Abstract
Background
As pilomatricoma is a common adnexal skin tumor often occurring in exposed areas, dermatologists focus on minimizing postsurgical scarring.
Methods
This retrospective study included patients aged < 19 years who underwent surgical treatment for pilomatricoma at a single university hospital from 2015 to 2021. Patient demographics, tumor characteristics, and surgical outcomes were analyzed according to the surgical methods including punch incision and elliptical excision.
Results
Overall, 75 patients and 79 lesions were included in the study. The mean age of the patients was 8.4 years, and 48 patients (64.0%) were females. The face was the most common site of pilomatricoma (51.9%), and within the face, the cheeks were the most common sites. No recurrence was observed in the elliptical excision group, while one case of recurrence (4.5%) was observed in the punch incision group. The mean length of the wound was 2.00 cm in the elliptical excision group, which was longer than that in the punch incision group (0.49 cm; p < .001).
Conclusions
Considering that surgery is the gold standard treatment for pilomatricoma, punch incision may be useful as an alternative surgical option for pilomatricoma in children.
Introduction
Pilomatricoma is a benign tumor originating from the matrix cells of a hair follicle and is a common adnexal skin tumor (Citation1). Surgical excision is the treatment of choice; however, there are no standard guidelines regarding the techniques and appropriate margins to be achieved (Citation1). It often occurs in exposed areas, such as the face and neck (Citation1,Citation2), which are cosmetically sensitive areas, and is more common in children; therefore, there is a need to minimize the surgical site and operating time. A punch is an instrument for skin biopsy that dermatologists can access easily and can be used to remove various skin tumors (Citation3). Therefore, this study aimed to evaluate pediatric patients who underwent elliptical excision or punch incision for pilomatricoma.
Materials and methods
Study design
This retrospective study included patients aged < 19 years who underwent surgical treatment for pilomatricoma at Chosun University Hospital between January 2015 and December 2021. The data analyzed included patient demographics, tumor characteristics, and surgical outcomes. Local recurrence was defined as occurrence of the same lesion. When there was no medical record of recurrence or complications, the data were assessed through wire-line calls with the patients or their caregivers. This study was approved by the Institutional Review Board of Chosun University Hospital (no. 2020-12-031).
Surgical procedure
The surgical treatments for pilomatricoma included elliptical excision based on the traditional elliptical radical excision method using a no. 15 surgical scalpel blade and punch incision based on the surgical excision method using a punch. Punch incision was performed as follows:
The lesion boundaries were marked using a surgical pen based on direct visualization by the naked eye by a surgeon or dermoscopy.
The surgical site was anesthetized using 1% lidocaine with 1:100,000 epinephrine solution.
After usage of a disposable 3–4-mm punch at the center of the lesion boundaries, the tumor materials were exposed by applying lateral pressure to the surrounding skin.
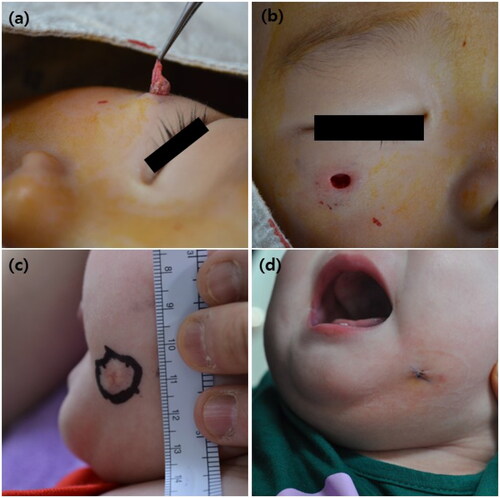
Dissection between the tumor and surrounding tissue was performed using iris scissors, and as much of the tumor as possible was removed (). When the tumor was too large for dissection, it was cut into small pieces using a punch and pulled out using forceps.
After main mass removal, the remaining walls and materials were removed using curettes or iris scissors. The process was repeated until the materials did not emerge in any direction from the incision hole.
Following sufficient irrigation with isotonic sodium chloride solution, the surgeon carefully inspected the wound for evidence of remnant lesions ().
The wound was closed with only one or two simple interrupted sutures (). When the tumor was large and a deeper defect was expected to remain, deep dermal suturing was performed using absorbable sutures.
Figure 1. Clinical images of the punch incision method. Patient 1: (a) removal of the main mass. (b) Appearance of the defect after inspection to ensure that the lesion is removed. Patient 2: (c) clinical manifestation of pilomatricoma before punch incision and long axis of the lesion (1.5 cm). (d) Clinical image taken after wound closure; the wound length did not exceed 0.6 cm.
In contrast, elliptical excision was performed with the incision line oriented in the direction of the relaxed skin tension lines. The length-to-width ratio was 3:1, and the apical angle was designed to be smaller than 30°. Two-layered suturing, including the deep dermal and epidermal layers, was performed.
Statistical analysis
Statistical analysis was performed to determine whether there were significant differences between the groups according to the surgical procedure. Student’s t-test was performed to analyze the differences in age, tumor duration, long axis length, and long axis wound size and Pearson’s Chi-square test in all other variables. These tests were performed using SPSS v22.0 (IBM Corp., Armonk, NY), and p < .05 was considered statistically significant.
Results
Patient demographic data
A total of 75 patients with 79 lesions were included herein. Their mean age was 8.4 years (range: 6 months to 18 years), and 48 patients (64.0%) were women. Five patients (6.7%) had a treatment history, and none reported a family history of pilomatricoma. Although no patient had a history of trauma at the lesion site, one patient reported that the lesion occurred at the vaccination injection site.
Tumor characteristics and surgical outcomes
The face was the most common tumor site (51.9%), followed by the upper extremities (22.8%). On the face, pilomatricoma mostly occurred on the cheeks, followed by the periorbital areas. The mean tumor duration until surgery was 7.4 months, and the mean long axis length was 1.01 cm. Additionally, pain was reported in 51 lesions (64.6%), and most skin over the tumor was erythematous (40.5%) and flesh-colored (39.2%). The lesions were more distributed on the face; the tumor duration was shorter; and the tumor size was smaller in the punch incision group than in the elliptical excision group. However, the difference was not significant (). Complications were observed in two cases in the elliptical excision group, in which keloids developed at the surgical site. No recurrence was observed in the elliptical excision group, while one case of recurrence was observed in the punch incision group during a mean follow-up period of 27.6 and 20.3 months, respectively. The mean long axis length of the postoperative wound was 2.00 cm in the elliptical excision group, which was longer than that in the punch incision group (0.51 cm) (p < .001) ().
Table 1. Tumor characteristics.
Table 2. Surgical outcomes.
Discussion
Pilomatricoma usually is presented as calcified nodules in the dermis or subcutaneous fat with various clinical features (Citation4). It is known to occur most commonly during the first decade of life (Citation1,Citation4). Indeed, there are reports (Citation5,Citation6) that pilomatricoma is a common surgically resected skin tumor in children. Therefore, it is relatively easy for clinicians to consider pilomatricoma as a diagnosis of skin tumors in pediatric patients, which explains the high initial diagnostic accuracy of 79.7% in this study. Pilomatricoma commonly occurs in the head and neck (Citation1,Citation2). Consistently, 67.1% of the cases occurred in the head and neck in this study. As pilomatricoma does not show spontaneous remission, surgical excision should be considered. For young patients, dermatologists are concerned of the treatment timing and method because children may be uncooperative with surgery and anesthesia (Citation1,Citation2). As it can lead to additional damage with pilomatricoma occurrence, early excision yields a better cosmetic outcome (Citation2). In this situation, a large surgical area can be a burden to the surgeon.
Punches have the advantages of being relatively easy to handle and access and having minimal complications (Citation3). They can be used for the most common biopsies as well as mole excision, lipoma extraction, and cyst removal (Citation3,Citation7,Citation8). Additionally, pilomatricoma can be successfully treated using a 4-mm punch and 25% trichloroacetic acid (Citation9). The most important advantage of tumor resection using punches is the good cosmetic outcome owing to minimal surgical wound. Herein, punch incision yielded a smaller wound size than did elliptical excision (p < .001), and the size did not exceed 0.6 cm. This small wound size not only has an advantage in cosmetic outcomes but also eases the burden on surgeons. However, a major concern with punch incision is the risk of recurrence. The recurrence rate of pilomatricoma was 4.5% in this study, which is similar to other results of cyst removal using punches (3.2–15.0%) (Citation7,Citation8,Citation10). Further, there was no significant difference in the recurrence rate between the groups (p = .105) in this study. Recurrence after punch incision appears to have occurred because of the incomplete tumor removal. Therefore, because there was no significant difference in the recurrence rates between the two surgical procedures, punch incision may be a useful alternative surgical option for pilomatricoma in children, considering that pilomatricoma occurs more frequently in exposed areas and is more common in younger patients who are cosmetically sensitive. Additionally, if pilomatricoma is strongly suspected during punch biopsy, tumor resection can be attempted at the biopsy site, and examination and treatment can be performed simultaneously.
This study had several limitations. First, this was a single-center study with a small sample size. Second, because this was a retrospective study, there was no evaluation of patient satisfaction and cosmetic outcomes according to the surgical method. Additionally, the lesions treated with punch incision were smaller than those treated with elliptical excision, which might have depended on the operator’s preferences; therefore, further well-designed head-to-head comparison studies are needed to verify our results.
Punch incision may be used as an alternative surgical option for pilomatricoma in pediatric patients. We hope that this result will be helpful in determining the appropriate treatment method for pilomatricoma.
Patient consent
Informed consent for image publication was obtained from the parents of the patients.
Disclosure statement
All authors declare no conflict of interest.
References
- Hernández-Núñez A, Nájera Botello L, Romero Maté A, et al. Retrospective study of pilomatricoma: 261 tumors in 239 patients. Actas Dermosifiliogr. 2014;105(7):699–705.
- Oh YW, Suh HS, Choi YS. Optimal timing of surgical excision in pediatric pilomatricoma: association between clinicopathological features and cosmetic outcomes. Ann Dermatol. 2020;32(2):93–100.
- AlGhamdi KM, AlEnazi MM. Versatile punch surgery. J Cutan Med Surg. 2011;15(2):87–96.
- Zamanian A, Farshchian M, Farshchian M. Clinical and histopathologic study of pilomatricoma in Iran between 1992 and 2005. Pediatr Dermatol. 2008;25(2):268–269.
- López V, Martín JM, Monteagudo C, et al. Epidemiology of pediatric dermatologic surgery: a retrospective study of 996 children. Actas Dermosifiliogr. 2010;101(9):771–777.
- Wyatt AJ, Hansen RC. Pediatric skin tumors. Pediatr Clin North Am. 2000;47(4):937–963.
- Cheeley J, Delong Aspey L, MacKelfresh J, et al. Comparison of elliptical excision versus punch incision for the treatment of epidermal inclusion cysts: a prospective, randomized study. J Am Acad Dermatol. 2018;79(2):360–361.
- Lee HE, Yang CH, Chen CH, et al. Comparison of the surgical outcomes of punch incision and elliptical excision in treating epidermal inclusion cysts: a prospective, randomized study. Dermatol Surg. 2006;32(4):520–525.
- Maranda EL, Riyaz F, Shwayder T. Punch and scoop technique for removing pilomatricoma. Pediatr Dermatol. 2017;34(5):622–623.
- Mehrabi D, Leonhardt JM, Brodell RT. Removal of keratinous and pilar cysts with the punch incision technique: analysis of surgical outcomes. Dermatol Surg. 2002;28(8):673–677.

