Abstract
Background and Objectives
Hypertrophic scarring is a complex process, and numerous methods have been introduced to treat scars. This study aims to evaluate the effect of combined CO2 fractional laser and narrowband intense pulsed light (IPL) compared to IPL alone in the treatment of hypertrophic scars.
Materials and Methods
This was a prospective, randomized controlled study enrolled 138 patients with hypertrophic scars. The participants were randomly divided into two groups: CO2-IPL and IPL group, and received three sessions at 10–14-week intervals for 3-month follow-up. Two independent plastic surgeons evaluated the treatments using the Patient and Observer Scar Assessment Scales (POSAS). Overall satisfaction was evaluated using the Patient Satisfaction Scale (PSS).
Results
101 subjects completed the study. Compared to single IPL, the combination CO2-IPL group showed a significant improvement in itching, color, stiffness, thickness, and irregularity, except for pain, and an enhancement in vascularization, pigmentation, thickness, relief, and pliability of the scar, assessed by POSAS (p < .01). 100% patients in the combination group were satisfied compared to 84% in IPL alone.
Conclusion
The combination of CO2 fractional laser and narrowband IPL efficiently improved the appearance and profile of hypertrophic scars, offering a comprehensive and reliable approach for scar therapy.
Introduction
Skin wound healing involves a series of pathophysiological processes that defend against harmful injuries, protect against infection, and maintain skin integrity. Typically, normal wound healing occurs in three stages: inflammation, proliferation, and remodeling (Citation1). However, when the injury affects the dermis or deep tissues, it can trigger an abnormal inflammatory response, increased vessel density, excessive collagen deposition, and ultimately result in pathological scars such as hypertrophic scars (HTS) and keloid (Citation2,Citation3). In the clinical setting, HTS is often caused by burns, surgery, trauma, infection, and other severe skin diseases. It tends to be restricted to the margins of the initial wound, unlike keloid. HTS can present with clinical symptoms such as pain, itching, redness, thickness, stiffness, and poor appearance, even leading to deformity and dysfunction, which can result in physiological and psychological issues (Citation4).
Various therapeutic methods have been extensively utilized for hypertrophic scars, including silicone gel sheeting, pressure garments, intralesional corticosteroid injections, cryotherapy, surgery and photoelectric therapy (Citation5). While surgery can resolve joint contractures and reduce scar tension, it is ineffective for addressing itching, erythema, and unsightly appearance. Pressure therapy is also challenging to apply to certain body parts, such as the neck and face. Additionally, other methods have drawbacks, including low efficacy, dyspigmentation, and high recurrence rates. Photoelectric therapy has rapidly developed and has been proven effective for hypertrophic scars, with minimal invasiveness and excellent outcomes (Citation6).
In photoelectric technology, laser therapy has been used for the treatment of hypertrophic scars for decades, based on the principle of photothermolysis. The CO2 laser was initially invented for this purpose, but it was found to cause high rates of pigmentation, erythema and burning. In 2006, the revolutionary concept of fractional laser therapy was introduced, whereby microscopic thermal treatment zones (MTZs) are created and surrounded by untreated tissue, in order to stimulate collagen remodeling and regeneration of skin tissue (Citation7). Nowadays, ablative fractional CO2 laser treatment has been found to be highly beneficial and safe for the treatment of hypertrophic scars (Citation8–10). Compared to laser, the intense pulsed light (IPL) is a non-coherent broadband light with the spectrum between 400–1200 nm. IPL system has high versatile conditions based on specific targets with various parameters such as wavelength, pulse width and interval time (Citation11). Narrowband IPL, evolved from IPL, λ = 500–600 nm, can be effectively absorbed by hemoglobin because of 542 and 577 nm oxyhemoglobin absorption peaks with minimized skin damage. Narrowband IPL system has numerous applications including vascular malformations, acne vulgaris, rejuvenation, sensitive skin, melasma, telangiectasias and hypertrophic scars. Recent studies have reported that narrowband IPL can improve hypertrophic scars on itching, erythema, and suppress scar excessive proliferation (Citation12,Citation13).
Although photoelectric technologies, such as ablative fractional CO2 laser and narrowband IPL, have shown promise in the treatment of hypertrophic scars, past studies have provided limited comparisons between combination therapy and single therapy. As a result, we have designed a prospective, randomized controlled trial to evaluate the efficacy and safety of combined CO2-IPL versus single IPL.
Materials and methods
Study design
This was a prospective, observer-blinded, randomized controlled study. It was approved by the Ethic Board of Shanghai Ninth People’s Hospital, Shanghai Jiaotong University of Medicine, China (2017-343-T252) and registered at Chinese Clinical Trial Registry (ChiCTR-ONH-17012350). Informed consents were obtained from all patients before enrollment.
Patients
From August 2017 to January 2021, a total of 138 patients with hypertrophic scars were recruited for this study from the Department of Plastic and Reconstructive Surgery, Shanghai Ninth People’s Hospital. The inclusion criteria were patients aged between 16 and 55 with Fitzpatrick skin types II-IV who developed hypertrophic scars due to burns, surgeries, or trauma that were at least 2 cm in length and had been present for over 8 weeks. Exclusion criteria included pregnancy and lactation, patients diagnosed with keloids, serious skin disorders, or systemic diseases, as well as those who had undergone laser, intralesional treatment, or dermabrasion for hypertrophic scars in the past 3 months. To randomly assign patients to either the CO2-IPL group or the IPL group, A or B were generated through a computer-generated process prior to the study.
Treatment
Each patient received three sessions with intervals of 10-14 weeks and a follow-up of 3 months. Prior to therapy, each patient’s scar area was cleaned with 70% alcohol and dried using sterile gauzes. The same photographer took photos of the patients before each session and again 3 months after the final session in fixed position and lighting, using a digital camera (D750, Nikon, Japan) and the VISIA Skin Analysis System (Canfield Scientific, USA). During photoelectric treatment, physicians should wear specialized glasses and ensure that patients’ eyes are protected.
For narrowband IPL therapy, 2–3 mm of ultrasound gel was evenly applied to the scar surface. The area was then irradiated using a commercial IPL (λ = 500–600 nm, spot size = 3 cm2, fluence = 6–8 J/cm2, pulse width = 12 ms, 2 passes) (Alma Laser, Caesarea, Israel). For CO2-IPL therapy, a topical anesthetic cream (Compound Lidocaine Cream, Beijing Ziguang, China) was applied to the scar and occluded for 30–60 min. The cream was then removed and the IPL treatment was conducted according to the above protocol. Next, the clinician used the Ultrapulsed Fractional CO2 Laser (Deep FX mode, Lumenis, Santa Clara, CA, USA) with a parameter of 17.5–25 mJ/cm2 for one pass at a density of 5%. The endpoint was determined by the appearance of thermal ablation, mild erythema, and edema. To avoid bias, patients in both groups applied ice bags to the scar area for 20–30 min to reduce thermal damage. Following the procedure, antibacterial ointment and moisturizer were applied topically twice a day for one week. The treated region was instructed to remain sterile, and patients were advised to avoid intense exercise and saunas for one week. Additionally, patients were instructed to protect themselves from the sun during the entire therapy by wearing protective clothing, hats, and using sunscreen cream.
Clinical Assessment
The Patient and Observer Scar Assessment Scales (POSAS) are a reliable and feasible scar evaluation scale that have been modified from the Vancouver Scar Scale. The scale comprises a combination of a patient scale and an observer scale, with the former assessing pain, itching, color, stiffness, thickness, and irregularity. The observer scale reflects vascularization, pigmentation, thickness, relief, and pliability. Each characteristic is scored on a scale of 1–10, with one representing normal skin and ten indicating the worst possible situation. Before each treatment and three months after the last session, two independent plastic surgeons assessed each characteristic of the POSAS. Additionally, overall satisfaction was assessed by Patient Satisfaction Scale (PSS) with the range of 1 (very satisfied), 2 (satisfied), 3 (unsatisfied) and 4 (very unsatisfied) after the follow-up.
Statistical Analysis
The statistical software (SPSS version 24.0, IBM, Chicago, USA) was used for performing the statistical analyses. The paired Student’s t-test was used to analyze significant changes between baseline and follow-up, whereas the non-parametric Mann-Whitney test was used to compare statistical differences between two groups for demographic data (age, scar duration), POSAS scores, and PSS scores. Pearson’s chi-square test was used for other characteristics of patients (gender, scar location, scar source). A statistically significant difference was defined as p < .05 at a 95% confidence level.
Results
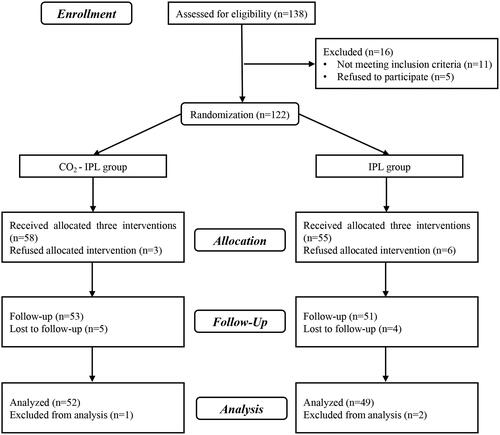
The consort flow chart is illustrated in . Out of the 138 patients who were recruited, a total of 122 patients with hypertrophic scars were randomized into either the CO2-IPL group or the IPL group. Ultimately, a total of 101 participants (43 male and 58 female) successfully completed the study. Nine patients were unable to complete the three interventions while another nine were lost to follow-up due to scheduling conflicts or other reasons. The age range of the patients was between 16 and 52 years old with a mean scar duration of 6.4 months (ranging from 2–15 months). The hypertrophic scars were located on the face (30.7%), neck (11.9%), trunk (19.8%), and extremities (37.6%). The majority of scars were caused by burns (57.4%), while others resulted from surgery (34.7%) and trauma (7.9%). No significant differences were observed between the CO2-IPL and IPL groups in terms of gender, scar duration, scar location, and source (p < .05) ().
Table 1. Characteristics of patients and hypertrophic scars (n = 101).
The POSAS scores from clinical assessments were measured after photoelectric therapy and are presented in . At 3 months after three sessions, the total POSAS scores were significantly lower in the CO2-IPL group (38.58 ± 4.71) compared to the IPL group (44.04 ± 5.07) (p < .0001). Both PSAS and OSAS scores showed significant improvement in the CO2-IPL group compared to the IPL group. For PSAS, improvements in itching, color, stiffness, thickness, and irregularity were significantly greater in the CO2-IPL group than in the IPL group (p < .01), except for pain (p = .4205). In the OSAS, significant differences were observed in vascularization, pigmentation, thickness, relief, and pliability after CO2-IPL treatment compared to IPL intervention (p < .01).
Table 2. Comparison of POSAS scores before and after treatment.
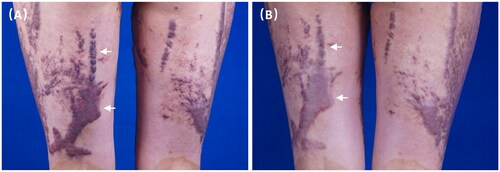
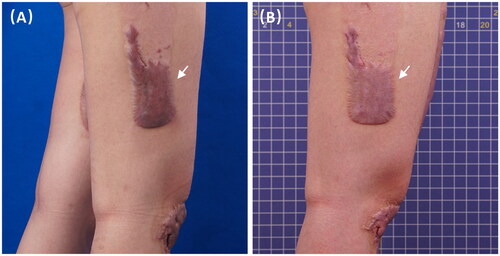
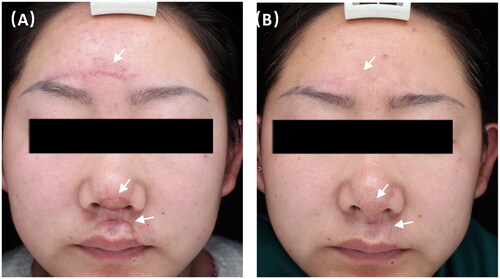
At the final follow-up of the study, the patients were told to provide satisfaction scale scores based on their previous therapy. Results from the CO2-IPL group showed that 28 patients (54%) were very satisfied with the combined phototherapy, while 24 patients (46%) were satisfied. No patients were unsatisfied or very unsatisfied. In the IPL group, 41 patients (84%) reported being satisfied, while 8 patients (16%) expressed dissatisfaction due to insufficient changes in texture, thickness, and stiffness of their skin. The patient satisfaction rate was significantly higher in the combined CO2-IPL therapy group compared to the single IPL group (p < .05). No severe side effects were observed during the application of CO2 and IPL. Mild erythema may occur for about three days after CO2-IPL therapy, and post-inflammatory hyperpigmentation was uncommon. Clinical responses of representative patients were presented in , which clearly showed that CO2-IPL therapy significantly improved skin thickness, stiffness, pliability, and color due to photothermolysis, compared to single IPL treatment.
Figure 2. A 21-year-old burn female with hypertrophic scars on lower limbs received three CO2-IPL treatments showing marked improvement in color, thickness and texture.
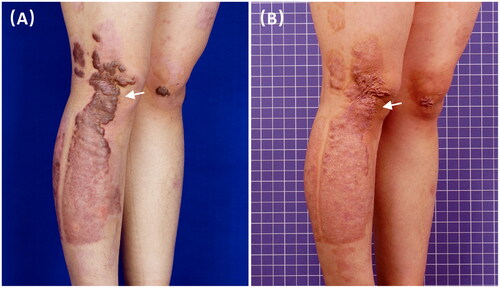
Figure 3. A 26-year-old burn male with hypertrophic scars on face at (A) baseline and (B) 3 months after three CO2-IPL treatments showing great improvement in vascularization, pliability and thickness.
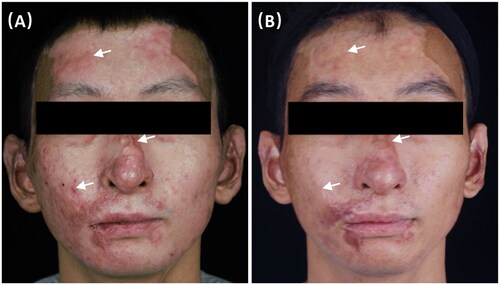
Figure 4. A 28-year-old female with hypertrophic scars from surgery on face at (A) baseline and (B) 3 months after three CO2-IPL treatments showing excellent improvement in thickness, color, stiffness and texture.
Discussion
This study was a prospective, randomized controlled trial that aimed to assess the efficacy and safety of combined CO2-IPL and single light IPL in treating hypertrophic scars. The clinical curative effect was evaluated using POSAS, and patient satisfaction was assessed using PSS. In comparison to single IPL, the combined CO2-IPL treatment demonstrated lower POSAS scores. Independent observers found the combined treatment to be more effective in terms of vascularization, pigmentation, thickness, relief, and pliability, while patients reported reduced pruritus, lighter color, thinner scars, and more regular shape. Moreover, 100% of patients in the CO2-IPL group expressed satisfaction with the treatment outcome. Of the satisfied group, 54% were very satisfied and wished to continue follow-up treatment. The IPL group obtained an overall satisfaction rate of 84%, but none were very satisfied with the therapy. Furthermore, 16% expressed dissatisfaction with the scar improvement.
Although the exact mechanism behind the formation of hypertrophic scars (HTS) is not fully understood, it is widely believed that trauma triggers the degranulation of platelets, activation of vascular endothelial cells (EC), and increased vascular permeability. This leads to the aggregation of immune cells, inflammatory waterfall, and neovascularization. Inflammatory cytokines stimulate fibroblasts to over-proliferate and transform into myofibroblasts, which express α smooth muscle actin (α-SMA), secrete collagen, and promote the deposition of extracellular matrix, scar growth, and contracture (Citation14,Citation15). As a result, microvasculature and collagen play crucial roles in HTS formation, which is characterized by two important clinical features: redness and thickening. Therefore, targeting microvasculature and collagen is pivotal in the prevention and treatment of HTS (Citation16).
Gradually, laser and light therapy are becoming central to the field. Photoelectric treatments are minimally invasive or noninvasive, less painful, and have excellent therapeutic efficacy with short downtime and rare side effects. They can be applied to a large area in a single session. The methods are most commonly used to destroy local vessels and reduce blood supply by targeting oxyhemoglobin, including IPL (400–1200nm) and Pulsed Dye Laser (PDL) (585 nm or 595 nm). To successfully close blood vessels, it is required that the pulse duration is shorter than the heat relaxation time of hemoglobin (Citation17).
IPL is a non-laser light source that targets both oxyhemoglobin and melanin, delivering low-level light to the epidermis and dermis layers. IPL can simultaneously coagulate microvasculature, eliminate melanin, and stimulate collagen regeneration. The researches had shown that IPL irradiation can promote fibroblast proliferation and increase the expression levels of procollagen I and III mRNA without affecting the levels of vascular endothelial growth factor (VEGF) and matrix metalloproteinases (MMP) (Citation18,Citation19). In one study, 109 patients with hypertrophic scars underwent eight IPL treatment sessions, and 92.5% of patients showed significant improvement in scar height, erythema, and hardness (Citation20). Previous studies have demonstrated IPL’s excellent effects on the pliability and pigmentation of surgical and traumatic scars. Importantly, IPL is suitable for almost all skin types, including darker skin, and can be combined with other therapies (Citation21,Citation22). PDL is capable of targeting oxyhemoglobin and coagulating microvessels, making it effective in the treatment of port wine stains and other hemangiomas. Additionally, it can decrease collagen III deposition and reduce the thickness, pigmentation, and vascularity of scar tissue (Citation23). However, in this study, we opted to use narrowband IPL instead of PDL to target scar vessels. PDL treatment often results in purpura, which can cause new injury to the thin scar skin and trigger excessive inflammatory reactions, neovascularization, and even new scarring. Moreover, PDL has a smaller hand tool spot size (15 mm), while the larger 3 × 1 cm footprint of IPL is better suited for treating large areas of hypertrophic scars. Narrowband IPL (500–600 nm) is filtered from IPL and effectively targets erythema and melanin without harming the epidermis, making it a safer choice for darker skin types with minimal downtime (Citation24,Citation25).
Based on fractional photothermolysis, the fractional CO2 laser (10600 nm) creates less than 500 μ MTZs surrounded by remaining skin tissue, which allows for rapid repair without new scarring. The CO2 laser can be absorbed by water and penetrate deeper into the skin with high energy, causing skin vaporization and collagen denaturation (Citation26,Citation27). Burn scars have been treated with fractional CO2 laser and studies have shown molecular changes, including increased collagen III, TGF-β3, and MMP-1, as well as reduced collagen I (Citation28,Citation29). In 2017, Julian treated ten patients with hypertrophic burn scars using fractional CO2 laser. After six months of treatment, it was observed that surface relief improved, the firmness of scars decreased, and the Vancouver Scar Scale (VSS) and POSAS scores showed significant improvement (Citation30). Additionally, the authors proved that the texture and color of hypertrophic post-burn scars improved noticeably after fractional CO2 laser treatment. No scarring or dyspigmentation was reported (Citation31).
In this study, fractional CO2 laser and narrowband IPL were selected for the treatment of hypertrophic scars. The combined CO2-IPL therapy demonstrated significant improvement in overall scar assessment, as compared to IPL therapy alone, according to the POSAS evaluation. This improvement in scars was due primarily to the photothermolysis of tissue collagen by fractional CO2, rather than narrowband IPL targeting scar vessels. No serious side effects were noted from the combination therapy. Results showed that the combination CO2-IPL therapy had a higher potential for benefits, with shorter treatment sessions than single IPL therapy. In a separate randomized controlled trial, 23 patients with large hypertrophic scars received CO2 ablative fractional laser (AFL) and IPL treatment over four sessions. Compared to control and CO2 laser alone, combined IPL and CO2 AFL resulted in higher improvements, as assessed by Manchester Scar Scale (MSS) and POSAS. This demonstrates the importance of applying multiple phototherapies, including CO2 AFL and IPL, for the effective treatment of hypertrophic scars (Citation32). However, this clinical study had a small sample size and did not have IPL therapy as a control, considering its excellent efficacy on scar vessels. Our study analyzed 101 patients with hypertrophic scars, providing strong evidence for the photoelectric combination therapy as the potential benefits of combination CO2-IPL therapy over IPL alone were demonstrated. Thus, the results emphasize the crucial role of combining phototherapies in the treatment of hypertrophic scars.
Our study has certain limitations. Firstly, it is a single-center study, and to strengthen the level of evidence, a multi-center clinical study involving multiple regions and ethnic groups should be conducted in the future. Secondly, more objective tests such as ultrasound should be applied. However, our study unequivocally demonstrates the efficacy of combination CO2-IPL therapy and offers a dependable approach for treating hypertrophic scars.
Conclusion
The use of a fractional CO2 laser in combination with narrowband IPL has been found to achieve substantial results in the management of hypertrophic scars. This combination offers a safe and dependable alternative for multi-photoelectric therapies.
Disclosure statement
No potential conflict of interest has been reported by the authors.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author upon reasonable request.
Additional information
Funding
References
- Zhang J, Li Y, Bai X, et al. Recent advances in hypertrophic scar. Histol Histopathol. 2018;33(1):1–7.
- Berman B, Maderal A, Raphael B. Keloids and hypertrophic scars: pathophysiology, classification, and treatment. Dermatol Surg. 2017;43(Suppl 1):S3–S18.
- Zhu Z, Ding J, Shankowsky HA, et al. The molecular mechanism of hypertrophic scar. J Cell Commun Signal. 2013;7(4):239–252.
- Chiang RS, Borovikova AA, King K, et al. Current concepts related to hypertrophic scarring in burn injuries. Wound Repair Regen. 2016;24(3):466–477.
- Berman B, Viera MH, Amini S, et al. Prevention and management of hypertrophic scars and keloids after burns in children. J Craniofac Surg. 2008;19(4):989–1006. Jul
- Niwa AB, Mello AP, Torezan LA, et al. Fractional photothermolysis for the treatment of hypertrophic scars: clinical experience of eight cases. Dermatol Surg. 2009;35(5):773–777. discussion 777–8.
- Laubach HJ, Tannous Z, Anderson RR, et al. Skin responses to fractional photothermolysis. Lasers Surg Med. 2006;38(2):142–149. Feb
- Blome-Eberwein S, Gogal C, Weiss MJ, et al. Prospective evaluation of fractional CO2 laser treatment of mature burn scars. J Burn Care Res. 2016;37(6):379–387. Nov/Dec
- Douglas H, Lynch J, Harms KA, et al. Carbon dioxide laser treatment in burn-related scarring: a prospective randomised controlled trial. J Plast Reconstr Aesthet Surg. 2019;72(6):863–870. Jun
- Clayton NA, Haertsch PA, Maitz PK, et al. Ablative fractional resurfacing in acute care management of facial burns: a new approach to minimize the need for acute surgical reconstruction. J Burn Care Res. 2019;40(3):368–372.
- Ash C, Town G, Whittall R, et al. Lasers and intense pulsed light (IPL) association with cancerous lesions. Lasers Med Sci. 2017;32(8):1927–1933.
- Klein A, Baumler W, Landthaler M, et al. Laser and IPL treatment of port-wine stains: therapy options, limitations, and practical aspects. Lasers Med Sci. 2011;26(6):845–859. Nov
- Gonzalez-Rodriguez AJ, Lorente-Gual R. Current indications and new applications of intense pulsed light. Actas Dermosifiliogr. 2015;106(5):350–364.
- Karppinen SM, Heljasvaara R, Gullberg D, et al. Toward understanding scarless skin wound healing and pathological scarring. F1000Res. 2019;8:787.
- Ogawa R, Akaishi S. Endothelial dysfunction may play a key role in keloid and hypertrophic scar pathogenesis - Keloids and hypertrophic scars may be vascular disorders. Med Hypotheses. 2016;96:51–60.
- Yuan B, Upton Z, Leavesley D, et al. Vascular and collagen target: a rational approach to hypertrophic scar management. Adv Wound Care. 2023;12(1):38–55. Jan
- Oliaei S, Nelson JS, Fitzpatrick R, et al. Laser treatment of scars. Facial Plast Surg. 2012;28(5):518–524.
- Wu D, Zhou B, Xu Y, et al. Impact of intense pulsed light irradiation on cultured primary fibroblasts and a vascular endothelial cell line. Exp Ther Med. 2012;4(4):669–674. Oct
- Cao Y, Huo R, Feng Y, et al. Effects of intense pulsed light on the biological properties and ultrastructure of skin dermal fibroblasts: potential roles in photoaging. Photomed Laser Surg. 2011;29(5):327–332.
- Erol OO, Gurlek A, Agaoglu G, et al. Treatment of hypertrophic scars and keloids using intense pulsed light (IPL). Aesthetic Plast Surg. 2008;32(6):902–909.
- Bellew SG, Weiss MA, Weiss RA. Comparison of intense pulsed light to 595-nm long-pulsed pulsed dye laser for treatment of hypertrophic surgical scars: a pilot study. J Drugs Dermatol. 2005;4(4):448–452.
- Cartier H. Use of intense pulsed light in the treatment of scars. J Cosmet Dermatol. 2005;4(1):34–40.
- Alster TS. Improvement of erythematous and hypertrophic scars by the 585-nm flashlamp-pumped pulsed dye laser. Ann Plast Surg. 1994;32(2):186–190.
- Moy WJ, Yakel JD, Osorio OC, et al. Targeted narrowband intense pulsed light on cutaneous vasculature. Lasers Surg Med. 2015;47(8):651–657. Oct
- Alberdi E, Gomez C. Efficiency of methylene blue-mediated photodynamic therapy vs intense pulsed light in the treatment of onychomycosis in the toenails. Photodermatol Photoimmunol Photomed. 2019;35(2):69–77.
- Manstein D, Herron GS, Sink RK, et al. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34(5):426–438.
- Jih MH, Kimyai-Asadi A. Fractional photothermolysis: a review and update. Semin Cutan Med Surg. 2008;27(1):63–71.
- Ozog DM, Liu A, Chaffins ML, et al. Evaluation of clinical results, histological architecture, and collagen expression following treatment of mature burn scars with a fractional carbon dioxide laser. JAMA Dermatol. 2013;149(1):50–57.
- Qu L, Liu A, Zhou L, et al. Clinical and molecular effects on mature burn scars after treatment with a fractional CO(2) laser. Lasers Surg Med. 2012;44(7):517–524.
- Poetschke J, Dornseifer U, Clementoni MT, et al. Ultrapulsed fractional ablative carbon dioxide laser treatment of hypertrophic burn scars: evaluation of an in-patient controlled, standardized treatment approach. Lasers Med Sci. 2017;32(5):1031–1040.
- Haedersdal M. Fractional ablative CO(2) laser resurfacing improves a thermal burn scar. J Eur Acad Dermatol Venereol. 2009;23(11):1340–1341.
- Daoud AA, Gianatasio C, Rudnick A, et al. Efficacy of combined intense pulsed light (IPL) with fractional CO(2) -Laser ablation in the treatment of large hypertrophic scars: a prospective, randomized control trial. Lasers Surg Med. 2019;51(8):678–685.