Dear Editor,
Granuloma annulare (GA) is an inflammatory granulomatous skin disease of unknown etiology, which can be localized or disseminated. Current treatments include topical and intralesional corticosteroids, dapsone, hydroxychloroquine, methotrexate, pentoxifylline, and sulphasalazine, etc. We present a case of generalized GA resistant to conventional therapy with marked improvement following treatment with dupilumab.
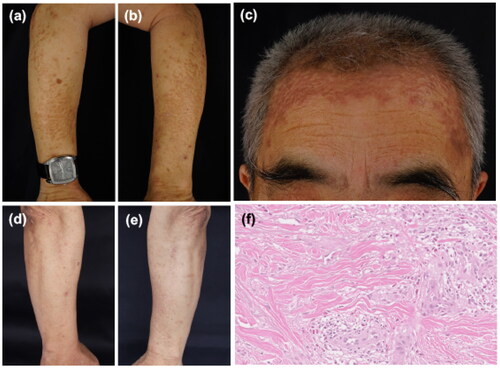
The patient presented with a 10-month history of a gradually worsening eruption with moderate itching. Physical examination found multiple brown-yellow papules and plaques over his trunk and limbs (), which felt firm on palpation. The skin biopsy from his forearm showed palisade-like granulomas in the dermis, accompanied by eosinophil infiltration (). The histopathology led to the diagnosis of GA. Previous treatments included ultrapotent topical steroids, benvitimod cream, oral antihistinames, oral compound glycyrrhizin, isotretinoin, NB-UVB therapy and intramuscular injection of compound betamethasone, but all failed. He had a 20-year history of type 2 diabetes, with good glycemic control on oral hypoglycemic drugs. He did not have any associated atopy medical history. Considering the eosinophil infiltration in his pathology and the potential role of Th2 inflammation in GA (Citation1), the off-label treatment with dupilumab was prescribed with his consent, according to the approved dosage of initially 600 mg followed by 300 mg every other week, applied subcutaneously. He reported a significant improvement of itching, with itching numeric rating scale dropped from 7 (before treatment) to 2 (four days after the first injection), then to 0 (4 weeks after treatment). The skin lesions were flattened two weeks after the first administration (), and continued improving in the 16 weeks of follow-up, with good tolerability.
Figure 1. (a–c) Clinical presentation before treatment. Yellow-red papules and plaques on the forearms and on the forehead. (d,e) A clinical picture on the forearms after 2 weeks of treatment. (f) Histological analysis from the left forearm with hematoxylin and eosin staining (×200) showed palisade-like granulomas in the dermis, accompanied by eosinophil infiltration.
Dupilumab is a monoclonal antibody targeting the Interleukin 4 receptor alpha chain (IL-4Rα) and inhibiting IL-4R signaling. As GA is an inflammatory granulomatous skin disease, macrophage polarization plays an important role in its pathogenesis (Citation2), with an infiltration of M1 macrophages for pro-inflammation at the early stage and polarization to M2 macrophages for promoting tissue regeneration at the late stage. Macrophages could be induced to a M2 phenotype by IL-4 and IL-13. In addition, a retrospective series including 47 pediatric patients with GA (Citation3) and a recent case-control study (Citation4) found a potential association of GA with atopy. A study on the molecular phenotype of GA found significant upregulations in TNF-a and IFN-γ, IL-4, and JAK3, in which IL-4 showed a particularly pronounced increase (15,600-fold) in GA lesional skin versus control skin (Citation1).
The main inflammation type of GA is more likely a mixed pattern. Cases of GA successfully treated with or paradoxically induced by TNF-a inhibitors were reported. Similarly, the relationship between GA and dupilumab was interesting, with one case successfully treated with dupilumab (Citation5) and one case induced by dupilumab (Citation6).
Although limited, the encouraging effect of dupilumab in refractory generalized GA clinically confirmed the role of Th2 inflammation in GA and provided a new potential treatment option for GA. The case suggested itch or pathological eosinophil infiltration may be predictors for good response. However, further studies are warranted to confirm its efficacy and predictors.
Consent form
The authors confirm written informed consent from the patients for the use of image and publication of their case details has been given, regarding their privacy.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings are available from the corresponding author, Aiping Wang, upon reasonable request.
Additional information
Funding
References
- Min MS, Wu J, He H, et al. Granuloma annulare skin profile shows activation of T-helper cell type 1, T-helper cell type 2, and janus kinase pathways. J Am Acad Dermatol. 2020;83:63–70.
- Asai J. What is new in the histogenesis of granulomatous skin diseases? J Dermatol. 2017;44:297–303.
- Cruz SA, Stein SL. The clinical presentation and comorbidities associated with granuloma annulare in the pediatric population: a retrospective study. Skinmed. 2022;20:24–28.
- Joshi TP, Chen V, Dong JL, et al. Atopic comorbidities associated with granuloma annulare: a Case-Control study in the all of Us database. J Am Acad Dermatol. 2023. DOI:10.1016/j.jaad.2023.02.012
- Song EJ, Bezecny J, Farrer S. Recalcitrant generalized granuloma annulare treated successfully with dupilumab. JAAD Case Rep. 2021;7:1–2.
- Phelps-Polirer K, Alkhatib BL, Davis C. Generalized granuloma annulare associated with dupilumab therapy. Cureus. 2022;14:e27439.

