Abstract
Purpose
Nail bed atrophy, a common condition for which conservative treatments have limited efficacy, continues to present challenges in determining the optimal surgical intervention. This study introduces a novel technique for nail bed expansion.
Materials and Methods
A total of 34 patients with nail bed atrophy, selected between 2015 and 2020 (ChiCTR2000036232), were randomized into a control group (n = 17) and a surgical group (n = 17). While no specialized treatment was administered to the control group, the surgical group underwent continuous W-shaped incisions on the ventral side of the digits.
Results
Following a 12-month follow-up period, changes in nail bed height, width, area, esthetic satisfaction, pain levels, and tactile sensation were assessed in both groups. In the surgical group, the height, width, and area of the nail bed increased significantly by 1.50 ± 0.49 times, 1.16 ± 0.23 times, and 1.69 ± 0.60 times, respectively, compared to the preoperative measurements. The newly-formed nail plate exhibited improved esthetics, characterized by its smoothness and transparency, a marked improvement over the control group (p < 0.05). Furthermore, this surgical approach showed significant effects, regardless of whether it was applied to fingers or toes.
Conclusion:
The continuous W-shaped incision technique demonstrated substantial benefits and could be a practical therapeutic approach for nail bed enlargement.
Introduction
The concept of nail bed atrophy was first introduced by Samman in 1969 when it was frequently misdiagnosed as lichen planus and even used as a diagnostic marker (Citation1). In 1988, Barth et al. identified histological changes associated with nail bed atrophy, which resembled idiopathic atrophy, and consequently categorized it as a distinct disease entity (Citation1). Nail bed atrophy can arise from several causes, such as nail trauma, radiation dermatitis, infection, and genetic factors, with fungal infection being the most common (Citation2–8).
Conservative treatment for nail bed atrophy is generally considered suboptimal and controversial (Citation9,Citation10). Traditional treatment methods encompass using nail clippers or other tools to trim deformed nails, employing artificial nail plates to redirect the growth of newly formed nail plates, or utilizing abrasive tools to thin and smoothen thickened nails. These methods can be used individually or in combination for optimal results. Additionally, drugs such as trichloroacetic acid can also supplement conservative treatment. However, traditional treatment methods typically require a considerable duration to show significant improvement, necessitating long-term patient adherence. This process can be complex and resource-intensive, concluding that conservative treatment may not be optimal for treating nail bed atrophy.
Surgical treatment typically yields quicker results compared to conservative treatment (Citation11,Citation12). Traditional nail bed enlargement surgery is typically classified into two primary techniques: the U-flap and rectangular skin excision methods. The U-flap method involves making centripetal incisions on both sides of the nail root to form a U-shaped flap of periungual tissue. This flap is partially excised to expose the nail bed, and skin and subcutaneous tissue segments above the nail root are removed to reveal more of the nail bed. Conversely, the rectangular skin excision method necessitates the removal of a rectangular part of the skin and subcutaneous tissue at the base of the nail, aligning the long axis of the rectangle parallel to the nail folds. The rectangular incision is subsequently sutured along its long edge, thereby pulling back the skin and revealing a more significant portion of the nail bed. However, it is crucial to note that with both techniques, the actual surface area of the nail bed remains unchanged; these methods merely expose the portion previously concealed beneath the skin.
In contrast to these traditional surgical methods, flap grafting also presents a viable option for nail bed augmentation. As noted in a study by Jayaletchumi Gunasagaran (Citation11), a patient suffering from a chemical burn-induced nail bed defect underwent repair using a flap graft harvested from the adjacent middle finger. The transplantation operation is deemed complete only after the pedicle of the skin flap is severed in a secondary procedure. Other studies have proposed using a V–Y incision to advance the finger pulp flap as a means of repairing nail bed defects (Citation12). However, despite their ability to cover nail bed defects, these techniques often lead to poor adhesion between the newly formed nail bed and the nail plate, implying that the nail plate cannot adhere closely to the nail bed. To address this issue of nail plate adhesion, Li MW proposed a technique that involves excising an appropriately-sized piece of nail bed tissue from one side of the nail bed and transplanting it to the distal end, thereby increasing its length while reducing its width (Citation13). The modified nail bed maintains the adhesive capacity of a standard nail bed. However, this method does not augment the surface area of the nail bed. Subsequently, Liu, T.H. proposed a method involving the excision of dermal tissue from the distal phalangeal joint of the affected finger and its transplantation to the nail bed defect, which is then protected with an artificial nail plate (Citation14). Despite this method yielding a new nail bed with some capacity to adhere to the nail plate after ten months, it led to the formation of a large wound and did not guarantee a high rate of adhesion.
Nail bed atrophy has long-term implications for many patients (Citation15). The field needs a universally accepted surgical approach for nail bed expansion, leaving a significant therapeutic need unaddressed. Through our research, we introduce an innovative surgical technique designed to mitigate nail bed atrophy effectively. This technique harnesses tension from the ventral aspect of the digit to stretch the nail bed. The research and application of this approach promise to provide a reliable and productive means for treating nail bed atrophy, thereby enhancing the quality of life for those affected.
Materials and methods
Patients
This study, conducted between 2015 and 2020, enrolled 34 patients (). The research was carried out by clinical research guidelines and regulations and received approval from the hospital’s ethics committee. Treatment procedures adhered to the principles outlined in the 1975 Helsinki Declaration, and all participants provided informed consent (). The inclusion criteria for patients (ChiCTR2000036232) were as follows:
Figure 1. Schematic diagram of the study protocol. Patients (n = 34) were enrolled in the study. In the control group, participants underwent nail extraction or did not receive specialized intervention, whereas the surgical group underwent continuous W-shaped nail bed expansion procedures. The nail bed deformity was evaluated, followed by a 12-month follow-up period. Data analysis was performed to assess the outcomes.
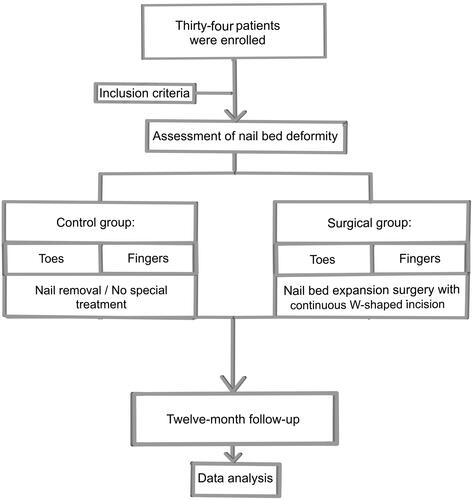
Table 1. General characteristics of patients.
Possession of complete phalanges.
A residual nail bed area exceeded 25% of the original nail bed area.
Effective control of etiological factors, such as onychomycosis.
Intact finger pulp.
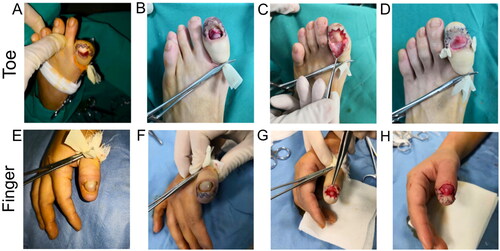
To avoid bias caused by individual differences, we employed a randomized block allocation method to divide patients into surgical and control groups. Upon their selection into the surgical group, patients underwent surgery involving a continuous W-shaped incision. During the surgery, patients were positioned prone. Adherence to a standard sterilization protocol was ensured, and sterile drapes were deployed over the patient. Subsequently, 2% lidocaine was used for local anesthesia at the base of the finger/toe. A tourniquet was applied at the base of the digit to prevent bleeding. The surgeon then used methylene blue to delineate a continuous W-shaped incision approximately 2–3 millimeters from the nail bed margin (). After the extraction of the entire nail plate, subcutaneous tissues were dissected along the methylene blue marking, separating the nail bed flaps. The contractured tissue was excised if cicatricial contracture was encountered during nail bed flap separation. Upon total elevation of the nail bed flap, any abnormal bony prominences on the dorsal aspect of the distal phalanx were addressed and smoothened as necessary to achieve a flat osseous surface. Excessive tissue was judiciously trimmed according to each patient’s condition before suturing the nail bed flaps to the surrounding digital pulp under appropriate tension (). After ensuring adequate hemostasis, 5–0 sutures were used to secure the nail bed flaps to the digital pulp, maintaining the directional stability of the nail bed to prevent morphological aberrations due to deviation. The tourniquet was then released, and the vascular supply to the finger/toe was assessed. Finally, the wound was dressed with sterile gauze to conclude the procedure. post-operative wound dressings were changed every three days, and sutures were removed two weeks post-operation ().
Figure 2. Schematic representation of the surgical procedure. (A) Continuous W-shaped incisions were made on the pulp of the finger/toe approximately 2–3 mm away from the nail bed. (B) The nail bed flap was meticulously dissected. (C) Skin and soft tissue excess were excised along the shaded area. The width of the shaded area was adjusted based on tension and blood circulation. (D) Stretching the trimmed nail bed flap toward the periphery. (E) Appropriate removal of fingertip soft tissue was performed to adjust the longitudinal axis of the nail bed flap. (F) The incision was sutured to expand the nail bed.
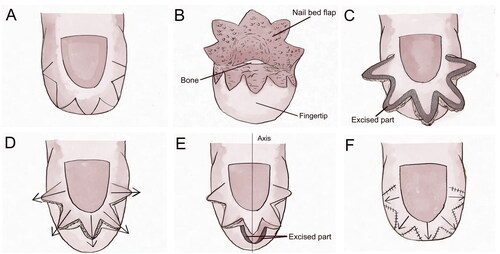
Figure 3. Application of the continuous W-Shaped incisions: (A, B) The incision is made on the toe pulp about 2–3 millimeters away from the nail bed. (C) The nail bed flap is carefully dissected along the design line and appropriately trimmed based on tension and blood circulation. The remaining nail bed flap is stretched outward, and the longitudinal axis is adjusted by removing soft tissue from the fingertip. (D) Finally, the incision is sutured to push the nail bed. (E–H) Continuous W-shaped incision nail bed surgery was conducted on the patient’s thumb.
In this study, patients in the control group had their underlying pathologies, such as infections, already controlled at the time of inclusion. Four individuals underwent toenail removal within the control group due to severe nail plate deformities. The remaining patients, whose nail plate deformities were tolerable and who experienced a relatively lower degree of pain, did not reach the threshold that would prompt them to seek medical intervention actively. Within the control group, cases with nail bed atrophy did not receive any specific treatment related to nail bed expansion during the assessment period.
Measurements
At month 0 and month 12 of the study, we employed a flexible ruler to measure the height and width of the nail bed. The surface area of the nail bed was calculated by multiplying the height and width measurements. Furthermore, we utilized the ratio of sizes at the follow-up to initial values for comparison between the two groups. A scoring system ranging from 0 to 10 was employed to gauge patient satisfaction with the cosmetic results of nails during the follow-up period, with 10 denoting the highest level of satisfaction and 0 indicating the lowest. During statistical analysis, the ratio of values measured at the 12-month follow-up to those at the experiment’s inception was used to compare the differences between the surgical and control groups.
Furthermore, we used the visual analog scale (VAS) to assess the pain experienced by patients in both groups. VAS is a commonly used self-report pain assessment tool that allows patients to mark their current pain level on a continuous line, with the endpoints being ‘no pain’ and ‘worst pain imaginable.’ The bar is typically 10 cm long, and the pain score is determined by the distance between the marked point and the ‘no pain’ endpoint. By calculating the difference between the quantities measured at the 12-month follow-up and those measured at the outset, we could evaluate the impact of the surgery on the pain experienced by the patients.
In this study, we employed the Semmes–Weinstein Monofilament (SWM) test to obtain tactile scores at follow-up, with the primary aim of observing changes in tactile sensitivity among patients in the surgical group to determine the safety and feasibility of the surgical intervention. The SWM test uses a series of monofilaments to administer tactile stimulation to the test area, calibrating the applied force to elicit a bend in the monofilament. A stimulation duration of 1.5 s is maintained, with accompanying documentation of the patient’s response to each stimulation. The results are classified into two levels, standard and reduced sensitivity, based on the threshold of tactile sensitivity on the corresponding area of the healthy toe/finger. This test method can evaluate the recovery of tactile sensation in patients after surgery and is essential for assessing surgical outcomes.
Data analysis
All data were analyzed using SPSS 26.0 statistical software. In the present study, we employed a paired T-test for intra-group analysis to assess the temporal changes in nail bed width and height within the surgical and control groups. The Wilcoxon rank sum test was utilized to compare the differences in nail bed height, width, and surface area between the control and surgical groups. This method also analyzed the esthetic scores and pain intensity for both groups. The results of the SWM test were analyzed using a Chi-square test. Data are presented as mean ± standard deviation or as proportions. Statistical significance was considered at p < 0.05.
Results
This study employed a random allocation method to divide the patients into surgical and control groups. Furthermore, nail-related data from 34 patients have been successfully obtained and documented.
In this study, we conducted a correlative analysis of the degree of change in the nail bed over time. For this purpose, two-time points were selected, namely, the baseline (month 0) and the study’s conclusion (month 12). Specifically, a comparison of nail bed height values at these two-time points was made for the control group. The results revealed a p-value of 0.09 (p > 0.05), indicating no significant change in nail bed height in the control group during our study. Further, an analogous analysis was conducted on the nail bed width values for the control group, and it corroborated the lack of significant change with a p-value of 0.09 (p > 0.05) over the observation period. However, for the surgical group, a starkly contrasting outcome was observed. Upon measurement at the same time points (month 0 and month 12), a significant increase in nail bed height was recorded at 12 months post-operation, with a p-value of 0.00 (p < 0.05), signifying statistical significance. Similarly, a significant augmentation in nail bed width was documented, with a p-value of 0.00 (p < 0.05). Collectively, these findings illuminate the absence of substantial change in nail bed height and width for the control group over this period. In contrast, the surgical group exhibited a notable increase in both nail bed dimensions within the same duration.
Regarding the comparison between the surgical group and the control group, after 12 months of follow-up, patients in the surgical group showed transparent, painless, and well-adhered neo-nails without signs of necrosis, blood supply disorders, or other complications (). The previously deformed nails of the patients returned to a natural and attractive state ( and ).
Figure 4. Comparison of outcomes at baseline and 12 months post-intervention between the control group and surgical group (toes): (A) control group: This patient, who had their nail removed due to severe nail plate deformity, exhibited malformed regrowth of the nail plate with compromised transparency at follow-up. (B) Control group: without any specific treatment, no significant alteration in the nail bed is observed in this patient after 12 months. (C, D) Surgery group: as can be seen, the newly formed nail plate is more symmetrical and exhibits a smoother surface after the surgical intervention. There is also an increase in the nail bed’s length and width, which validates the efficacy of the surgical approach employed in this study.
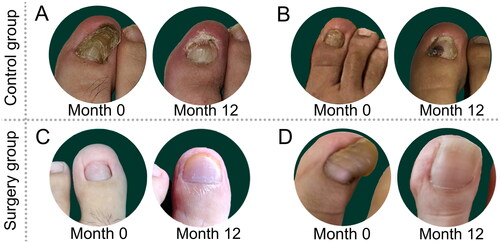
Figure 5. Comparison of outcomes at baseline and 12 months post-intervention between the control group and surgical group (fingers): (A, B) control group: for two patients, who did not undergo any specific treatment, no notable alteration in the nail bed is observed after 12 months. (C, D) Surgery group: the figure demonstrates the significant changes in the newly formed nail plate following surgical intervention.
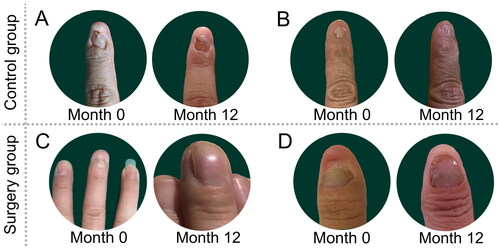
Table 2. Comparison of nail bed alterations between the surgical and control groupsTable Footnote*.
Within the surgical group, the ratio of nail bed height at 12 months post-operation to the preoperative measurement was 1.50 ± 0.49, whereas, in the control group, the ratio (follow-up/baseline) was 0.90 ± 0.16. The difference between the groups was statistically significant, with a p-value of 0.00 (p < 0.05), indicating a more substantial change in nail bed height in the surgical group compared to the control group and suggesting the capability of continuous W-shaped incision surgery to augment nail bed height. Additionally, compared to preoperative measurements, the surgical group exhibited a ratio of 1.16 ± 0.23 for nail bed width at 12 months post-operation. In contrast, the control group displayed a balance of 0.91 ± 0.17 for nail bed width. Compared to the change in nail bed width in the control group, there was a significant improvement in the surgical group (p < 0.05).
Furthermore, as both nail bed height and width were enhanced in the surgical group, there was a notable expansion in nail bed surface area. At 12 months follow-up, the nail bed surface area in the surgical group attained 1.69 ± 0.60 times the original nail bed surface area. In contrast, the control group demonstrated unsatisfactory nail bed area progression. The follow-up examination at 12 months revealed a reduction in nail bed surface area compared to baseline measurements, with a ratio of 0.84 ± 0.24. In reaching the nail bed surface area, the surgical group showed more significant improvement than the control group (p < 0.05).
In the analysis above, we observed that the surgery significantly improved the height, width, and area of the patient’s nail beds. However, this raised an exploratory question: Is the surgery’s efficacy affected by the operation site? To delve deeper into this issue, we conducted a more detailed subgroup analysis of the data. Specifically, we compared the changes in toenail beds in the surgical group with those in the control group (). Likewise, we compared the differences in fingernail beds in the surgical group with those in the control group ().
The change in the toenail height ratio showed a p-value of 0.00 (p < 0.05), indicating that the change in the surgical group was more significant than in the control group. A similar analysis of the difference in the width ratio of the toenails yielded a p-value of 0.00 (p < 0.05), confirming the advantage of the surgical group in the change in the toenail width ratio. Analysis of the area ratio change in toenails also showed similar results, with a p-value of 0.00 (p < 0.05).
Subsequently, we turned our attention to the changes in fingernail beds. Here, our analysis yielded results akin to those of the toenails. In comparing the height, width, and area of the nail bed between the surgical group and the control group, we found that the improvements in the height, width, and area of the nail bed were more pronounced in the surgical group than in the control group, with specific p-values of 0.00 (p < 0.05), 0.00 (p < 0.05), and 0.00 (p < 0.05), respectively. These results suggest that the surgery significantly improves nail bed dimensions in both fingers and toes, independent of the specific surgical site.
At the 12-month follow-up, we evaluated the esthetic outcomes of the surgical and control groups using the ratio of esthetic scores at 12 months to baseline. The esthetic score ratio for the surgical group was 2.22 ± 0.71, significantly higher than that of the control group (p < 0.05). Pain score changes were similar for both groups, with reported average pain scores of less than 1 point at 12 months. The SWM test results indicate that the surgery has a negligible negative impact on fingertip tactile sensitivity. In conclusion, our study suggests that the surgical approach can effectively enhance the nail bed’s height, width, and area, thereby improving esthetic outcomes and patient satisfaction. The surgery does not compromise the patient’s fingertip sensation ().
Discussion
Nail bed atrophy is a common pathological condition, often caused by delayed or inadequate treatment of acute or chronic infections. Its main pathological changes involve degeneration or shrinkage of the nail bed tissue, significantly impacting the patient’s quality of life. Surgical intervention is of paramount importance in addressing such issues.
The two traditional methods for nail bed atrophy are essentially the same, both involving the removal of a portion of the covering tissue above the nail root while preserving the entire nail plate to achieve a visual expansion of the nail bed. Traditional surgery is implemented based on the assumption that the patient’s nail plate is typical and not pathologically atrophied. Patients undergo surgery primarily due to subjective dissatisfaction with the esthetic appearance of the nail plate. Consequently, these methods have inherent limitations and only apply to patients with average nail plate thickness, curvature, and transparency. Therefore, abnormal nail plates are not within the scope of indications for these two surgical methods.
In contrast, the surgical technique with continuous W-Shaped incisions has a broader range of applications, including nail plates with different thicknesses, curvature, and transparency on fingers and toes. This surgical technique restores a new transparent and smooth nail bed by stretching the nail bed, even if the previous nail plate was malformed. Therefore, compared to traditional surgical methods, one advantage of the continuous W-shaped incision is that it does not have the limitation of requiring a healthy and transparent nail plate. Additionally, traditional nail bed surgery is primarily used for fingers, making it unsuitable as a control group for this study. Furthermore, using a continuous W-shaped incision on the volar side during surgery has less tissue damage than tissue grafting methods, resulting in shorter surgical duration and reduced patient discomfort (Citation11,Citation15).
During the surgical procedure, the longitudinal adjustment of the nail bed is also noteworthy because it is a unique tissue that provides adhesion and guides the direction of nail growth (Citation16,Citation17). In this study, we employed the continuous W-shaped incision during the surgical process, through this incision approach, we could apply appropriate traction to the surrounding nail bed and adjust its longitudinal axis to parallel that of the finger (or toe). This process involves the removal of proper tissue from the nail bed flap and the staggered suturing of the incision on the volar side, further influencing the direction of new nail growth.
Furthermore, post-operative esthetics is associated with the height, width, and surface area of the nail bed (Citation17). Using the continuous W-shaped incision technique allows for more precise adjustment of the size and direction of the nail bed, facilitating the restoration of the more natural nail bed shape and appearance. As for post-operative rehabilitation management, although our study did not specifically focus on rehabilitation management, it is crucial for the patient’s recovery. After surgery, patients must rest their fingers or toes and avoid excessive activity or heavy lifting to prevent unnecessary damage to the surgical site or compromise the surgical outcomes.
It should be noted that there are some limitations to our study. Firstly, the sample size was small, and the study was conducted in a single center. Thus further studies with larger sample sizes and multicenter designs are needed to validate the stability and reliability of our results. Secondly, our study only observed the 12-month effects after surgery, and further long-term follow-up is required to investigate whether the surgical outcomes may change over time.
In conclusion, our study results suggest that the surgical method we designed can effectively improve the appearance of nail bed deformities in fingers/toes, with high surgical safety and fast post-operative recovery, and has high clinical value. However, further research and exploration on post-operative management, optimization, and improvement of surgical methods are needed to improve surgical outcomes and patients’ quality of life.
Conclusion
This study employed the design of a continuous W-shaped surgical incision to correct nail bed deformities in fingers/toes. The objective was to achieve a simple and minimally invasive surgical procedure while ensuring effective treatment outcomes. Through the observation and analysis of preoperative and post-operative indicators such as nail bed height, width, and surface area, we found that this surgical approach significantly improved these parameters and elevated the overall level of surgical outcomes. Furthermore, our research highlighted the importance of adjusting the vertical axis of the nail bed during the surgical procedure, providing the necessary strength and directional guidance to enhance treatment effectiveness. However, it should be noted that the sample size in this study was relatively small, and further research is needed to validate and refine the findings. Overall, this study provides a simple, feasible, and effective surgical approach for correcting finger/toenail bed deformities, offering valuable references for clinical practice.
Ethical approval
The clinical research part of this project was performed according to the clinical research rules and regulations and implemented after it received approval from the ethics committee of the Shanghai Ninth People’s Hospital.
Disclosure statement
No potential conflict of interest was reported by the author(s). Financial disclosure statements have been obtained, and no conflicts of interest have been reported by the authors or by any individuals in control of the content of this article.
Data availability statement
Datasets generated and analyzed during the course of this study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Samman PD. Idiopathic atrophy of the nails. Br J Dermatol. 1969;81(10):1–7. doi: 10.1111/j.1365-2133.1969.tb15934.x.
- Barth JH, Millard PR, Dawber RP. Idiopathic atrophy of the nails. A clinico-pathological study. Am J Dermatopathol. 1988;10(6):514–517. doi: 10.1097/00000372-198812000-00007.
- Dehesa L, Tosti A. Treatment of inflammatory nail disorders. Dermatol Ther. 2012;25(6):525–534. doi: 10.1111/j.1529-8019.2012.01516.x.
- Donovan KM. Antarctic environment and nail growth. Br J Dermatol. 1977;96(5):507–510. doi: 10.1111/j.1365-2133.1977.tb07153.x.
- Ferrusquia-Toriz D, Hernandez-Diaz C, Amezcua-Guerra LM, et al. Ultrasound characterization of the nail bed in patients with systemic lupus erythematosus. Lupus. 2021;30(4):608–614. doi: 10.1177/0961203320988609.
- Chang C, Beutler BD, Cohen PR. Polydactylous transverse erythronychia: report of a patient with multiple horizontal red bands affecting the fingernails. Dermatol Ther. 2017;7(2):255–262. doi: 10.1007/s13555-017-0177-2.
- Oliveira MH, Pinto FCM, Ferraz-Carvalho RS, et al. BIO-NAIL: a bacterial cellulose dressing as a new alternative to preserve the nail bed after avulsion. J Mater Sci-Mater Med. 2020;31:9.
- Goulden V, Goodfield MJD. Onychomycosis and linear nail growth. Br J Dermatol. 1997;136(1):139–140. doi: 10.1111/j.1365-2133.1997.tb08772.x.
- Regana MS, Ezquerra GM, Millet PU, et al. Treatment of nail psoriasis with 8% clobetasol nail lacquer: positive experience in 10 patients. J Eur Acad Dermatol Venereol. 2005;19:573–577.
- Jain A, Jones A, Gardiner MD, et al. NINJA trial: should the nail plate be replaced or discarded after nail bed repair in children? Protocol for a multicentre randomised control trial. BMJ Open. 2019;9(12):e031552. doi: 10.1136/bmjopen-2019-031552.
- Gunasagaran J, Sian KS, Ahmad TS. Nail bed and flap reconstructions for acute fingertip injuries – a case review and report of a chemical burn injury. J Orthop Surg. 2019;27:1–6.
- Mak MCK, Ho PC, Chow ECS, et al. Neurovascular island flap for pulp and nail augmentation in thumb duplication reconstruction: a surgical method with long-term follow-up. J Hand Surg-Am. 2021;46:8.
- Li MW, Chen ZY, Yang YJ, et al. Split-Thickness nail bed flap graft in the management of distal partial defect of the nail bed combined with soft tissue. J Hand Surg-Am. 2020;45:10.
- Liu TH, Hsieh MC, Chou PR, et al. Reconstruction for defects of total nail bed and germinal matrix loss with acellular dermal matrix coverage and subsequently skin graft. Med Lith. 2020;56:7.
- Stewart CL, Rubin AI. Update: nail unit dermatopathology. Dermatol Ther. 2012;25(6):551–568. doi: 10.1111/j.1529-8019.2012.01510.x.
- Geyer AS, Onumah N, Uyttendaele H, et al. Modulation of linear nail growth to treat diseases of the nail. J Am Acad Dermatol. 2004;50(2):229–234. doi: 10.1016/j.jaad.2003.07.011.
- Chen HY, Hsu CC, Lin YT, et al. Functional and aesthetic outcomes of the fingertips after nail lengthening using the eponychial flap. J Plast Reconstr Aesthet Surg. 2015;68(10):1438–1446. doi: 10.1016/j.bjps.2015.06.005.

