Abstract
Purpose: Onychopapilloma is a rare benign nail tumor affecting the distal matrix and the nail bed. Currently, the only available treatment is surgical resection, which has a recurrence rate of 20% and may lead to various complications. Here we report a new method to treat onychopapilloma with pulsed dye laser (PDL).
Materials and methods: We retrospectively analyzed 13 cases and evaluated disease classification, dermoscopic examination, laser treatment parameters, photographs before and after treatment, and treatment outcome.
Results: The site distribution of onychopapilloma was consistent with previous reports. PDL treatment was performed with 595 nm laser, with 1.5 ms pulse duration, spot diameter 3–5 mm, and 11.5–13.5 J/cm2 fluence. Irradiation covered the telangiectatic area up to the edge of the nail folds, with the terminal response of purpura occurrence. The overall effective rate was 77%; the effective rates for erythronychia, leukonychia, and melanonychia were 88%, 67%, and 50%, respectively.
Conclusions: PDL treatment for onychopapilloma provides an alternative to traditional surgery with comparable effectiveness but much less risk for complications.
Introduction
Onychopapilloma is a rare benign nail tumor affecting the distal matrix and the nail bed (Citation1,Citation2). It presents variously as longitudinal erythronychia (the most common), longitudinal leukonychia, longitudinal melanonychia, splinter hemorrhages, distal fissuring, subungual ketatotic mass, onycholysis, and other rare conditions (Citation1–8). Since it was first reported in 1995 (Citation1), there has been approximately 20 reports of 222 cases in the literature (Citation5). Most patients seek medical attention because of the appearance of malformation and pain in the nail. At present, surgical resection is the only treatment for onychopapilloma. However, it has a recurrence rate of 20% (Citation4), with complications including intraoperative and postoperative pain, long recovery period, and poor post-surgical appearance.
Dermoscopic examination reveals telangiectasia in the proximal nail folds with onychopapilloma. As pulsed dye laser (PDL) can eliminate abnormal capillaries by photothermolysis (Citation9,Citation10), we tested PDL as a treatment of onychopapilloma. Here we retrospectively examine 13 cases of onychopapilloma treated with PDL at our hospital.
Methods
This study includes a total of 13 patients diagnosed with onychopapilloma at Xijing Hospital from November 2016 to October 2021, who refused surgical treatment and consented to receive PDL treatment instead. We retrospectively analyzed the disease’s characteristics, classification by dermoscopic examination, PDL irradiation settings (Vbeam Perfecta, Candela Corporation, Wayland, MA, USA), and treatment outcome. PDL parameters were: wavelength 595 nm, pulse duration 1.5 ms, spot diameter 3–5 mm, and energy fluence 11.5–13.5 J/cm2. Treatment outcome was assessed by pre- and post-treatment photographs, Visual Analogue Scale (VAS) scores, and patients’ subjective feeling.
Results
13 patients presented with pain or tenderness in the affected areas. Among them, seven reported difficulty in picking up objects, and two presented with no subjective symptom. Dermoscopic examination showed histological characteristics consistent with onychopapilloma. There were continuous red, white, or dark streaks from the nail lunula to the nail edge; the nail edge showed V-shaped peeling, accumulation of keratinoid, or splinter hemorrhages. The age, gender, affected sites, average time from onset, and diagnostic classification of the patients were summarized (). Onychopapilloma occurred on the hands of 12 patients and on the feet of one patient in this series. The disease mainly started on the first and second fingers/toes (six cases on the first, three cases on the second, and four cases on the third or the fifth fingers). Left hands/feet (8 cases) was affected more frequently than right ones (5 cases).
Table 1. Clinical characteristics of 13 patients with onychopapilloma.
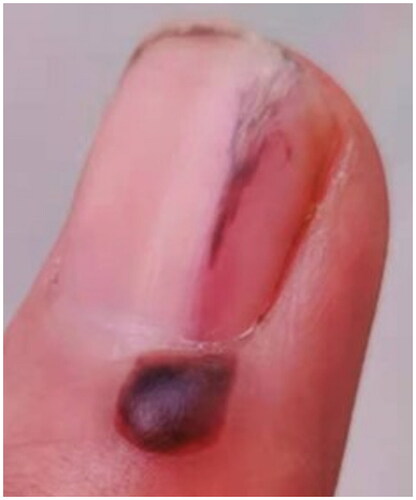
We performed PDL irradiation covering the telangiectatic area of the nail fold up to edge of the affected nail. In each treatment session, the site received one pass of irradiation until an intense purpura occurred (). Usually, the purpura was absorbed and disappeared within a week. Seven cases received one treatment session, three cases two sessions, and three cases more than three sessions, with a one-month interval between sessions. Post-treatment care included immediate ice compress for 20 min, and the patient was instructed to keep the treated limb under rest and to avoid infection.
In patients presented with pain or tenderness, we measured their VAS scores before, during and after PDL treatment, which were respectively 2.1 (range: 1–10), 6.6 (range: 4–10) and 0.4 (range: 0–1). In general, pain was relieved. We followed up patients for six months and up to three years. According to photographs and self-reports, five patients recovered well without recurrence, five showed improvement, and three showed poor outcomes. Interestingly, all cases in which the first or the second fingers/toes were affected achieved cure or improvement, whereas those with other figures affected showed less effectiveness.
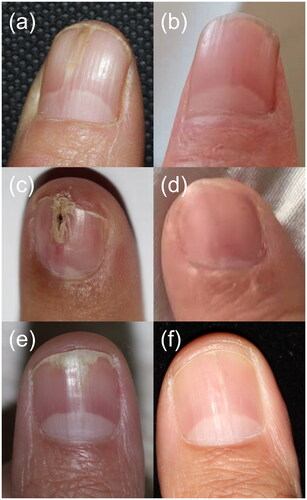
Overall, the effective rate was 77% and the recurrence rate was 23%. Among them, the effective rate for erythronychia was 88%, with a cure rate of 39%; the effective rate for leukonychia was 67%, without any case of cure; the effective rate of melanonychia was 50%, without any case of cure ().
Figure 2. Comparison between pre- and post- PDL irradiation in three typical cases. (a) Case 1, female, 56 years, right thumb, longitudinal erythronychia. (b) Case 1, five years after two sessions of PDL irradiation. (c) Case 2, female, 35 years, left index finger, longitudinal erythronychia with distal fissuring and splinter hemorrhages. (d) Case 2, three years after one session of PDL irradiation. (e) Case 3, female, 24 years, left thumb, longitudinal leukonychia with onycholysis and V-shaped distal notch. (f) Case 3, one year after five sessions of PDL irradiation.
Discussion
Onychopapilloma is usually benign, with only one case of malignant transformation reported in the literature (Citation11). In all cases (>200 patients) reported to date (Citation5), patients received surgical treatment. The age, gender, and affected areas of our patients largely agree with reports in the literature (Citation5). We found that the first and the second fingers showed better outcome, particularly on the right hand. This may be due to the more frequent use of the right hand (the dominant hand of most people), which could lead to higher permeability and larger diameter of the capillaries. Future studies are needed to confirm this phenomenon and to clarify its physiological mechanism.
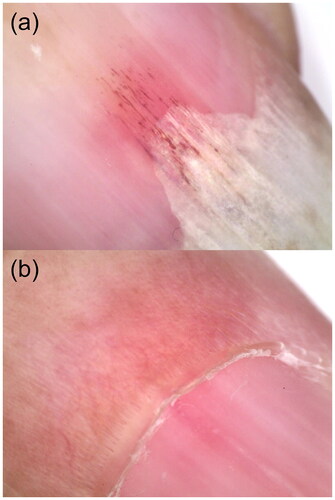
Dermoscopic examination revealed subungual splinter hemorrhages as well as telangiectasia in the nail folds of some patients (). These findings suggest the presence of capillary abnormalities in onychopapilloma. PDL irradiation is effective in superficial capillary malformation, as it is absorbed specifically by erythrocytes (Citation9,Citation10). As PDL can induce rapid coagulation to block the capillaries, it may achieve its therapeutic effect by altering microcirculation. A histopathological examination of nail psoriasis revealed dilated capillaries in the papillary dermis similar to that of onychopapilloma (Citation12). PDL irradiation does not significantly improve nail psoriasis compared to intralesional steroid treatment, and the improvement rate is 22.24% (Citation13). A better understanding of the pathological differences between nail psoriasis and onychopapilloma is required.
Figure 3. Characteristics of dermoscopic examination. (a) Subungual splinter hemorrhages. (b) Telangiectasia at the area of nail folds.
We found that erythronychia responded better to PDL treatments. There are several possible reasons that some patients were not cured. First, nail splinters might be too thick, which attenuated the laser and diminished the treatment effect. Second, the surgeon might have given a sub-optimal level of laser energy to the proximal area of the nail edge due to concerns about adverse effects.
In all patients, PDL treatment obviously mitigated the pain associated with onychopapilloma. The laser treatment itself only induced transient, tolerable pain that lasted a few seconds. The immediate application of an ice compress after the treatment further relieved the pain. Compared to conventional surgery, which involves anesthesia and suture removal and is associated with post-surgical pain, the patient was much less afraid of the pain associated with PDL treatment. Even in patients with unsatisfactory treatment outcome, the VAS score still dropped after the treatment.
After the treatment, the patient was instructed to protect the affected area and to avoid strenuous physical activities for three days; there was no need for bandaging. Thus, the impact on the patient’s normal life is minimal compared to conventional surgery.
No obvious difference is observed between the effectiveness and the recurrence rate of laser treatment and those of surgical treatment. Recurrence after surgical resection may be linked to incomplete excision (Citation4). In this series of cases, the effective rate is 77% and the recurrence rate is 23% overall. However, the effective rate for erythronychia satisfactorily reaches 88%, with a cure rate of 39%. In contrast, the effective rate of leukonychia or melanonychia is low, without any case of cure. Such differences may result from differences in the pathogenesis of these conditions. For example, melanonychia may be due to oxyhemoglobin formed after nail bed hemorrhage, or due to activation of melanocytes. Dermoscopic examination suggests that the treatment of melanonychia caused by bleeding is satisfactory. Future studies are needed to test whether Q-switched laser, often used to treat pigmented disorders, can be used to treat melanonychia with active melanocytes.
Author contributions
Y.L. and B.L. have full access to all data in this study and take responsibility for the integrity of the data and the accuracy of data analysis. X.F., T.L., and X.Z. conceived and designed the study. All authors contributed to data acquisition, analysis, and interpretation. X.F. and Y.L. drafted the manuscript, and all authors contributed to the critical revision of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The authors are unable to provide individual patient data as consent for distribution of personal information was not obtained in the report.
Additional information
Funding
References
- Baran R, Perrin C. Localized multinucleate distal subungual keratosis. Br J Dermatol. 1995;133(1):1–4.
- Baran R, Perrin C. Longitudinal erythronychia with distal subungual keratosis: onychopapilloma of the nail bed and Bowen’s disease. Br J Dermatol. 2000;143(1):132–135.
- Criscione V, Telang G, Jellinek NJ. Onychopapilloma presenting as longitudinal leukonychia. J Am Acad Dermatol. 2010;63(3):541–542.
- Delvaux C, Richert B, Lecerf P, et al. Onychopapillomas: a 68-case series to determine best surgical procedure and histologic sectioning. J Eur Acad Dermatol Venereol. 2018;32(11):2025–2030.
- Starace M, Alessandrini A, Ferrari T, et al. Clinical and onychoscopic features of histopathologically proven onychopapillomas and literature update. J Cutan Pathol. 2022;49(2):147–152.
- Jellinek NJ. Longitudinal erythronychia: suggestions for evaluation and management. J Am Acad Dermatol. 2011;64(1):167.e1–167.e11.
- Miteva M, Fanti PA, Romanelli P, et al. Onychopapilloma presenting as longitudinal melanonychia. J Am Acad Dermatol. 2012;66(6):e242–e243.
- Tosti A, Schneider SL, Ramirez-Quizon MN, et al. Clinical, dermoscopic, and pathologic features of onychopapilloma: a review of 47 cases. J Am Acad Dermatol. 2016;74(3):521–526.
- Iznardo H, Roé E, Puig L, et al. Good response to pulsed dye laser in patients with capillary malformation-arteriovenous malformation syndrome (CM-AVM). Pediatr Dermatol. 2020;37(2):342–344.
- Ang YS, Koh MJA. Treatment of capillary malformations in capillary malformation-arteriovenous malformation syndrome with pulsed dye laser. J Cosmet Dermatol. 2021;20(11):3710–3711.
- Haneke E, Iorizzo M, Gabutti M, et al. Malignant onychopapilloma. J Cutan Pathol. 2021;48(1):174–179.
- Maranda EL, Nguyen AH, Lim VM, et al. Laser and light therapies for the treatment of nail psoriasis. J Eur Acad Dermatol Venereol. 2016;30(8):1278–1284.
- Soliman M, Aal HA, Sadek AM, et al. Pulsed-dye laser versus intralesional steroid in the management of nail psoriasis: a randomized, intra-patient, comparative, controlled study. J Clin Aesthet Dermatol. 2021;14(9):45–49.