Sirs,
Ano-genital infection by human papillomavirus (HPV) can cause neoplastic lesions (Citation[1],Citation[2]), most notably in HIV-positive patients (Citation[3]) in whom the risk seems to be higher when CD4+ lymphocytes are < 200 cells/mm3 (Citation[4]). We describe a case of penile intraepithelial carcinoma that occurred in an HIV-positive male receiving topical imiquimod 1%.
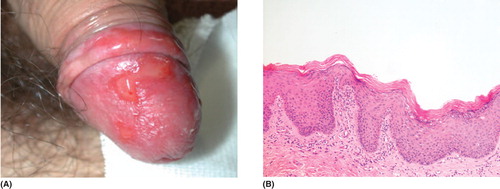
An HIV positive male came to our department in 1998 for the onset of genital warts on his balano-preputial sac. We made several diathermies of the relapsing warts. In 2000, the patient started imiquimod 5% three times a week, resolution of the lesions being observed within 2 months. In March 2004, a new lesion occurred in the previously treated area. Clinical and histological examinations revealed intraepithelial carcinoma ( and ). The patient restarted imiquimod 5% which caused intense local inflammation. Resolution was obtained within 1 year with several periods of no treatment due to side effects. In 2006, the lesion relapsed and the patient refused imiquimod. He first started photodynamic therapy and then cidofovir 1% cream, both were interrupted due to local side effects. In April 2007, we performed a new histological examination which confirmed the previous diagnosis. Meanwhile, the patient started a new antiretroviral protocol. Despite the immunological improvement, the lesion remained unchanged and imiquimod 1% was initiated. The patient is still applying this preparation five times a week; the drug is now better tolerated and equally effective, no evolution of the lesion to invasive carcinoma having taken place ().
Figure 1. (A) Clinical features of the intraepithelial carcinoma at the onset. (B) Histological features of the intraepithelial carcinoma at the onset (hematoxylin-eosin).
This case is interesting because of its long clinical course marked by two different periods: the first one characterized by genital warts and the second one by intraepithelial carcinoma. Such a long course is not surprising since HIV-related immunodeficiency can influence the ability of HPV to persist in the organism, proliferate or play its carcinogenic role (Citation[4]). It is, on the contrary, worth emphasizing that the genital warts responded rapidly to imiquimod 5%, whereas this concentration was not tolerated when used against the carcinoma. We can speculate that the thickness and keratinization of the carcinoma, lower than the warts' ones, are responsible for higher drug absorption, leading to more severe inflammation. Moreover, the carcinoma's intrinsic features might cause a more intense immunological response to imiquimod. Also, the improvement of immunological conditions caused by the antiretroviral therapy might play a role in inducing such an inflammatory reaction.
Imiquimod is particularly suitable for intraepithelial carcinomas of the ano-genital area because it avoids wide tissue losses and allows regional treatment, which is indispensable due to the multi-centric nature of HPV infection (Citation[5],Citation[6]). The use of imiquimod at a lower concentration can be hypothesized in order to improve tolerability, thus allowing the regular application of the drug. Such a therapeutic schedule seems to be able to control HPV proliferation and to avoid neoplastic evolution. Careful and regular clinical and histological follow-up is mandatory.
References
- Paavonen J. Human papillomavirus infection and the development of cervical cancer and related genital neoplasias. Int J Infect Dis. 2007; 11: S3–9
- Palefsky JM. HPV infection in men. Dis Markers. 2007; 23: 261–72
- Kreuter A, Brockmeyer NH, Hochdorfer B, Weissenborn SJ, Stucker M, Swoboda J, et al. Clinical spectrum and virologic characteristics of anal intraepithelial neoplasia in HIV infection. J Am Acad Dermatol. 2005; 52: 603–8
- Frisch M, Biggar RJ, Goedert JJ. Human papillomavirus- associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J Natl Cancer Inst. 2000; 92: 1500–10
- Hober D, Ajram L, Chehadeh W, Lazrek M, Goffard A, Dewilde A, et al. [Mechanisms of imiquimod indirect antiviral activity.] Ann Biol Clin. (Paris). 2005; 63: 155–63
- Wendling J, Saiag P, Berville-Levy S, Bourgault-Villada I, Clerici T, Moyal-Barracco M. Treatment of undifferentiated vulvar intraepithelial neoplasia with 5% imiquimod cream. Arch Dermatol. 2004; 140: 1220–4

