HAND screening and diagnosis was fairly consistent across the booklets. Two articles were blogs on HAND diagnosis, and one was a link to a description of the stages of diagnosis (Crawford, Citation2016, Citation2017). The dates of publication were 2014–2020.
Six not-for-profit articles encouraged early assessment. Four articles provided brief descriptions of testing; for example, medical history, medical examination, blood tests, brain scan, possibly a lumbar puncture and interviews by a neuropsychologist (Dementia Australia, Citationn.d.). The NSW Health site and Turning Point provided an outline of what the neurocognitive tests measure (Australian Federation of AIDS Organisations, Citation2015; Manning et al., Citation2021). The Australian Federation of AIDS Organisations (Citation2015) mentioned the final stage of diagnosis was a written report and discussion of the assessment findings. The articles included a list of supportive not-for-profit groups or health professionals. The Neuropsychologists web page had links to a variety of support services, including Dementia Australia and Alzheimer Australia, but not HIV support services. QPP recommended people with concerns about their cognitive state and functioning to contact them or their local doctor (QPP, Citation2022). Instead of providing a general overview of diagnostic procedures, ASHM (Citation2022) developed a comprehensive policy statement detailing the frequency of cognitive screening, indicators for additional screening, and referral for comprehensive cognitive assessment by suitably qualified people without specifying the qualifications and training in advanced neuropsychological assessment.
Discussion
The scoping review aim was to identify policy guidelines and information relating to HAND screening and diagnosis. Most of the literature differentiated between screening and diagnosis, stating diagnosis requires neuropsychological testing by a neuropsychologist. In academic papers, there were inconsistencies regarding the most appropriate person to administer the screening tools. Jargon and detailed information were avoided when targeting the general population, however, it was included when targeting support workers.
RQ(a)
There was no evidence of state-based or national health policies for HAND diagnosis and referral pathways. However, New South Wales Health has a link to its Adaphs program, and Positive Life refers people to the NSW’s ACON program.
RQ(b)
Community members participated in developing HAND diagnostic guidelines at a state and international level, and NSW HIV specialists screening tools and referral pathways (Cummins et al., Citation2017). Additionally, an international HIV medical specialist organisation developed a comprehensive psychological support policy that includes a repeated cognitive assessment of HIV diagnoses (ASHM, Citation2022), and Australian Neuropsychologists recommend people with HIV receive neurocognitive testing within a few weeks of cognitive change (Neuropsychology, Citationn.d.). Cummins et al. (Citation2017) suggested professional caregivers administer screening tools. However, support from professional caregivers can typically only occur when PLHIV experiences sufficient disability to qualify for professional caregiver support and therefore early HAND diagnostic opportunities may be missed. In contrast, Ian et al. (Citation2016) argued that pre-screening for depressive symptoms may be more effective in capturing asymptomatic cognitive change. Thus, if pre-screening could be incorporated into primary care physician’s annual chronic disease management plans and results forwarded to HIV specialists for assessment, and to neurologists for ongoing monitoring, HAND may be more likely to be diagnosed early when present.
The nursing guidelines for HAND screening in the ASHM training (Cummins et al., Citation2019) within Australasia were consistent with those suggested by Ian et al. (Citation2016). These guidelines can be accessed by any nurses interested in updating their HAND knowledge. However, there was no mention of specialist training for screening tool administration, scoring and interpretation nor when to refer for diagnosis. ASHM recommended nurses also ask PLHIV and their support person about changes in function (see ), however, there was no evidence that the questions were a validated or reliable HAND screening tool. Research could determine the usefulness of the questions and what responses would trigger a referral for diagnosis.
Despite the reported importance of screening, screening is not necessary for HAND diagnosis. Pre-screening and screening could be included in diagnostic guidelines to streamline people into more advanced assessments to avoid late diagnosis. Thus, there is a need to establish a central online resource to provide authoritative information (Antinori et al., Citation2007). Despite the reported importance of psychological interventions and neuropsychological testing, there was no guidance for referral to psychologists identified.
RQ(c)
There is limited research on screening tools. Herrmann et al. (Citation2019), in WA, reported the MoCA has sufficient sensitivity to detect asymptomatic cognitive impairment in PLHIV. The Cogstate research tool is being tested as a clinical assessment tool in a Sydney clinic (Underwood & Winston, Citation2016). A review of the limitations of repeated testing (Kamminga, Lal, et al., Citation2017) recommended that tools only be used according to validated protocols and interpreted using normed values. The diagnostic tools reported included medical history, tests for liver function, and infections are in line with recommendations (Antinori et al., Citation2007; Cysique et al., Citation2012; Cysique & Brew, Citation2009).
It is unknown if HAND screening is suitable for all Australian PLHIV as the research is limited to Sydney and Perth. The limited research locations also suggest rural and regional Australia, Australian Aboriginal and Torres Straight Islanders, and Culturally and Linguistically Diverse People in Australia are under-represented, and the research may not sufficiently generalize to these groups. The research was primarily conducted by neuropsychologists, suggesting the views of other Australian health professionals and key stakeholders may be under-represented or excluded including clinical psychologists trained in neuropsychological testing.
RQ(d)
The web-based information is mainly consistent across resources but inaccurate, perhaps because the booklets published between 2014 and 2016 are outdated. The preliminary search results for HIV and memory loss on Google were predominately USA-based HIV dementia sites where much information was inaccurate. For example, contrary to Australian booklets, screening is not necessary for diagnosis (Antinori et al., Citation2007; Cysique & Brew, Citation2009; Kinai et al., Citation2017).
Several documents did not have publication or copyright dates on downloadable documents (ASHM, Citation2022; Dementia Australia, Citationn.d.; Manning et al., Citation2021) or websites (Neuropsychology, Citationn.d.). This makes it difficult to determine up-to-date literature. It is recommended that documents have easily identified publication or copyright dates to allow consumers and researcher to identify the documents which are the most recent. This may help disseminating up-to-date and, perhaps, accurate diagnostic information.
The additional discovery of new websites in 2022 is an indication that some not-for-profit organisations are beginning to promote HAND diagnoses (Manning et al., Citation2021, Queensland Positive People [QPP], Citation2022) However, the number of government reports was unchanged. Thus, there appears to be a growth in the number of non-for-profit organisations promoting HAND but there remains a lack of policy at the government level.
Including Australia in the Google search terms may be a barrier to seeking help as the first search results were Dementia Australia, which could seem irrelevant if the relationship between HAND and dementia is not well understood. The stigma and prognosis of dementia in addition to HIV-related stigma may also deter early screening and diagnosis. These possibilities warrant further investigation, particularly since 25% of PLHIV are unaware of HAND and most of those who know about HAND are concerned about their future (Cummins et al., Citation2018). Inaccurate information, potential barriers, and difficulty finding accurate Australian HAND information could be addressed by developing Australia-specific current and accurate online information. There is a clear need for easily located accurate online information.
RQ(e)
Readers of booklets and blogs were referred to their doctor or to not-for-profit organisations which support PLHIV. However, one organisation, Turning Point, recommended neurological assessment by neuropsychologists for any cognitive and functional changes including HAND (Manning et al., Citation2021). There was no recommendation to seek psychological intervention for depression or to develop coping strategies. These findings suggest these interventions for HAND may be overlooked and undervalued and may represent an important area for future health promotion research.
The mapping of HAND screening and diagnosis revealed a paucity of information for Australian health workers and the general population. NSW and WA are the only states who have published research and NSW is the only state to have developed diagnostic guidelines. Information on HAND screening and diagnosis for clinicians of all disciplines is very limited and it is difficult for the general population and PLHIV to find reliable information.
International implications
Our review demonstrates that while research about HAND screening and diagnosis exists in Australia, it is limited geographically with repercussions on where best care for HAND is available in the country. Because of this, this research has concentrated on a restricted demographic of people living with HIV infection in Australia. Efforts are underway to address this issue and the development of tools that are cross-culturally valid to assess HAND in Australia (Gates et al., Citation2021; Thompson et al., Citation2020).
Furthermore, research on HAND in Australia has not been widely translated into guidelines that can be used by frontline HIV healthcare professionals and the community (although this is being partly addressed by this project and review which has also developed resources for healthcare professionals and the community). The dissociation between academic research and translation to practice is not unique to Australia. Several reasons are in cause. There has been a chronic lack of research funding for HIV clinical research relative to other areas of HIV research (particularly severe in Australia since the country has reached the 90.90.90 WHO HIV treatment strategy. In addition, Australia has no dedicated HIV funding apart from surveillance and is amongst OECD countries with one of the lowest percentage research GDP contributions, that is 0.49%; Research Professional News, Citation2023). On par with the international context in High Income countries, the public health message has been on maintaining viral suppression, delivering PrEP as widely as possible, and continuing to mainly fund vaccine and cure research. While these are laudable aims and very important research, they should not come at the expense of clinical research and associated translation for the people who are living with HIV now and HAND in particular.
As noted in the introduction, the community and some care professionals and researchers (with limited resources as in the current project) have nonetheless continued to talk and research about HAND and its impact on quality of life as well as the added risk of cognitive decline in late life. Another reason is that the current international diagnostic criteria for HAND focus on the neuropsychological assessment for HAND but provide limited information on the other clinical investigations (Nightingale et al., Citation2023). The clinical investigations are only provided in specialized textbooks which are dissociated from the criteria and have not been widely translated to clinical care with a few exceptions. An effort from the global NeuroHIV community is needed to better translate this information so that it reaches healthcare professionals and the community.
However, funding organizations and governments will need to support such an effort and in the current funding context both in Australia and internationally, this is uncertain. Indeed, clinical researchers are leaving this area because this is not a sustainable research career anymore (LAC personal communication). This paper therefore serves, as another call, for a careful update of the international HAND diagnostic criteria with the inclusion of guidelines for screenings, diagnosis, and prognosis encompassing all the required investigations for a HAND diagnosis (Cysique et al., Citation2024). Such guidelines should be updated with prevention, early detection, and early management as well as interventions in mind, similar to other neurological conditions (e.g., Alzheimer’s disease, Vascular Cognitive Impairment). An update of the criteria would also need to include tools and guidelines for the Low-Middle Income Countries and the diverse people who are living with HIV in High Income countries including Australia. An international update would also facilitate translation efforts at the national level.
Limitations
Clinical chart searches for referral pathways were not conducted, and not-for-profit support groups were not asked to identify HAND information given to clients, nor policy guidelines on screening, diagnosis, or referrals. Additionally, this review has not conducted a critical analysis of the screening or diagnostic tools, since the purpose is to discover the tools currently being used or recommended. Future research is needed in these areas. Findings from the current review have relevance to international considerations and guidelines (particularly High-Income countries); however may not be appropriate for generalization to Low-Middle Income Countries and warrant an important focus for further research. This review does not focus on costs and financial viability (including staff training and resources), and thus it is recommended that future research consider further, and more comprehensive considerations related to health economics and health service optimization.
In conclusion, this review mapped the current academic and online information about the state of HAND screening and diagnosis in Australia. HAND can be managed with pharmaceutical and psychosocial interventions especially if diagnosed early, however, gaps in knowledge exist and information that is directed towards healthcare professionals and the community is scant. With coordinated national HAND research, resources, and policy guidelines, PLHIV and key stakeholders would be more assured that early cognitive change is identified and assessed promptly, so psychological and medical interventions are timely and declines in cognition and function are ameliorated.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Antinori, A., Arendt, G., Becker, J. T., Brew, B. J., Byrd, D. A., Cherner, M., Clifford, D. B., Cinque, P., Epstein, L. G., Goodkin, K., Gisslen, M., Grant, I., Heaton, R. K., Joseph, J., Marder, K., Marra, C. M., McArthur, J. C., Nunn, M., Price, R. W., Pulliam, L., … Wojna, V. E. (2007). Updated research nosology for HIV-associated neurocognitive disorders. Neurology, 69(18), 1789–1799. https://doi.org/10.1212/01.WNL.0000287431.88658.8b
- Aung, H. L., Siefried, K. J., Gates, T. M., Brew, B. J., Mao, L., Carr, A., & Cysique, L. A. (2023). Meaningful cognitive decline is uncommon in virally suppressed HIV, but sustained impairment, subtle decline and abnormal cognitive aging are not. eClinicalMedicine, 56, 101792. https://doi.org/10.1016/j.eclinm.2022.101792
- Australasian Society for HIV, Viral Hepatitis, and Sexual Health Medicine. (2022). Standards for Psychological Support for Adults with HIV. Retrieved December 16, 2022, from https://www.ashm.org.au/resources/australian-standards-for-psychological-support-for-adults-with-hiv/
- Australian Federation of AIDS Organisations; National Association of People with HIV Australia. (2015). Living well: Women with HIV: Information about some of the key issues for women with HIV. https://tinyurl.com/4hfteet7
- Australian Government Department of Health. (2018). Eighth National HIV Strategy. https://tinyurl.com/4pnwtdb2
- Bloch, M., Kamminga, J., Jayewardene, A., Bailey, M., Carberry, A., Vincent, T., Quan, D., Maruff, P., Brew, B., & Cysique, L. A. (2016). A screening strategy for HIV-associated neurocognitive disorders that accurately identifies patients requiring neurological review. Clinical Infectious Diseases, 63(5), 687–693. https://doi.org/10.1093/cid/ciw399
- Bougea, A., Spantideas, N., Galanis, P., Gkekas, G., & Thomaides, T. (2019). Optimal treatment of HIV-associated neurocognitive disorders: Myths and reality. A critical review. Therapeutic Advances in Infectious Disease, 6. https://doi.org/10.1177/2049936119838228
- Brew, B., Cummins, D., & Crawford, D. (2016a). HIV associated neurocognitive disorder. Positive Life NSW. https://tinyurl.com/389vbc9a
- Brew, B., Cummins, D., & Crawford, D. (2016b). HIV associated neurocognitive disorder. Positive Life NSW. Partners, Family, friends and carers of people with HIV associated neurocognitive disorder. Positive Life NSW. https://tinyurl.com/23at3z3z
- Crawford, D. (2016, December 18). Lets talk about hand. Blog. https://www.positivelife.org.au/blog/talk-about-hand/
- Crawford, D. (2017, March 14). The good news about HAND. Blog. https://www.positivelife.org.au/blog/good-news-about-hand/
- Cummins, D. (2019). HIV-associated neurocognitive disorder. https://hivmanagement.ashm.org.au/hiv-associated-neurocognitive-disorder/
- Cummins, D., Murray, K., Trotter, G., Batterham, M., Healey, L. & O’Connor, C. (2017), Can patients and their caregivers boost identification of HIV Associated Neurocognitive Disorder (HAND)? Australian Journal of Advanced Nursing, 34(3), 24–33. https://www.ajan.com.au
- Cummins, D., Waters, D., Aggar, C., & O'Connor, C. C. (2018). Potential impacts of poor communication on early diagnosis of HIV-associated neurocognitive disorder. Journal of Advanced Nursing, 74(6), 1342–1348. https://doi.org/10.1111/jan.13533
- Cummins, D., Waters, D., Aggar, C., & O’Connor, C. C. (2019). Assessing risk of HIV-associated neurocognitive disorder. Nursing Research, 68(1), 22–28. https://doi.org/10.1097/NNR.0000000000000312
- Cysique, L., Bain, M. P., Lane, T. A., & Brew, B. (2012). Management issues in HIV-associated neurocognitive disorders. Neurobehavioral HIV Medicine, 4, 63–73. https://doi.org/10.2147/NBHIV.S30466
- Cysique, L. A., & Brew, B. J. (2009). The assessment of HIV-associated neurocognitive disorders: New challenges in the HAART era. In R. P. Sacktor, V. Valcour, & K. Tashima (Eds.), HIV and the brain: New challenges in the modern era (1st ed., pp. 109–132). Humana Press Inc. https://doi.org/10.1007/978-1-59745-434-6_7
- Cysique, L. A., Brew, B. J., Bruning, J., Byrd, D., Costello, J., Daken, K., Ellis, R. J., Fazeli, P. L., Goodkin, K., Gouse, H., Heaton, R. K., Letendre, S., Levin, J., Aung, H. L., Mindt, M. R., Moore, D., Mullens, A. B., de Almeida, S. M., Muñoz–Moreno, J. A., … Rourke, S. B. (2024). Cognitive criteria in HIV: Greater consensus is needed. Nature Reviews Neurology, 20(2), 127–128.
- Cysique, L. A., Maruff, P., Darby, D., & Brew, B. J. (2006). The assessment of cognitive function in advanced HIV-1 infection and AIDS dementia complex using a new computerised cognitive test battery. Archives of Clinical Neuropsychology, 21(2), 185–194. https://doi.org/10.1016/j.acn.2005.07.011
- Dementia Australia. (2014a). Living with HIV-associated neurocognitive disorders (HAND): Information for people living with HIV and HAND, their partners, Families, and friends. https://www.dementia.org.au/sites/default/files/HAND-booklet-for-consumers.pdf
- Dementia Australia. (2014b). HIV-associated neurocognitive disorders (HAND): A toolkit for community care workers. https://tinyurl.com/5n8ac296
- Dementia Australia. (n.d.). HIV associated dementia. From About dementia Series no 19. https://tinyurl.com/4kzwmvav
- Gates, T. M., Kamminga, J., Jayewardene, A., Vincent, T., Quan, D., Brew, B. J., Bloch, M., & Cysique, L. A. (2021). An examination of reliable change methods for measuring cognitive change with the Cogstate Computerized Battery: Research and clinical implications. Archives of Clinical Neuropsychology, 36(4), 597–612. https://doi.org/10.1093/arclin/acaa076
- Haddaway, N. R., Pritchard, C. C., & McGuinness, L. A. (2021). PRISMA2020: R package and ShinyApp for producing PRISMA 2020 compliant flow diagrams (Version 0.0.2). Zendodo. https://doi.org/10.5281/zenodo.4287834
- Heaton, R. K., Ellis, R. J., Tang, B., Marra, C. M., Rubin, L. H., Clifford, D. B., McCutchan, J. A., Gelman, B. B., Morgello, S., Franklin, D. R., & Letendre, S. L. (2023). Twelve-year neurocognitive decline in HIV is associated with comorbidities, not age: A CHARTER study. Brain, 146(3), 1121–1131. https://doi.org/10.1093/brain/awac465
- Herrmann, S., McKinnon, E., Skinner, M., Duracinsky, M., Chaney, R., Locke, V., & Mastaglia, F. (2019). Screening for HIV-Associated neurocognitive impairment: Relevance of psychological factors and era of commencement of antiretroviral therapy. Journal of the Association of Nurses in AIDS Care, 30(1), 42–50. https://doi.org/10.1097/JNC.0000000000000040
- Ian, E., Gwen, C. L., Soo, C. T., Melissa, C., Chun-Kai, H., Eosu, K., Hyo-Youl, K., Asad, K., Scott, L., Chung-Ki, L. P., Anekthananon, T., Jordan, T. G., Han-Ting, W., & Wing-Wai, W. (2016). The burden of HIV-associated neurocognitive disorder (HAND) in the Asia-Pacific region and recommendations for screening. Asian Journal of Psychiatry, 22, 182–189. https://doi.org/10.1016/j.ajp.2015.10.009
- Kamminga, J., Bloch, M., Vincent, T., Carberry, A., Brew, B. J., & Cysique, L. A. (2017). Determining optimal impairment rating methodology for a new HIV-associated neurocognitive disorder screening procedure. Journal of Clinical and Experimental Neuropsychology, 39(8), 753–767. https://doi.org/10.1080/13803395.2016.1263282
- Kamminga, J., Lal, L., Wright, E., Bloch, M., Brew, B., & Cysique, L. (2017). Monitoring HIV-associated neurocognitive disorder using screenings: A critical review including guidelines for clinical and research use. Current HIV/AIDS Reports, 14(3), 83–92. https://doi.org/10.1007/s11904-017-0349-9
- Kinai, E., Komatsu, K., Sakamoto, M., Taniguchi, T., Nakao, A., Igari, H., Takada, K., Watanabe, A., Takahashi-Nakazato, A., Takano, M., Kikuchi, Y., & Oka, S. (2017). Association of age and time of disease with HIV-associated neurocognitive disorders: A Japanese nationwide multicenter study. Journal of NeuroVirology, 23(6), 864–874. https://doi.org/10.1007/s13365-017-0580-6
- Kwasa, J., Cettomai, D., Lwanya, E., Osiemo, D., Oyaro, P., Birbeck, G. L., Price, R. W., Bukusi, E. A., Cohen, C. R., & Meyer, A. L. (2012). Lessons learned developing a diagnostic tool for HIV-associated dementia feasible to implement in resource-limited settings: Pilot testing in Kenya. PLoS ONE, 7(3), e32898. https://doi.org/10.1371/journal.pone.0032898
- Manning, V., Gooden, J. R., Cox, C., Petersen, V., Whelan, D., & Mroz, K. (2021). Managing cognitive impairment in AOD treatment: Practice guidelines for healthcare professionals. Turning Point.
- Mapstone, M., Hilton, T. N., Yang, H., Guido, J. J., Luque, A. E., Hall, W. J., Dewhurst, S., & Shah, K. (2013). Poor aerobic fitness may contribute to cognitive decline in HIV-infected older adults. Aging and Disease, 4(6), 311–319. https://doi.org/10.14336/AD.2013.0400311
- Murray, K. J., Cummins, D., Batterham, M., Trotter, G., Healey, L., & O'Connor, C. C. (2016). Does the informal caregiver notice HIV associated mild cognitive impairment in people living with HIV? AIDS Care, 28(2), 221–227. https://doi.org/10.1080/09540121.2015.1084989
- Musso, M. W., Cosgrove, S. J., Peltier, M. R., McGee, B. L., & Jones, G. N. (2018). Problems screening for HAND among the educationally disadvantaged. Applied Neuropsychology: Adult, 25(2), 120–125. https://doi.org/10.1080/23279095.2016.1248766
- Nasreddine, Z. S., Phillips, N. A., Bedirian, V., Charbonneau, S., Whitehead, V., Collin, I., Cummings, J. L., & Chertkow, H. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699. https://doi.org/10.1111/j.1532-5415.2005.53221.x
- Neuropsychology.org. (n.d.). Neuropsychology. Retrieved December 16, 2022, from http://www.neuropsychology.org.au/
- Nightingale, S., Ances, B., Cinque, P., Dravid, A., Dreyer, A. J., Gisslén, M., Joska, J. A., Kwasa, J., Meyer, A. C., Mpongo, N., & Winston, A. (2023). Cognitive impairment in people living with HIV: Consensus recommendations for a new approach. Nature Reviews Neurology, 19(7), 424–433. https://doi.org/10.1038/s41582-023-00813-2
- Nightingale, S., Cinque, P., Dravid, A., Dreyer, A. J., Gisslén, M., Joska, J. A., Kwasa, J., Meyer, A., Mpongo, N., Nakasujja, N., Pebody, R., Pozniak, A., Price, R. W., Saylor, D., Thomas, K. G. F., Underwood, J., Vera, J. H., & Winston, A. (2024). Reply to ‘Cognitive criteria in HIV: Greater consensus is needed’. Nature Reviews Neurology, 20(2), 129–130. https://doi.org/10.1038/s41582-024-00928-0
- Obermeit, L., Beltran, J. Casaletto, K., Franklin, D., Letendre, S., Ellis, R., Fennema-Notestine, C., Vaida, F., Collier, A., Marra, C., Clifford, D., Gelman, B., Sacktor, N., Morgello, S., Simpson, D., McCutchan, J., Grant, I., & Heaton, R. (2017). Evaluating the accuracy of self-report for the diagnosis of HIV-associated neurocognitive disorder (HAND): Defining “symptomatic” versus “asymptomatic” HAND. Journal of NeuroVirology, 23(1), 67–78. https://doi.org/10.1007/s13365-016-0474-z
- Parry, S., Zetler, S., Kentridge, A., Petrak, J., & Barber, T. (2017). Simple screening for neurocognitive impairment in routine HIV outpatient care: Is it deliverable? AIDS Care, 29(10), 1275–1279. https://doi.org/10.1080/09540121.2017.1300632
- Peters, M. D., Godfrey, C. M., McInernery, P., Soares, C. B., Khalil, H., & Parker, D. (2015). The Joanna Briggs Institute reviewers’ manual 2015: Methodology for JBI Scoping reviews. The Joanna Briggs Institute.
- Peters, M. D., Marnie, C., Tricco, A. C., Pollock, D., Munn, Z., Alexander, L., McInerney, P., Godfrey, C. M., & Khalil, H. (2020). Updated methodological guidance for the conduct of scoping reviews. JBI Evidence Synthesis, 18(10), 2119–2126. https://doi.org/10.11124/JBIES-20-00167
- Queensland Positive People (QPP). (2022). HIV-associated neurological disorders. Retrieved December 16, 2022, from https://www.qpp.org.au/hiv-associated-mnd-mild-neurocognitive-disorder/
- Sacktor, N., Skolasky, R. L., Seaberg, E., Munro, C., Becker, J. T., Martin, E., Ragin, A., Levine, A., & Miller, E. (2016). Prevalence of HIV-associated neurocognitive disorders in the Multicenter AIDS Cohort Study. Neurology, 86(4), 334–340. https://doi.org/10.1212/WNL.0000000000002277
- Sinclair, J. (2023, August 28). Australian R&D spending drops as percentage of GDP. https://www.researchprofessionalnews.com/rr-news-australia-politics-2023-8-australian-r-d-spending-drops-as-percentage-of-gdp/
- Tedaldi, E. M., Minniti, N. L., & Fischer, T. (2015). HIV-associated neurocognitive disorders: The relationship of HIV infection with physical and social comorbidities. Biomed Research International, 2015, 641913. https://doi.org/10.1155/2015/641913
- The Kirby Institute. (2023). HIV, viral hepatitis and sexually transmissible infections in Australia Annual Surveillance Report 2023.
- Thompson, F., Cysique, L. A., Harriss, L. R., Taylor, S., Savage, G., Maruff, P., & McDermott, R. (2020). Acceptability and usability of computerized cognitive assessment among Australian indigenous residents of the Torres Strait Islands. Archives of Clinical Neuropsychology, 35(8), 1288–1302. https://doi.org/10.1093/arclin/acaa037
- Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850
- Underwood, J., & Winston, A. (2016). Guidelines for evaluation and management of cognitive disorders in HIV-positive individuals. Current HIV/AIDS Reports, 13(3), 235–240. https://doi.org/10.1007/s11904-016-0324-x
- Wang, Y., Liu, M., Lu, Q., Farrell, M., Lappin, J. M., Shi, J., Lu, L., & Bao, Y. (2020). Global prevalence and burden of HIV-associated neurocognitive disorder: A meta-analysis. Neurology, 95(19), e2610–e2621. https://doi.org/10.1212/WNL.0000000000010752
- Zigmond, A. S., & Snaith, R. P. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x

