Dear Editor,
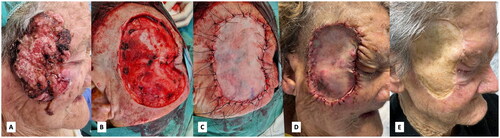
An 88-year-old woman with a history of chronic sun exposure consulted for a fast-growing exophytic friable tumor in the right zygomatic region, with a well-defined border, on which no treatment had been applied. Due to delay in consultation, the lesion had progressively reached a size of 8.9 × 5.7 cm, growing centrifugally toward the ipsilateral temple, malar, and periocular areas without compromising the eyelids. She did not have any other comorbidities. The clinical diagnosis of squamous cell carcinoma was established, and after an extension study, surgery under general anesthesia was scheduled. Removal with safety margins of such a lesion on the face and the consequent reconstruction of the secondary defect represent a surgical challenge that requires thoughtful planning. In our patient, we decided to repair the defect with a full-thickness dermo-epidermal graft to avoid, first, requiring multiple flaps to cover the defect and, second, potential complications in case of incomplete removal and the undesirable need of a second intervention. The patient evolved favorably with complete engraftment without complications and preserving full functionality (). The histopathological study confirmed the diagnosis of infiltrating Squamous Cell Carcinoma (SCC), poorly differentiated, with a thickness of 14.4 mm, lymphovascular invasion in the absence of perineural invasion, and with lesion-free resection margins. Given these characteristics, adjuvant radiotherapy was offered but the patient refused any further treatment. She is currently under periodic clinical and echography follow-ups with no signs of recurrency.
Figure 1. Clinical evolution with surgery: (A) aspect at diagnosis; (B) wide resection with safety margins; (C) Graft implantation; (D) One week after surgery; (E) Seven months after surgery.
Squamous cell carcinoma is the second most frequent skin cancer, and in the recent years, its global incidence has been increasing. Regarding its etiopathogenesis, among other factors, we must highlight the influence of ultraviolet radiation and chronic photoaging [Citation1]. Delays in diagnoses and treatments, like those consequence of the SARS-CoV-2 pandemic in almost all areas of Medicine including Dermato-oncology, lead to worse outcomes [Citation2,3]. Some of the high-risk factors for SCC according to the international guidelines include a size greater than 2 cm, location in the temple, poor differentiation, and thickness greater than 6 mm [Citation4,Citation5]. These factors, as well as the degree of resection achievable by surgery, condition the prognosis and the need for adjuvant therapy [Citation6]. Upon diagnosis of a high-risk SCC, physical examination should include total body skin examination, palpation of lymph nodes and radiologic imaging techniques such as ultrasound of regional lymph nodes, or broader studies like MRI, CT or PET-CT.
Ethical approval
Written informed consent was obtained from the patient for publication of his case details.
Acknowledgment
This article has no funding source.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings are available from the corresponding author, RRV, upon reasonable request. The corresponding author had full access to all the data in this manuscript and takes responsibility for the integrity of the data.
Additional information
Funding
References
- Dessinioti C, Stratigos AJ. Overview of guideline recommendations for the management of high-risk and advanced cutaneous squamous cell carcinoma. Acad Dermatol Venereol. 2022;36(S1):1–2.
- Stratigos AJ, Garbe C, Dessinioti C, European Dermatology Forum (EDF), the European Association of Dermato-Oncology (EADO) and the European Organization for Research and Treatment of Cancer (EORTC), et al. European interdisciplinary guideline on invasive squamous cell carcinoma of the skin: part 1. epidemiology, diagnostics and prevention. Eur J Cancer. 2020;128:60–82.
- Stratigos AJ, Garbe C, Dessinioti C, European Dermatology Forum (EDF), the European Association of Dermato-Oncology (EADO) and the European Organization for Research and Treatment of Cancer (EORTC), et al. European interdisciplinary guideline on invasive squamous cell carcinoma of the skin: part 2. treatment. Eur J Cancer. 2020;128:83–102.
- Kim JYS, Kozlow JH, Mittal B, Invited Reviewers, et al. Guidelines of care for the management of cutaneous squamous cell carcinoma. J Am Acad Dermatol. 2018;78(3):560–578.
- Heppt MV, Steeb T, Berking C, et al. Comparison of guidelines for the management of patients with high-risk and advanced cutaneous squamous cell carcinoma – a systematic review. J Eur Acad Dermatol Venereol. 2019;33(S8):25–32.
- Stratigos A, Garbe C, Lebbe C, European Organization for Research and Treatment of Cancer (EORTC), et al. Diagnosis and treatment of invasive squamous cell carcinoma of the skin: european consensus-based interdisciplinary guideline. Eur J Cancer. 2015;51(14):1989–2007.

