Sir,
Darier’s disease (DD) is a rare autosomal dominant genodermatosis, characterized by hyperkeratotic papules in a predominately seborrheic and intertriginous distribution with associated nail findings such as onychoschizia. In most cases, DD develops from childhood and persists through adolescence. DD is characterized by brown, keratotic papules of varying sizes, ranging from pinhead to millet seed which develops in seborrheic areas such as the forehead, central chest, back, and scalp margins. The lesions are often associated with itching and malodor (Citation1). The genetic abnormality is due to a mutation in the ATP2A2 gene on chromosome 12q23-24 which encodes SERCA2, a calcium ATPase in the sarco/endoplasmic reticulum. Mutations in the ATP2A2 gene, which encodes the 2b isoform of the Sarcoendoplasmic Reticulum Calcium-ATPase pump (SERCA2b). This mutation leads to calcium pump dysfunction and ultimately epidermal acantholysis and apoptosis (Citation2).
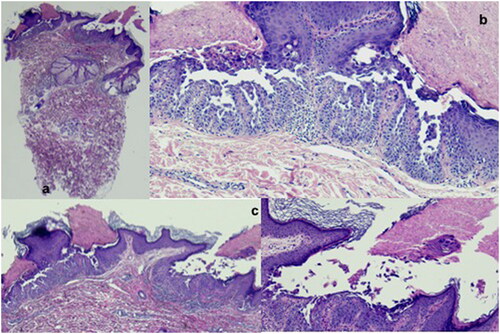
A 32 years old woman presented to the hospital with a widespread rash. Ten days prior to admission she developed congestion and fatigue and tested positive for COVID-19. Physical examination revealed extensive keratotic, erythematous, edematous papules and vesicles on the trunk and extremities (). The face was spared. Chronic Darier nail changes were noted with splinter hemorrhages, longitudinal bands, and v-shaped nicks. The patient reported a history of diffuse xerosis, associated with fine scaling and keratosis pilaris-like follicular papules, which had been treated with emollients with mild to moderate improvement. A suspect of Darier’s disease was made on the basis of the clinical appearance, and a skin biopsy confirmed it with the presence of typical features (.
Figure 1. Extensive keratotic, erythematous, edematous papules and vesicles on the trunk and extremities.

Figure 2. a) Papule of Darier’s disease showing suprabasal acantholysis, with the formation of a small cleft, associated with a thicked stratum corneum, with focal parakeratosis (Haematoxylin-eosin; original magnification 10x); b) Dyskeratotic cells are observed both in the upper malpighian layer and the stratum corneum (corps ronds and grains), floating also in the suprabasal cleft (Haematoxylin-eosin; original magnification 100x); c) Papillary dermis projections covered by a single layer of basal cells extend into the suprabasal cleft. In the superficial dermis is observed mild lymphocytic infiltrate, with rare eosinophils (Haematoxylin-eosin; original magnification 40x).
Therapy with systemic retinoids was proposed to the patient. However, she refused due to the desire for motherhood. For this reason, topical therapy was initiated with partial benefit.
Well-known triggers of Darier’s disease primarily include exogenous factors such as sun exposure, friction, or infection (Citation3). In addition, case reports describe flares of Darier’s disease following treatment of interferon therapy, lithium and COVID-19 vaccination indicating involvement of a possible immune mechanism (Citation4). To date, COVID-19 infection can exacerbate some inflammatory skin diseases such as psoriasis and atopic dermatitis; however, to the best of our knowledge, COVID-19-associated DD exacerbations have been reported only in one case. it is supposed that a cytokine storm caused by COVID-19 infection can lead to a flare of DD (Citation5). Specifically, COVID-19 infection produces a cytokine storm characterized by elevated levels of TNF-alpha, IL-6, and IL-1β (Citation6) TNF-alpha and IL-6 act to downregulate ATP2A2 mRNA levels, which would decrease the capacity of an already dysfunctional SERCA2b calcium pump in patients with Darier disease (Citation7). Expression of ATP2A2 was decreased by high level of IL-1a and IL-6 also (Citation8). Furthermore, IL-1a and TNF-a have been shown to be relevant in the regulation and synthesis of complement and proteases, so they could play an important part in exacerbation of DD favoring acantholysis (Citation9). Finally, we must consider that fever, sweating and bed rest during COVID-19 infection are known factors for the exacerbation of Darier’s disease. The mechanism of DD’s exacerbation after COVID-19 is still unclear, the cytokine storm and the clinical condition of the patient could play a pivotal role in this. However, data on genetic dermatoses during COVID-19 are limited and further studies are mandatory to shed a light on the pathogenetic mechanisms that lead to flare of these diseases.
Disclosure statement
None.
Data availability statement
Additional data supporting the findings of this manuscript are available upon reasonable request to the corresponding author.
Additional information
Funding
References
- Takagi A, Kamijo M, Ikeda S. Darier disease. J Dermatol. 2016; 43(3):1–2. PMID: 26945535. doi: 10.1111/1346-8138.13230.
- Savignac M, Edir A, Simon M, et al. Darier disease: a disease model of impaired calcium homeostasis in the skin. Biochim Biophys Acta. 2011;1813(5):1111–1117. Epub 2010 Dec 15. PMID: 21167218. doi: 10.1016/j.bbamcr.2010.12.006.
- Burge SM, Wilkinson JD. Darier-White disease: a review of the clinical features in 163 patients. J Am Acad Dermatol. 1992; 27(1):40–50. doi: 10.1016/0190-9622(92)70154-8.
- Elbæk MV, Vinding GR, Jemec GBE. Darier’s disease flare following COVID-19 vaccine. Case Rep Dermatol. 2021;13(2):432–436. doi: 10.1159/000517256.
- Dykes R, Martin T, Ergen E, et al. Exacerbation of darier’s disease with COVID-19. JAAD Case Rep. 2022;27:64–66. doi: 10.1016/j.jdcr.2022.06.037.
- Jalloh S, Olejnik J, Berrigan J, et al. CD169-mediated restrictive SARS-CoV-2 infection of macrophages induces pro-inflammatory responses. bioRxiv. 2022;18(10):e1010479. doi: 10.1101/2022.03.29.486190.
- Yamamoto T, Aoyama Y. Role of pro-inflammatory cytokines in the pathophysiology of herpes simplex virus superinfection in darier’s disease. J Dermatol. 2021;48(10):1607–1611. doi: 10.1111/1346-8138.16097.
- Mayuzumi N, Ikeda S, Kawada H, et al. Effects of ultraviolet B irradiation, proinflammatory cytokines and raised extracellular calcium concentration on the expression of ATP2A2 and ATP2C1. Br J Dermatol. 2005;152(4):697–701. PMID: 15840101. doi: 10.1111/j.1365-2133.2005.06383.x.
- Feliciani C, Toto P, Amerio P, et al. In vitro and in vivo expression of interleukin-1alpha and tumor necrosis factor-alpha mRNA in pemphigus vulgaris: interleukin-1alpha and tumor necrosis factor-alpha are involved in acantholysis. J Invest Dermatol. 2000;114(1):71–77. PMID: 10620118. doi: 10.1046/j.1523-1747.2000.00835.x.

