Dear Editor,
In Shared Decision Making (SDM), patients and physicians collaborate to make a decision regarding the best diagnostic or treatment option, taking patients’ values and preferences into account (Citation1). For psoriasis, many treatment options with more or less equal effectiveness and safety exist (Citation2). As patient preferences are pivotal in this treatment decision, SDM appears an appropriate approach. A survey among dermatologists and patients showed a clear need for SDM in psoriasis patients (Citation3). In this study, mentioned barriers to perform SDM for physicians were inexperience with SDM and short consultation times. For patients, barriers were inadequate information on SDM and treatment options (Citation3).
Some of these barriers can be vanquished by the use of specific Patient Decision Aids (PtDA). PtDAs explain to patients the different treatment options and help them consider their preferences. These PtDAs support physicians and patients in the decision making process (Citation4). Furthermore, PtDAs improve the knowledge of patients and reduce their feelings of being uninformed or unclear about their personal values, leading to more value-congruent choices (Citation4). We developed a PtDA for systemic therapy in psoriasis. More information on the development of this PtDA was published previously (Citation5).
In dermatology, limited research has been performed on PtDAs and their effect on SDM (Citation6,Citation7). Therefore, the objective of this study was to pilot the feasibility and effects of our PtDA on the level of SDM, as experienced by patients, physicians, and objective researchers in a before-and-after study. In a before-and-after study, observations are made in two separate patient groups; a control group that receives usual care (before group) and one that receives the intervention (after group) (Citation8). We designed and conducted this study at the dermatology department of the Amsterdam University Medical Center, a tertiary referral center for psoriasis. Patients and physicians gave informed consent for participating in this study. Our study was registered in the Netherlands Trial Register (Main ID NL8116). According to the Medical Ethics Review Committee of the Academic Medical Center in Amsterdam, ethical approval was not required to perform this study (reference number W19_299 # 19.356).
Patients who visited the outpatient clinic before introduction of the PtDA were included in the ‘before’ group (n = 15), and those visiting after introduction in the ‘after’ group (n = 15). Physicians (n = 14) discussed the completed PtDA from the after group during consultation. The primary outcome measure was the objective level of SDM assessed, using the OPTION5 questionnaire (Citation9). Two researchers independently rated the audio recorded consultations with this OPTION5 instrument. The secondary outcomes involved the level of SDM as perceived by physicians and patients. The patient questionnaire included the SDM-Q-9 questionnaire (Citation10) and the CollaboRATE questionnaire (Citation11). Physicians completed the SDM-Q-Doc questionnaire (Citation10). These scores were reported as percentages of maximum scores. Furthermore, a Visual Analogue Scale (VAS, from 0 – 9) to appreciate patient satisfaction and the Decisional Conflict Scale (DCS, 16 items on a scale from 0 ‘strongly disagree’ to 4 ‘strongly agree’) (Citation12) were collected.
Mean OPTION5 scores did not differ significantly before and after the PtDA introduction: 37.0 (SD 21.3) vs. 34.3 (SD 13.1), respectively (p = .68). The level of SDM experienced by patients and physicians however, was high; the SDM-Q-9 was 91.1% (IQR 75.6–95.6%) vs. 84.4% (IQR 75.6–88.9%); p = .27, before and after introduction. The SDM-Q-Doc was 75.6% (IQR 64.4–86.7%) vs. 71.1% (IQR 60.0–77.8%); p = .217, for the before and after studies. See for the SDM-Q-9 score per item. An overview of all outcomes can be seen in .
Figure 1. (a) Stacked bar chart SDM-Q-9 per item before and after introduction of the intervention. (b) Stacked bar chart SDM-Q-Doc per item before and after introduction of the intervention.
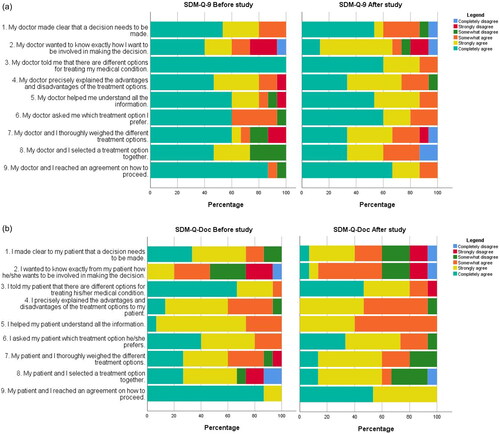
Table 1. Chosen treatment and effectiveness before-and-after study.
Since this study showed no significant differences before and after introduction of the PtDA, it might be possible to conclude that this PtDA does not increase the level of SDM among psoriasis patients. However, a few reasons can be mentioned for the absence of a difference in the level of SDM in the before and after study; firstly, this might be a consequence of the deficit of patients’ knowledge on SDM. Patients might have judged more subjective aspects, like the empathy of their physician (Citation13). Secondly, patients were usually referred to our center to start the treatment with biologics, for which we have special expertise. As can be seen in , 58.6% of the patients eventually started this treatment. Patients might have complete the PtDA with the wish to start biologics in mind and might not have felt the need for further SDM. Lastly, this study only investigated the effect of a PtDA on the level of SDM. This level might be higher if physicians would have known how to utilize a PtDA in their consultations e.g. through a consultation training (Citation3,Citation14).
A limitation for this study is the lack of recruitment in other hospitals. We started this study in two smaller hospitals, but no patients were included there.
Our findings indicate that there is room for improvement of SDM in the treatment of psoriasis patients. The contrast between the medium low objective and high subjective SDM levels suggest that it is of more importance to raise awareness of the concept of SDM, before trying to implement and study any tool to promote SDM.
Acknowledgments
We would like to thank Michiel Hageman (director of PATIËNT + Netherlands) for the technical development of the PtDA and his input on our paper.
Disclosure statement
AH was involved as sub-investigator in clinical trials for Abbvie, Lilly, LeoPharma and UCB. NR has no conflicts of interest. GK and PS were involved in the development of the PtDA investigated in this study. DU has no conflicts of interest. PS received a departmental independent research grants for TREAT NL registry from Pharma since December 2019 for the TREAT NL registry, is involved in performing clinical trials with many pharmaceutical industries that manufacture drugs used for the treatment of e.g. psoriasis and atopic dermatitis, for which financial compensation is paid to the department/hospital and, is Chief Investigator (CI) of the systemic and phototherapy atopic eczema registry (TREAT NL) for adults and children and one of the main investigator of the SECURE-AD registry.
Data availability statement
Our data is available on request. Data will be shared with researchers who provide a methodologically sound proposal after execution of a data-sharing agreement.
Additional information
Funding
References
- Elwyn G, Laitner S, Coulter A, et al. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146.
- Sbidian E, Chaimani A, Afach S, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database Syst Rev. 2022;5(5):CD011535.
- van der Kraaij GE, Vermeulen FM, Smeets PMG, et al. The current extent of and need for shared decision making in atopic dermatitis and psoriasis in the Netherlands: an online survey study amongst patients and physicians. J Eur Acad Dermatol Venereol. 2020;34(11):2574–2583.
- Stacey D, Legare F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4(4):CD001431.
- van der Kraaij GE, van Huizen AM, Baerveldt EM, et al. Online decision aid for patients with psoriasis. Br J Dermatol. 2021;184(5):981–983.
- Tan J, Linos E, Sendelweck MA, et al. Shared decision making and patient decision aids in dermatology. Br J Dermatol. 2016;175(5):1045–1048.
- van Winden MEC, Klösters FM, Hamaker M, et al. Optimizing shared decision making in older adults with basal cell carcinoma: experiences from a specialized outpatient clinic. Br J Dermatol. 2022;186(3):589–591.
- Cochrane. Non-randomised controlled study (NRS) designs; 2019. Available from: https://childhoodcancer.cochrane.org/non-randomised-controlled-study-nrs-designs
- Barr PJ, O'Malley AJ, Tsulukidze M, et al. The psychometric properties of observer OPTION(5), an observer measure of shared decision making. Patient Educ Couns. 2015;98(8):970–976.
- Rodenburg-Vandenbussche S, Pieterse AH, Kroonenberg PM, et al. Dutch translation and psychometric testing of the 9-Item shared decision making questionnaire (SDM-Q-9) and shared decision making Questionnaire-Physician version (SDM-Q-Doc) in primary and secondary care. PLoS One. 2015;10(7):e0132158.
- Barr PJ, Forcino RC, Thompson R, et al. Evaluating CollaboRATE in a clinical setting: analysis of mode effects on scores, response rates and costs of data collection. BMJ Open. 2017;7(3):e014681.
- O'Connor AM. Validation of a decisional conflict scale. Med Decis Making. 1995;15(1):25–30.
- Stubenrouch FE, Mus EMK, Lut JW, et al. The current level of shared decision-making in anesthesiology: an exploratory study. BMC Anesthesiol. 2017;17(1):95.
- Larsen MH, Hagen KB, Krogstad AL, et al. Shared decision making in psoriasis: a systematic review of quantitative and qualitative studies. Am J Clin Dermatol. 2019;20(1):13–29.

