Abstract
Background and objectives
There has been no validated tool for objectively quantifying the overall condition and characteristics of the scalp. This study aimed to establish and validate a new classification and scoring system for evaluating scalp conditions.
Methods
The Scalp Photographic Index (SPI) using a trichoscope grades five features of scalp conditions (dryness, oiliness, erythema, folliculitis, and dandruff) on a score of 0–3. To evaluate the validity of SPI, SPI grading was performed by three experts on the scalps of 100 subjects along with a dermatologist’s assessment of the scalps and a scalp-related symptom survey. For reliability assessment, 20 healthcare providers performed SPI grading for the 95 selected photographs of the scalp.
Results
SPI grading and the dermatologist’s scalp assessment showed good correlations for all five scalp features. Warmth showed a significant correlation with all features of SPI and the subjects’ perception of a scalp pimple had a significant positive correlation with the folliculitis feature. SPI grading demonstrated good reliability with excellent internal consistency (Cronbach’s α = 0.90) and strong inter- and intra-rater reliability (Kendall’s W = 0.84, ICC(3,1)=0.94).
Conclusions
SPI is an objective, reproducible, and validated numeric system for classifying and scoring scalp conditions.
Introduction
Scalp-related symptoms such as dandruff or pruritus are very common problems encountered in dermatological practice (Citation1). These symptoms are commonly associated with various inflammatory scalp disorders, including seborrheic dermatitis, atopic dermatitis, and psoriasis. Even when the patients’ symptoms are similar, the underlying scalp conditions can be very different. For example, dandruff is considered as a Malassezia yeast-related condition and treated with antifungal agents; however, a recent study of 54 Koreans with dandruff found that nearly half of the subjects had sebum levels that were even lower than in healthy controls (Citation2), suggesting a different pathophysiology between scalps with dry vs. oily dandruff. Classification of scalp conditions or types is important for personalized treatment with the increasing demand for better scalp health. However, to date, scalp evaluation has been mainly focused on hair loss (Citation3,Citation4), and there has been no systematic evaluation methods for scalp skin conditions. Although the Baumann skin type system is popular for classifying the types of glabrous skin, especially the facial skin, it has limitations when applied to the scalp (Citation5).
One of the reasons why studies on scalp conditions or types are scarce is that the scalp is more difficult to observe than the glabrous skin. People cannot directly observe their scalp, and because it is covered with hair, investigators face challenges in photo documentation of the scalp and subsequent communication with other investigators. Although several studies have been conducted to diagnose inflammatory scalp disorders using dermoscopy, which allows observation of the scalp structures in detail (Citation6–8), no attempt has yet been made to classify the physiological characteristics of scalps.
In this study, we aimed to introduce the Scalp Photographic Index (SPI), a new, objective, reproducible numeric grading system that describes the scalp conditions. SPI grades five features of the scalp conditions using magnified photographs of the scalp. We evaluated the validity of SPI through the correlation with the dermatologist’s assessment of the scalps and the subjects’ scalp-related symptoms. We also evaluated the internal consistency and inter- or intra-rater reliability of SPI.
Materials and methods
Development of the Scalp Photographic Index
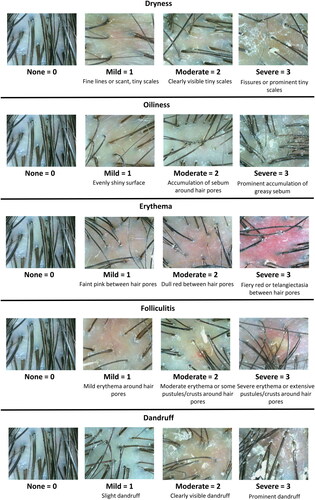
The SPI was prepared using highly magnified (×60) pictures of the scalp taken by a trichoscope. SPI grades five features of scalp conditions (dryness, oiliness, erythema, folliculitis, and dandruff) to 0 (none), 1 (mild), 2 (moderate), and 3 (severe) using magnified photographs of the scalp. Each item reflects scalp characteristics that are important for deciding treatments. For example, dryness reflects epidermal barrier integrity or scalp hydration level, whereas oiliness shows sebaceous activity. Erythema and folliculitis are manifestations of interfollicular and follicular inflammations, respectively. Hyper-proliferative epidermal response is indicated by dandruff. To improve the objectivity and reproducibility of grading, a photographic scale was used. Detailed methods are as follows.
A 60-fold magnified images were acquired from five areas of the scalp (vertex, anterior, posterior, right, and left) using a scalp photography equipment (ASM-202™ camera, Aram Huvis Co., Ltd., Seongnam, South Korea) (Citation7). The ASM-202™ camera was a hand-held trichoscope that took non-polarized, non-reflective images by non-reflective lighting. Compared to the dermoscope, it had a shorter shooting time (<0.5 seconds) and was easier to observe the scalp surface by obtaining non-reflection images regardless of lighting with a fixed focusing (). The patients were instructed not to wash their scalps or use hair products within 12 hours before taking the pictures, and we used the Scalp Positioning Ruler to replicate the exact spot of each picture in the long-term evaluation of a patient (). Here, anterior and posterior refer to the center of the anterior and posterior hair lines, respectively. Right and left scalp images were photographed from just above the right and left ear, respectively ().
Dryness (fine lines or tiny scales on the scalp surface), oiliness (greasy sebum or shine on the scalp surface), erythema (erythema or telangiectasia between the hair pores), folliculitis (erythema or pustules of hair pores), and dandruff (coarse and large white scales) were chosen to evaluate scalp conditions.
With each image of the five areas, the severity of the five features was evaluated on a four-grade scale: 0 (normal), 1 (mild), 2 (moderate), and 3 (severe) using a photographic scale. Detailed descriptions and the photographic scale for each feature are shown in .
The sum of each score reflects the overall severity of scalp problems and features with scores 2 or 3 help to classify scalp conditions. The SPI score was defined as the sum of the severity scores of the five features. The SPI score of one area ranged from 0 to 15 points. The total SPI score (0–75 points) is the sum of the SPI score of five areas: vertex, anterior, posterior, right, and left (). This represents the overall severity of an undesirable condition of the scalp. The scalp type was defined as the features with scores 2 or 3. For example, a scalp with grade 2 or 3 oiliness and dandruff can be defined as the ODa type, whereas a scalp with dryness and erythema can be classified as the DE type.
Figure 1. (a) A scalp image taken with a dermoscope (×20 magnification, non-polarized, Dermlite DL4™, DermLite, San Juan Capistrano, CA). (b) A scalp image of the same individual taken with a trichoscope (×60 magnification, ASM-202™ camera, Aram Huvis Co., Ltd., Seongnam, South Korea). (c) The Scalp Positioning Ruler was used to constantly photograph five areas of the scalp. (d) Five areas to measure scalp conditions for the Scalp Photographic Index (vertex, anterior, posterior, right, and left).
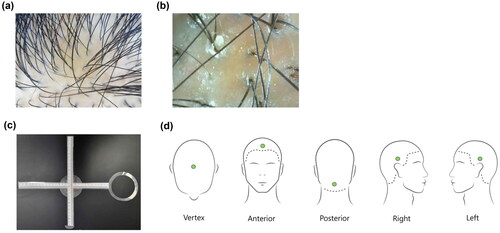
Figure 2. The photographic scale for the Scalp Photographic Index. Dryness is determined by fine lines, scales, and fissures of the surface; mild = 1 (fine lines or scant, tiny scales), moderate = 2 (clearly visible tiny scales), and severe = 3 (fissures or prominent tiny scales). Oiliness is determined by sebum accumulation and shine of the surface; mild = 1 (evenly shiny surface), moderate = 2 (accumulation of sebum around hair pores), and severe = 3 (prominent accumulation of greasy sebum). Erythema is determined by erythema and telangiectasia between the hair pores; mild = 1 (faint pink between hair pores), moderate = 2 (dull red between hair pores), and severe = 3 (fiery red or telangiectasia between hair pores). Folliculitis is determined by erythema and pustules of hair pores; mild = 1 (mild erythema around hair pores), moderate = 2 (moderate erythema or some pustules/crusts around hair pores), and severe = 3 (severe erythema or extensive pustules/crusts around hair pores). Dandruff is determined by coarse and large scales of the surface; mild = 1 (slight dandruff), moderate = 2 (clearly visible dandruff), and severe = 3 (prominent dandruff).
Validity assessment
To evaluate whether the SPI grading adequately reflects the scalp condition, 100 healthy volunteers over the age of 19 years with scalp-related problems including itching, dandruff, excessive sebum or dryness were recruited. This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-2107-697-301), written informed consent was obtained from each participant. An expert dermatologist (J.I.N.) evaluated the severity of dryness, oiliness, erythema, folliculitis, and dandruff from 0 (normal) to 3 (severe) points after visual inspection of the subjects’ scalps. The SPI grading was performed for each participant using 60-fold magnified photographs taken from five designated areas of the scalp by three experts (J.I.N., J.W.S., and H.R.C.) and grades agreed by at least two of three experts were chosen for the analysis. To evaluate the subjective symptoms, subjects were asked to rate warmth, itch, pain, and pimple of the scalp from 0 (nothing) to 3 (worst) using a self-questionnaire. To evaluate the correlation between the SPI grading and the dermatologist’s evaluation and the SPI grading and the subjective symptoms, Pearson’s correlation test was performed. Data were analyzed using IBM SPSS version 20 (IBM Corp., Armonk, NY), and a p value <.05 was considered to be statistically significant.
Reliability assessment
A reliability assessment of the SPI grading was performed by 20 healthcare providers (10 dermatology residents, six dermatologists, and four nurses) using a questionnaire consisting of the ninety-five 60-fold magnification photographs of the scalp. The photographs included 74 images according to the severity of each subscale, 10 normal scalp images, and 11 pairs of duplicate images. The healthcare providers were briefly instructed on the method of the SPI grading and provided with the photographic scale for the SPI. The healthcare providers recorded their scores for the 95 scalp photos on an answer sheet. Each answer was reviewed and compared with the answers agreed upon by two out of three experts. Cronbach’s α for internal consistency and Kendall’s coefficient of concordance W (Kendall’s W) for inter-rater reliability were calculated using a total of 95 images. To measure intra-rater reliability, we calculated intra-class correlation coefficient (ICC) (Citation1, Citation3) with 11 pairs of duplicate images that were randomly selected among a total 95 images. ICCs and their 95% confidence intervals (CIs) were estimated based on a single measurement, absolute-agreement, two-way mixed effect model (Citation9). All reported p values <.05 were considered statistically significant. Statistical analyses were performed using R (version 4.0.1; R Foundation for Statistical Computing, Vienna, Austria) and R Studio (version 1.3.959; PBC, Boston, MA) with R packages ‘psych’ and ‘irr’.
Results
Validity of the Scalp Photographic Index
The average age of the 100 volunteers with scalp problems was 34.90 ± 7.85 years (range 19–61), and women accounted for 69.0% of the volunteers. The correlation analysis between the SPI grading and the dermatologist’s or subject’s evaluation of the scalp condition is summarized in . There was a statistically significant positive correlation between the dermatologist’s visual evaluation and each feature of the SPI grading (dryness, oiliness, erythema, folliculitis, and dandruff). This suggests that the SPI grading has significant relevance to an expert’s objective evaluation of the scalp condition.
Table 1. Relationship between the Scalp Photographic Index (SPI) and the scores evaluated by the patients and one investigator.
Among the subjects’ subjective symptoms, warmth showed a significant correlation with all features of the SPI grading. The subjects’ perception of a scalp pimple had a significant positive correlation with the folliculitis feature of the SPI grading. Itch or pain showed a negative or positive correlation, respectively, with erythema, but had no clinical implication.
Reliability of the Scalp Photographic Index
Values for Cronbach’s α greater than 0.70 are generally considered as a marker of high reliability, and Kendall’s W values greater than 0.80 and ICC values greater than 0.90 generally indicate excellent agreement (Citation10,Citation11). The SPI grading had excellent internal consistency (Cronbach’s α = 0.90). This means that different individual subscales of the SPI for evaluating scalp conditions give consistent and appropriate scores. The SPI grading also had excellent inter- and intra-rater reliability (Kendall’s W = 0.84; p value <.0001, ICC(3,1)=0.94; 95% CI 0.93–0.95) (). A higher Kendall’s W value means that the scores between the evaluators are consistent. Notably, as Kendall’s W values of dermatologists, dermatology residents, and nurses were all above 0.80, showing the SPI grading had good reproducibility between raters, regardless of the rater’s career. In addition, when Kendall’s W values were calculated for each subscale of the SPI, not only easily visible items such as erythema, folliculitis, and dandruff, but also items that were considered difficult to visually evaluate such as dryness and oiliness showed good inter-rater reliability. The ICC(3,1) of 0.94 evaluated with 11 pairs of duplicate images showed high intra-rater reliability, and the ICC(3,1) values within each subgroup of dermatologists, dermatology residents, and nurses were all 0.9 or higher, indicating excellent intra-rater reliability regardless of the rater’s career.
Table 2. Inter-rater and intra-rater reliabilities of the Scalp Photographic Index.
Discussion
When developing the scalp assessment tool, the following points were considered. First, the scalp assessment should reflect the scalp features that are clinically important. To address this, we chose five features, and defined a scalp type, which is determined by features scored 2 or 3. The scalp type aids quick and easy assessment of scalp condition and helps to choose treatments. For example, for DE type, which stands for dry scalp with interfollicular erythema, anti-inflammatory agents along with agents for the skin barrier recovery can be used. For OF type (oily scalp with folliculitis), anti-bacterial or anti-fungal agents can be used in addition to sebum-controlling agents. Although classifying scalp types cannot be used to diagnose specific diseases of the scalp, it can be used to provide personalized care by identifying the physiologic characteristics of individual scalps.
Second, the scalp assessment should be objective and reproducible. To meet this, we decided to use photographs and a photographic scale for scalp evaluation. Image-based assessment has several advantages. As the scalp condition can be recorded with photographs, the raters can consistently evaluate the scalp condition under the guidance of a photographic scale. The raters can also review their assessment and correct it if needed. Additionally, images can be examined by multiple raters, reducing rater-dependent bias. Another benefit of image-based assessment is that it allows the use of deep learning technology. Applying deep learning technology may improve the reliability of scalp assessment, considering deep learning algorithms’ expert-level classification capability of medical images (Citation12–14).
Third, the scalp assessment tool should be able to quantify the overall severity of scalp conditions. Although scalp-related problems are very common, to the best of our knowledge, there has been no tool to objectively quantify the overall condition and characteristics of the scalp. Some studies used different scalp severity scoring systems for their outcome measures, such as dandruff or seborrheic dermatitis, but these methods do not include the various scalp conditions holistically (Citation15,Citation16). The SPI score we proposed is defined as the sum of the severity scores of the five features. This represents the overall severity of an undesirable condition of the scalp. The SPI score allows a quantitative evaluation of scalp problems, and the sequential tracking of SPI score will be helpful to assess the treatment response. It can also be used as an outcome measure for future drug development and clinical trials.
In this study, we developed the SPI, a new assessment tool that incorporates all clinically relevant aspects of scalp conditions with excellent validity and reliability. For all five features, construct validity was verified by the good correlation between the SPI grading and the dermatologist’s assessment. The SPI grading was reliable with its strong internal consistency and excellent inter-rater and intra-rater agreements. It was especially noteworthy that the SPI grading showed high inter-rater reliability across dermatologists, dermatology residents, and even nurses who have little experiences in scalp assessment, indicating that the SPI grading is easily learned and provides consistent results regardless of professional knowledge.
Compared to glabrous skin, scalp is more difficult to photograph. To capture scalp photos, we tried various tools including a DSLR camera, a dermoscope, and selected a trichoscope with a ×60 magnification in consideration of the ease of photographing and image quality. With ×60 magnification photographs, we could observe not only easily visible features such as erythema, folliculitis, and dandruff, but also dryness and oiliness that were considered difficult to visually evaluate. In dry scalps, fine lines, tiny scales, or fissures were observed. Sebum was observed as a shiny wax-like substance on the surface of the scalp. Accumulation of sebum around hair pores or the entire scalp surface was observed in oily scalps (). Dryness and oiliness demonstrated the good validity and reliability as well as other features.
Our study had several limitations. First, the SPI grading evaluates only five representative areas, not the entire scalp. We measured only in five representative areas in consideration of the time and effort required for scalp assessment, but the measurement site could be modified according to the study. Second, the correlation between SPI grading and the biophysical measurements such as skin hydration, sebum levels were not investigated. The correlation between biophysical parameters could further support the validity of the SPI grading. Third, the SPI grading requires a trichoscope for scalp imaging. When compared to a dermoscope, a trichoscope is less widely used among dermatologists; however, we find it more convenient to observe scalp conditions. Unlike dermoscopes, trichoscopes are fixed-focusing, so non-experts can easily take well-focused photos. The SPI grading can be automated using deep learning of scalp images. In this case, non-experts will be able to evaluate the scalps by simply taking a picture with a trichoscope. Fourth, in this study, validity and reliability assessments were limited to SPI grading only, and SPI score or total SPI score were not validated. Since the reliability of SPI measurements by areas has not been validated, the possibility of variation according to the topographic area should be considered. Fifth, SPI grading was not validated for subjects with all levels of pigmentation, and people with deep pigmentation may not be able to be evaluated with this method because erythema may not be as readily visible, and reflectance of sebum might be different.
The SPI grading is a new, objective, reproducible, and validated numeric system used to classify scalp condition and measure the severity. The scalp type determined by SPI grading helps to assess the characteristics of patient’s scalps and to choose personalized treatment. The severity determined by SPI grading can be used to assess the treatment response, or to measure an outcome for future drug development and clinical trials.
Consent form
The patients in this manuscript have given written informed consent to publication of their case details.
Acknowledgements
IRB approval status: reviewed and approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-2107-697-301).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
For any purpose, with investigator support, anyone can request the data through email-id [email protected]
Additional information
Funding
References
- Misery L, Rahhali N, Duhamel A, et al. Epidemiology of dandruff, scalp pruritus and associated symptoms. Acta Derm Venereol. 2013;93(1):80–81.
- Yoon JS, Shim J, Lim JM, et al. Biophysical characteristics of dandruff-affected scalp categorized on the basis of sebum levels. J Cosmet Dermatol. 2021;20(3):1002–1008.
- Olsen EA, Roberts J, Sperling L, et al. Objective outcome measures: collecting meaningful data on alopecia areata. J Am Acad Dermatol. 2018;79(3):470–478.e3.
- Guarrera M, Cardo P, Arrigo P, et al. Reliability of Hamilton-Norwood classification. Int J Trichol. 2009;1(2):120–122.
- Baumann L. The skin type solution: a revolutionary guide to your best skin ever. New York: Bantam Books; 2006.
- Mubki T, Rudnicka L, Olszewska M, et al. Evaluation and diagnosis of the hair loss patient: part II. Trichoscopic and laboratory evaluations. J Am Acad Dermatol. 2014;71(3):431.e1–431.e11.
- Park DS, Koo JE, Oh SY, et al. Physiological profiles of hair and scalp conditions in Korea population: survey, hairological expert-diagnosis and new diagnostic device. Adv Bioeng Biomed Sci Res. 2021;4(2):63–71.
- Chang WJ, Chen LB, Chen MC, et al. ScalpEye: a deep learning-based scalp hair inspection and diagnosis system for scalp health. IEEE Access. 2020;8:134826–134837.
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163.
- Cassell SE, Bieber JD, Rich P, et al. The Modified Nail Psoriasis Severity Index: validation of an instrument to assess psoriatic nail involvement in patients with psoriatic arthritis. J Rheumatol. 2007;34(1):123–129.
- Simpson E, Bissonnette R, Eichenfield LF, et al. The Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD): the development and reliability testing of a novel clinical outcome measurement instrument for the severity of atopic dermatitis. J Am Acad Dermatol. 2020;83(3):839–846.
- Han SS, Park I, Eun Chang S, et al. Augmented intelligence dermatology: deep neural networks empower medical professionals in diagnosing skin cancer and predicting treatment options for 134 skin disorders. J Invest Dermatol. 2020;140(9):1753–1761.
- Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115–118.
- Haenssle HA, Fink C, Toberer F, et al. Man against machine reloaded: performance of a market-approved convolutional neural network in classifying a broad spectrum of skin lesions in comparison with 96 dermatologists working under less artificial conditions. Ann Oncol. 2020;31(1):137–143.
- Satchell AC, Saurajen A, Bell C, et al. Treatment of dandruff with 5% tea tree oil shampoo. J Am Acad Dermatol. 2002;47(6):852–855.
- Trznadel-Grodzka E, Błaszkowski M, Rotsztejn H. Investigations of seborrheic dermatitis. Part II. Influence of itraconazole on the clinical condition and the level of selected cytokines in seborrheic dermatitis. Postepy Hig Med Dosw. 2012;66:848–854.

