Delusions of parasitosis (DOP) is a psychocutaneous disorder presenting as monosymptomatic hypochondriacal psychosis, generally with fixed delusions about skin infestation or infection (Citation1–3). DOP can be classified as either a primary disease or secondary to substance use, various medications, or the presence of additional psychiatric, neurologic, and organic medical conditions (Citation1). Patients with DOP commonly present to a dermatologist due to their concern about a primary skin disorder, but differences in patients’ beliefs and physicians’ clinical understanding about their condition often result in dissatisfaction, significant loss to follow-up, and inadequate treatment (Citation3). A skin biopsy may strengthen therapeutic rapport between physician and patient, therefore increasing the chance for successful treatment with antipsychotics and psychiatric intervention (Citation3–5). Our aim was to investigate factors affecting follow-up rates in patients presenting with DOP, specifically whether receiving a biopsy at the initial visit for DOP alters follow-up retention.
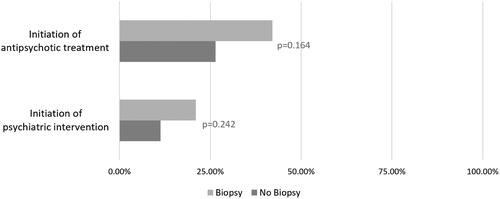
We conducted a retrospective chart review of 125 patients diagnosed with DOP or a DOP-related disorder, including Morgellons disease and Ekbom syndrome, by a dermatologist at the University of Virginia Medical Center between January 1, 1998 and January 30, 2023 (). Fifty-seven percent of patients had no follow-up visits with dermatology at UVA after their diagnosis while 43% had at least one follow-up visit. Follow-up retention was not associated with undergoing a biopsy at initial visit (p = 0.651). When we classified patients based on primary versus secondary forms of DOP, we similarly found no association between biopsy at initial visit and follow-up (data not shown). In addition, we found no significant difference in follow-up rates based on age, gender, or distance from UVA (p = 0.663, p = 0.685, p = 0.978). Interestingly, we did find that performing a biopsy at any point in the care of a patient with DOP was associated with higher rates of initiation of an antipsychotic medication (42.11% vs 26.42%) and initiation of psychiatric intervention (21.01% vs 11.32%), however these were not statistically significant ().
Table 1. Comparison of demographic and clinical characteristics of the two groups (N = 125).
There are several limitations to this study. First, our sample size of only 125 total patients and 19 patients who received a biopsy as part of their management was small and at increased risk of uncontrolled confounding. Second, we reviewed patients with DOP from only one hospital center. Additional large-sample multi-center studies would help to verify our findings.
In summary, given the complex nature of treating patients with DOP, further research is needed to identify factors associated with increased follow-up rate, patient acceptance of diagnosis, and improved outcomes. Importantly, our data shows that a biopsy at an initial visit is not associated with an increased follow-up rate. However, biopsy may still be a useful tool in the management of DOP by facilitating a strong provider-patient therapeutic alliance and encouraging initiation of psychiatric intervention and antipsychotic medications.
IRB approval status
Reviewed and approved by UVA IRB; approval #24282
Disclosure statement
Research for Regeneron and Concert.
References
- Campbell EH, Elston DM, Hawthorne JD, et al. Diagnosis and management of delusional parasitosis. J Am Acad Dermatol. 2019;80(5):1–2. doi: 10.1016/j.jaad.2018.12.012.
- Heller MM, Wong JW, Lee ES, et al. Delusional infestations: clinical presentation, diagnosis and treatment. Int J Dermatol. 2013;52(7):775–783. doi: 10.1111/ijd.12067.
- Koo J, Lee CS. Delusions of parasitosis. A dermatologist’s guide to diagnosis and treatment. Am J Clin Dermatol. 2001;2(5):285–290. doi: 10.2165/00128071-200102050-00003.
- Jeon C, Nakamura M, Koo J. The demand for skin biopsy from a patient with delusional parasitosis. J Am Acad Dermatol. 2017;77(5):e125. doi: 10.1016/j.jaad.2017.05.021.
- Hylwa SA, Bury JE, Davis MD, et al. Delusional infestation, including delusions of parasitosis: results of histologic examination of skin biopsy and patient-provided skin specimens. Arch Dermatol. 2011;147(9):1041–1045. doi: 10.1001/archdermatol.2011.114.