Abstract
Background
Although biologics improve the quality of life of psoriasis patients, they also impose a substantial economic burden. There is a lack of research addressing the economic and humanistic impact of biologics in China.
Objective
This cross-sectional investigation aims to assess the economic cost, quality of life, and patient satisfaction among individuals with psoriasis treated with biologics and non-biologics.
Methods
From July 2021 to December 2022, eligible patients with psoriasis were recruited through both on-site and online questionnaire completion. The questionnaires collected sociodemographic data, clinical characteristics of psoriasis, economic costs associated with treatment, and the Dermatological Life Quality Index (DLQI).
Results
481 patients with a mean age of 40.8 ± 13.4 years old were included and classified into a non-biologic (n = 195) and biologic (n = 286) treatment group. The direct medical cost for non-biologics patients was 7,249 CNY, accounting for 70.0% of the total cost, while biologics patients incurred 15,176 CNY, making up 94.3% of the total cost. The non-biologic group had higher costs related to hospitalization, self-purchase of drugs, and indirect costs than the biologic treatment group. Additionally, DLQI scores were higher in the non-biologic group.
Conclusion
Patients in the biologic group experienced a higher economic burden and better quality of life than those in the non-biologic group.
1. Introduction
Psoriasis is an immune-mediated, chronic disease with a global prevalence of 1–3% (Citation1,Citation2). The prevalence varies among different ethnic groups and regions, with a higher incidence in Western countries than in Asia (Citation1). The incidence rate is 2–4% in the United States (Citation3), 2.8% in the United Kingdom (Citation4), and 0.47% in China (Citation5). Due to the chronic, persistent nature of the disease, patients often require lifelong care, which results in high ongoing treatment costs (Citation6). Psoriasis also has a wide range of emotional and psychological effects on patients due to impaired appearance and disability, resulting in stigmatization, low self-esteem, increased pressure, impaired social functions, and interpersonal relationships (Citation7,Citation8). In addition, psoriasis is associated with various comorbidities, such as nonalcoholic fatty liver disease, obesity, hypertension, dyslipidemia, diabetes, cardiovascular disease, psychiatric disease, and inflammatory bowel disease.
Treatment of psoriasis encompasses topical therapy, phototherapy, systemic therapy, or combination therapy. Mild to moderate psoriasis can be treated with topical treatment, such as glucocorticoids and vitamin D3 analogs. In most cases, topical agents are combined to reduce side effects and improve the effectiveness of systemic therapy. However, a combination of phototherapy and systemic therapy is usually required for moderate to severe plaque psoriasis. Phototherapy reduces cell proliferation and induces apoptosis of T cells and keratinocytes by absorbing ultraviolet (UV) light into the skin (Citation9). Systemic therapy is divided into oral medications therapy and biologics therapy. Oral medications includes acitretin, methotrexate (MTX) and cyclosporine. Current evidence suggests that combining phototherapy and systemic therapy (such as cyclosporine) is not recommended due to the risk of carcinogenesis. In a large-scale transnational survey (Citation10), only 25% of patients receiving traditional systemic treatment were very satisfied with the treatment, and half expressed concerns about the health risks of long-term treatment. The discontinuation rate was high due to concerns regarding safety, tolerability, and ineffectiveness of treatment. Biologics are usually indicated after phototherapy and when conventional systemic therapy fails.
Biologics are targeted therapy drugs resulting from integrating research on the pathogenesis of psoriasis and molecular biology. Unlike non-biologics, biologics are targeted treatments that act on specific inflammatory pathways or cytokines. However, the high price of biologics can be a major obstacle for doctors and patients with psoriasis. Compared with biologics, traditional treatments are relatively low-cost; however, patients with moderate to severe psoriasis are often less able to work effectively and may have to seek lower-paid roles or even face unemployment (Citation11,Citation12). In these cases, the indirect cost caused by productivity loss may exceed the direct cost of psoriasis treatment (Citation13). Highly effective biologics may offset the higher costs by reducing indirect and hospital costs.
There are few reports on the economic cost of psoriasis treatment in China. As more biologics are now included in China’s medical insurance, they are becoming the treatment of choice for patients with moderate and severe psoriasis and psoriatic arthritis. Biologics can significantly improve the quality of life, reduce hospitalization rates, and enhance treatment satisfaction and compliance among this patient population.
To investigate the impact of biologic treatment on economic cost, quality of life, and patient satisfaction, we conducted a survey involving outpatient and hospitalized patients in our hospital.
2. Materials and methods
2.1. Subjects
The present study was a cross-sectional survey of patients with psoriasis who visited the dermatology department of Xuzhou Medical University from July 2021 to December 2022. Patients included in the study were required to meet the diagnostic criteria for psoriasis and have a disease course of at least 1 year. The age range of the participants was between 18 and 80 years. However, individuals who had previously participated in other drug, physical, or psychological trials related to psoriasis within the past year were excluded from the study.
2.2. Observation items
The questionnaire used in the study consisted of several sections. The first section gathered sociodemographic data, including information about gender, age, height, weight, and occupation. The second section focused on clinical characteristics and included questions about the patient’s medical history, family history of psoriasis, the type of psoriasis they had, the extent of psoriasis on their body surface area (BSA), and any comorbidities they may have had. The assessment of BSA was conducted with the assistance of the investigator. Additionally, the Dermatological Life Quality Index (DLQI) questionnaire was also included in the survey
2.3. Cost estimation
Economic cost refers to the direct and indirect economic cost of psoriasis over the past year. Direct costs include outpatient and hospital expenses for psoriasis or complications in the past year, self-purchased medications, nursing expenses, and transportation expenses. In our study, the reimbursement requirements for biological agents in China requires regular follow-up visits for most patients receiving biologic treatment at our hospital. Detailed records of outpatient and inpatient visits were readily available for these patients. For those treated with non-biologic agents, medical invoices were used as a reference to gather cost information. In cases where patients did not have invoices, we calculated costs by retrieving medication information from the past year and combining it with drug price data obtained from the China Pharmaceutical Inquiry Platform. All costs were presented in Chinese Yuan (CNY), and the average official conversion rate in 2021 was 6.45 CNY per 1.00 USD.
Due to discrepancies in local financial support, the reimbursement policies for biologic medical insurance differ across different regions of China. Taking Jiangsu Province as an example, the reimbursement ratio for biological agents ranges from approximately 60–80%, and the total reimbursement amount varies from around 30,000 to 100,000 CNY, depending on the specific region. Any amount exceeding the total reimbursement is the patient’s responsibility and must be paid out-of-pocket. During medical settlement, the medical insurance directly covers 60–80% of the expenses, while the residents are required to pay the remaining 40–20%. However, civil servants benefit from a higher reimbursement rate of 98.5%. Similar to others, they are responsible for any amount exceeding the total reimbursement, which they must pay at their own expense. For individuals without health insurance, they are required to pay the full cost of the treatment. Therefore, in our cost calculations, we only considered the out-of-pocket expenses incurred by the patients when evaluating the drug costs.
Indirect costs encompass the number of days patients and their caregivers have been off work due to psoriasis over the past year and are measured using the human capital approach. To determine the average monthly/daily wage incomes, we referred to the 2021 per capita Gross Domestic Product Index released by the China National Bureau of Statistics, which was 80,906 CNY. In China, the mandatory retirement age is 60 for men and 55 for women. Consequently, productivity loss for patients and their families beyond this age was not factored into the calculations of indirect costs.
2.4. DLQI
The DLQI is composed of ten questions concerning patients’ perception of the impact of skin disease on six aspects of their quality of life over the last week (Citation14). These ten questions are divided into six groups as follows: Symptoms and feelings (Questions 1 and 2), Daily activities (Questions 3 and 4), Leisure activities (Questions 5 and 6), Work or school (Question 7), Personal relationships (Questions 8 and 9), and Treatment (Question 10). If there is one missing answer in any dimension, the entire dimension is considered missing. In cases where two or more questions are left unanswered, the total DLQI score is considered missing, and the questionnaire is deemed invalid.
2.5. Statistical analysis
Data were analyzed by IBM SPSS 26.0 statistical software, and appropriate statistical methods were adopted according to data type. A Student’s t-test was employed for continuous variables with a normal distribution and homogeneous variance, and the results were expressed as mean ± SD (standard deviation). A Chi-squared test was used for categorical variables, and the results were presented as frequencies and percentages. A p-value less than 0.05 was statistically significant.
3. Results
3.1. Sociodemographic and clinical characteristics data
A total of 490 questionnaires were distributed, and 481 valid questionnaires were collected, resulting in a response rate of 98.1%. The biologic treatment (BT) group consisted of 286 patients, while the non-biologic treatment (Non-BT) group had 195 patients. The mean age of all participants was 40.8 ± 13.4 years, with the youngest patient being 18 years old and the oldest 78 years old. The included patients were predominantly male (n = 195, 40.5%) and urban residents (n = 315, 65.3%). The most common comorbidities observed were hypertension, obesity, and dyslipidemia ().
Table 1. Demographic and clinical characteristics of different treatments among patients with psoriasis.
3.2. Patient expectation and satisfaction
The expectations of both groups were similar, with most patients aiming for complete removal of skin lesions, while a few patients desired relief from itching or pain (5.6 vs. 2.8%). In the BT group, most patients (78.3%) were satisfied with the treatment effect, while a minority expressed dissatisfaction (7.7%). On the other hand, in the Non-BT group, around one-third of patients were satisfied (27.7%), but nearly half reported dissatisfaction (42.1%, ).
Table 2. Expectation and satisfaction of treatment in two groups.
3.3. Economic burden of psoriasis patients
Among the 286 patients treated with biologics, 155 (54%) received biologic treatment for at least a year and were included in the cost of biologics study. The average annual total costs in the Non-BT and BT groups were 10,340 CNY and 16,093 CNY, with direct costs accounting for 70.0% and 94.3% and indirect costs accounting for 29.9 and 5.7%, respectively ().
Table 3. Total economic burden/patient.
3.4. DLQI in two groups
Patients in the BT group experienced better quality of life across all dimensions than the Non-BT group (p < 0.01). Among both groups, symptoms had the highest impact, while work and study had the lowest impact (). When analyzing the factors influencing the decision of patients in the Non-BT group not to use biologic agents, 114 (58.5%) stated they had not heard of or did not understand biologics, 31 (15.9%) mentioned having mild psoriasis and not requiring them, and 26 (13.3%) expressed concerns about the cost ().
Table 4. DLQI in two groups.
Table 5. Reasons for not using biologics in non-biologic treatment users.
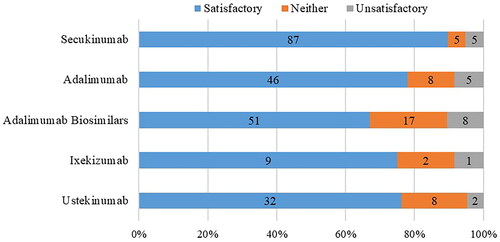
3.5. Treatment satisfaction
Patients were treated with the following biologics: secukinumab (n = 97), adalimumab biosimilars (n = 76), adalimumab (n = 59), istekinumab (n = 42), and ixekizumab (n = 12). The satisfaction analysis revealed that most patients (n = 224, 78.3%) were satisfied with treatment efficacy, while 22 patients (7.7%) were not. Secukinumab patients showed the highest rate of treatment satisfaction (89.7%), followed by adalimumab patients (78.0%); those on adalimumab biosimilars reported the lowest satisfaction rate (67.1%, ).
4. Discussion
Etanercept was the first biological agent approved by the US FDA to treat psoriasis in 2004. Since then, various other biological agents have been approved for psoriasis treatment, including subgroups of biologics such as TNF-α inhibitors, IL-17 inhibitors, and IL-12/IL-23 inhibitors (Citation15). In this study, investigators did not use etanercept due to its relatively slow onset (Citation16,Citation17) and high injection frequency compared to other biologics. The use of biological agents is becoming increasingly prevalent in the population, and our study aims to examine the economic and human impact of biologics on Chinese psoriasis patients.
Consistent with the literature (Citation18,Citation19), direct medical costs constituted a major component of the financial burden on psoriasis patients, regardless of the treatment approach. The average direct cost for patients in China ranged from 6542 to 11,362 CNY (Citation20,Citation21), consistent with our survey results. The direct medical cost in the Non-BT group was 7,249 CNY, accounting for 70.0% of the total cost, while in the BT group, it was 15,176 CNY, accounting for 94.3%, indicating that biologics were the primary driver of healthcare costs. However, the cost of hospitalization and self-purchase of drugs in the BT group was lower than in the Non-BT group.
Regarding indirect costs, the average cost in the Non-BT group was 3091 CNY, accounting for 29.9% of the total cost, while in the BT group, it was 917 CNY, accounting for 5.7%, which may be attributed to the high efficacy of biologics in alleviating patients’ symptoms and reducing the need for unnecessary family care. Moreover, the longer injection frequency allows patients to choose non-weekday treatment. In our study, the BT group predominantly consisted of patients with moderate-severe psoriasis, while the number of patients with mild, moderate, and severe psoriasis in the Non-BT group was equal. This difference in disease severity might lead to an underestimation of the economic burden in the Non-BT group.
Healthcare workers exhibited a 2-fold higher likelihood of receiving biologic treatment compared to non-biologics, whereas students and farmers were associated with a rate of receiving non-biologic treatment that was more than 2-fold higher. This phenomenon may be related to the level of knowledge and access to information about different treatment options and types of medical insurance. Highly knowledgeable groups, especially medical workers, are more aware of new treatment options and usually have employee health insurance and higher incomes, making them more proactive in seeking medical treatment, including biologics. In contrast, the number of farmers and students receiving treatment with non-biological agents is relatively high.
Psoriasis is associated with an increased risk of cardiovascular disease (Citation22–24), which may be reduced using TNF-α and IL-17 inhibitors (Citation25,Citation26).
First-line treatment for patients with moderate-to-severe plaque psoriasis depends largely on the condition, severity, comorbidities, country, and drug availability. For example, traditional systemic therapies like methotrexate, cyclosporine, and acitretin remain the primary first-line treatments for patients with moderate-to-severe plaque psoriasis in China, while the American Academy of Dermatology-National Psoriasis Foundation guidelines recommend biologics as the first-line treatment of choice for moderate-to-severe plaque psoriasis.
Biological agent therapy has been the most significant advancement in psoriasis treatment in recent years because it can control systemic inflammation and has additional positive effects on other organs, such as psoriatic arthritis. Many patients have achieved remarkable results, reaching PASI75 or even PASI90. The improvement in objective disease severity improves patients’ quality of life. Biologics have substantial benefits, improving general and somatic symptoms, sleep disturbances, social dysfunction, anxiety, and dysphoria compared to traditional systemic and topical treatments (Citation27). DLQI scores under any biological treatment decreased by an average of 6.6 by the 24th week, indicating a considerable enhancement in patients’ overall quality of life (Citation28). The DLQI scores of patients in our BT group were lower than those in the Non-BT group across all dimensions.
However, this study has several limitations. First, it is subject to recall bias due to the nature of the questionnaire used. Second, the research primarily focused on patients in central China treated in our hospital, which might limit its generalization. Additionally, the selection bias of this study may have led to an overestimation of the average economic cost, as patients who were negative about treatment and did not visit were not included.
5. Conclusions
There is a considerable disparity between biologic and non-biologic treatments concerning patients’ economic burden and quality of life. Biologics enhance patient quality of life, but they also come with a higher financial burden.
Acknowledgments
We are grateful to all patients and staff who participated in this study. This study received no external funding.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available upon request from the corresponding author, Guan Jiang, from the Affiliated Hospital of Xuzhou Medical University, upon reasonable request. Interested parties may request access to the data by contacting Dr. Guan Jiang via email at [email protected].
Additional information
Funding
References
- Parisi R, Symmons DP, Griffiths CE, et al. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133(2):1–6. doi: 10.1038/jid.2012.339.
- Parisi R, Iskandar IYK, Kontopantelis E, et al. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369:m1590. doi: 10.1136/bmj.m1590.
- Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70(3):512–516. doi: 10.1016/j.jaad.2013.11.013.
- Springate DA, Parisi R, Kontopantelis E, et al. Incidence, prevalence and mortality of patients with psoriasis: a UK population-based cohort study. Br J Dermatol. 2017;176(3):650–658. doi: 10.1111/bjd.15021.
- Ding X, Wang T, Shen Y, et al. Prevalence of psoriasis in China: a population-based study in six cities. Eur J Dermatol. 2012;22(5):663–667. doi: 10.1684/ejd.2012.1802.
- Radtke MA, Augustin M. Economic considerations in psoriasis management. Clin Dermatol. 2008;26(5):424–431. doi: 10.1016/j.clindermatol.2007.10.024.
- Dalgard FJ, Gieler U, Tomas-Aragones L, et al. The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol. 2015;135(4):984–991. doi: 10.1038/jid.2014.530.
- Lesner K, Reich A, Szepietowski JC, et al. Determinants of psychosocial health in psoriatic patients: a multi-national study. Acta Derm Venereol. 2017;97(10):1182–1188. doi: 10.2340/00015555-2760.
- Vañó-Galván S, Gárate MT, Fleta-Asín B[, et al. Analysis of the cost effectiveness of home-based phototherapy with narrow-band UV-B radiation compared with biological drugs for the treatment of moderate to severe psoriasis. Actas Dermosifiliogr. 2012;103(2):127–137. doi: 10.1016/j.ad.2011.05.002.
- Lebwohl MG, Bachelez H, Barker J, et al. Patient perspectives in the management of psoriasis: results from the population-based multinational assessment of psoriasis and psoriatic arthritis survey. J Am Acad Dermatol. 2014;70(5):871–881.e1-30. doi: 10.1016/j.jaad.2013.12.018.
- Levy AR, Davie AM, Brazier NC, et al. Economic burden of moderate to severe plaque psoriasis in Canada. Int J Dermatol. 2012;51(12):1432–1440. doi: 10.1111/j.1365-4632.2011.05359.x.
- Horn EJ, Fox KM, Patel V, et al. Association of patient-reported psoriasis severity with income and employment. J Am Acad Dermatol. 2007;57(6):963–971. doi: 10.1016/j.jaad.2007.07.023.
- Berger K, Ehlken B, Kugland B, et al. Cost-of-illness in patients with moderate and severe chronic psoriasis vulgaris in Germany. J Dtsch Dermatol Ges. 2005;3(7):511–518. doi: 10.1111/j.1610-0387.2005.05729.x.
- Finlay AY, Khan GK. Dermatology life quality index (DLQI)–a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–216. doi: 10.1111/j.1365-2230.1994.tb01167.x.
- Menter A, Strober BE, Kaplan DH, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics. J Am Acad Dermatol. 2019;80(4):1029–1072. doi: 10.1016/j.jaad.2018.11.057.
- Langley RG, Elewski BE, Lebwohl M, et al. Secukinumab in plaque psoriasis–results of two phase 3 trials. N Engl J Med. 2014;371(4):326–338. doi: 10.1056/NEJMoa1314258.
- Griffiths CE, Reich K, Lebwohl M, et al. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. Lancet. 2015;386(9993):541–551. doi: 10.1016/S0140-6736(15)60125-8.
- Balogh O, Brodszky V, Gulácsi L, et al. Cost-of-illness in patients with moderate to severe psoriasis: a cross-sectional survey in Hungarian dermatological centres. Eur J Health Econ. 2014;15(Suppl 1): s101–s109. doi: 10.1007/s10198-014-0599-z.
- Ghatnekar O, Ljungberg A, Wirestrand LE, et al. Costs and quality of life for psoriatic patients at different degrees of severity in Southern Sweden – a cross-sectional study. Eur J Dermatol. 2012;22(2):238–245. doi: 10.1684/ejd.2011.1635.
- Zhao MY, Wu J, Li YM. Economic burden of patients with moderate to severe psoriasis and its influencing factors (in Chinese). Chin J Dermatol. 2014;47:817–820.
- Chen XL, Zheng LY, Zhang H, et al. Disease burden and quality of life in patients with psoriasis: an internet-based questionnaire survey (in Chinese). Chin J Dermatol. 2019;52(11):791–795.
- Shiba M, Kato T, Izumi T, et al. Risk of myocardial infarction in patients with psoriasis: a cross-sectional patient-population study in a Japanese hospital. J Cardiol. 2019;73(4):276–279. doi: 10.1016/j.jjcc.2018.10.008.
- Furue M, Tsuji G, Chiba T, et al. Cardiovascular and metabolic diseases comorbid with psoriasis: beyond the skin. Intern Med. 2017;56(13):1613–1619. doi: 10.2169/internalmedicine.56.8209.
- Caiazzo G, Fabbrocini G, Di Caprio R, et al. Psoriasis, cardiovascular events, and biologics: lights and shadows. Front Immunol. 2018;9:1668. (doi: 10.3389/fimmu.2018.01668.
- Wu JJ, Poon KY, Channual JC, et al. Association between tumor necrosis factor inhibitor therapy and myocardial infarction risk in patients with psoriasis. Arch Dermatol. 2012;148(11):1244–1250. doi: 10.1001/archdermatol.2012.2502.
- Wu JJ, Guérin A, Sundaram M, et al. Cardiovascular event risk assessment in psoriasis patients treated with tumor necrosis factor-α inhibitors versus methotrexate. J Am Acad Dermatol. 2017;76(1):81–90. doi: 10.1016/j.jaad.2016.07.042.
- Takahashi H, Iinuma S, Tsuji H, et al. Biologics are more potent than other treatment modalities for improvement of quality of life in psoriasis patients. J Dermatol. 2014;41(8):686–689. doi: 10.1111/1346-8138.12544.
- Norris D, Photiou L, Tacey M, et al. Biologics and dermatology life quality index (DLQI) in the australasian psoriasis population. J Dermatolog Treat. 2017;28(8):731–736. doi: 10.1080/09546634.2017.1329501.