Sirs,
We describe a 26-year-old Chinese girl in whom vitiligo developed on the neck and left shoulder when she was 20 years old. The vitiligo stopped spreading 3 years later. She had received medical treatment but without any repigmentation. In May 2007, after written consent, she received an initial transplantation of autologous minigrafts to a 58-cm2 depigmented area as a trial (). After successful pigmentation was observed in that area (), she received the second similar treatment to other vitiliginous skin areas of larger sizes (64 cm2; ). Approximately 95% of treated vitiliginous skin was repigmented after two transplantations.
Figure 1. (A) Segmental vitiligo on the left shoulder before the first operation; (B) repigmentation took place within 4 weeks, with slight hyperpigmentation and redness; (C) successful pigmentation was observed 7 months after the first operation.
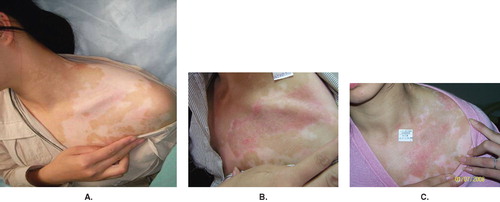
Figure 2. (A) Segmental vitiligo on the left shoulder and neck before the second operation; (B) repigmentation gradually took place 2 months after the second operation; (C) approximately 95% of treated vitiliginous skin was repigmented 7 months after the second operation.

The epidermis at the recipient site was removed by superficial abrasion with an ultra-pulsed CO2 laser (Lumenis Ltd, USA) (225 mJ/pulse, 40 pulse/s). After abrasion, the depigmented site was covered with gauze which had been soaked in physiological saline to prevent the site from being polluted. A very thin piece of epidermal graft skin (0.10–0.15 mm) was taken from a normally pigmented donor site under local anesthesia, mainly the buttock, with a hand dermatome. The size of the donor skin was usually one-sixth or one-tenth of the depigmented area. The epidermis was then put in a curved plate containing physiological saline and was cut into tiny pieces (about 1 mm2) with ophthalmic scissors. Then the tiny pieces were spread evenly on the tissue to cover the recipient site. The transplant was secured with Trex non-adherent silicone-treated gauze covered with gauze moistened with normal saline, followed by Tegaderm dressing. At 8–10 days later, all dressings were removed. The patient was encouraged to expose the treated area to natural sunlight with caution.
Clinical repigmentation gradually took place within 4 weeks after each treatment. A slight hyperpigmentation and redness presented initially, but then faded gradually (). Two months later, the treated areas acquired a color similar to the surrounding skin () and this appearance remained unchanged at the 7-month follow-up (). The total repigmented portion was 95% of the total treated areas (122 cm2). No hypertrophic scars or other complications were observed at recipient or donor areas.
Surgical interventions are useful only when lesions become stable and refractory to medical treatments in selected patients. Treatment of stable refractory vitiligo with epidermal grafting or the transplantation of cultured or non-cultured melanocytes has been reported previously (Citation[1]). Both methods had showed good results. However, epidermal grafting had disadvantages such as long suction blister time (about 60 minutes) and the restricted size of recipient areas (Citation[2]). Although cultured melanocyte grafting is expected to be used for treating large areas, high requirements on its technology and equipment baffle its promotion (Citation[1]). In 2002, Katsuhiko et al. (Citation[3]) reported a therapy combining ‘seed-graft’ with PUVA radiation, with an effective rate of 100% in three cases of stable refractory vitiligo. But the area they grafted was located just on the face and neck, and they did not mention the size of the recipient area. In reference to the Meek technique (Citation[4]) in the treatment of severe burns, we proposed a modified method using smaller skin sheets (1 × 1 mm2) than the Meek one (3 × 3 mm2) as skin grafts to treat vitiligo. Ultra-pulsed CO2 lasers have been used in dermatology for several years (Citation[5],Citation[6]). The pulse length of this laser is 600–900 μs and is shorter than the thermal relaxation time of the epidermal cells (695–950 μs). Thus, thermal damage in the surrounding tissue can be neglected (Citation[7]). So we adopted ultra-pulsed CO2 laser abrasion with transplantation of autologous minigrafts to treat a large area of stable vitiligo and we had satisfying clinical results.
In our patient, repigmentation occurred in a diffuse and not in a follicular pattern, indicating that it originated from the transplanted minigrafts. The transplantation of autologous minigrafts seems to be an effective treatment for a large area of segmental stable refractory vitiligo and to be able to repigment by retrograde migration of melanocytes (Citation[8]). The advantages of transplantation of autologous minigrafts include an easy surgical procedure, coverage of large depigmented lesions, and production of a homogeneous skin color. Furthermore, faster and deeper repigmentation has been observed when PUVA is used. However, this patient did not receive PUVA treatment. She was encouraged to expose the treated area to natural sunlight 10 minutes daily after each surgery. Further controlled studies of this treatment are needed.
Acknowledgement
This research was supported in part by a grant from the National Natural Science Foundation of China (no. 30671896), a grant from the Board of Health, Hangzhou City (no. 0070433Q01).
I am extremely thankful to Prof Yule Wu for his help and guiding.
References
- Falabella R. Surgical approaches for stable vitiligo. Dermatol Surg. 2005; 31: 1277–84
- Kahn AM, Cohen MJ. Vitiligo: Treatment by dermabrasion and epithelial sheet grafting. J Am Acad Dermatol. 1995; 33: 646–8
- Tsukamoto K, Osada A, Kitamura R, Ohkouchi M, Shimada S, Takayama O. Approaches to repigmentation of vitiligo skin: New treatment with ultrasonic abrasion, seed-grafting and psoralen plus ultraviolet A therapy. Pigment Cell Res. 2002; 15: 331–4
- Lari AR, Gang RK. Expansion technique for skin grafts (Meek technique) in the treatment of severely burned patients. Burns. 2001; 27: 61–6
- Baker TM. Dermabrasion. As a complement to aesthetic surgery. Clin Plast Surg. 1998; 25: 81–8
- Christian MM, Moy RL. Treatment of Hailey--Hailey disease (or benign familial pemphigus) using short pulsed and short dwell time carbon dioxide lasers. Dermatol Surg. 1999; 25: 661–3
- Raulin C, Greve B, Hammes S. The combined continuous-wave/pulsed carbon dioxide laser for treatment of pyogenic granuloma. Dermatol Surg. 2002; 138: 33–7
- Yones SS, Palmer RA, Garibaldinos TM, Hawk JL. Randomized double-blind trial of treatment of vitiligo: Efficacy of psoralen-UV-A therapy vs narrowband-UV-B therapy. Arch Dermatol. 2007; 143: 578–84
