Abstract
Background
While pincer nails may be treated using overcurvature-correcting devices, it takes several months to achieve successful outcomes. Nail-softening drugs may reduce the treatment duration required.
Objective
To evaluate the efficacy and safety of treatment with acetylcysteine (AC) gel added to an overcurvature-correcting device, and define the optimal AC concentration.
Methods
In this investigator-blinded study, 70 patients with hallux pincer nail were fitted with an overcurvature-correcting device for 7 days and were randomly assigned to receive a single 24-h administration of a gel containing 10%, 20% or 30% AC or vehicle. Nail improvement was objectively evaluated by calculating the distal narrowed nail width (dNNW) ratio.
Results
All three AC concentrations plus device showed earlier sustained improvement of pincer nails versus vehicle plus device. There was no observable correlation between AC concentration and effectiveness. No clinically problematic adverse events were observed at any AC concentration, and we recommended AC gel at a concentration of 10%.
Conclusions
By adding AC gel application to an overcurvature-correcting device, early and sustained reductions in transverse curvature were produced compared with using a device alone (vehicle control). The dNNW ratio used in this study was an appropriate objective index for evaluating therapeutic effects.
Trial registration:
Introduction
Pincer nail has an incidence rate of around 0.9%, and generally affects the hallux toenail (Citation1). Patients present with a characteristic narrowing of the nail bed and an increase in the maximum transverse curvature at the distal end of the nail (Citation2). While there are several causes of pincer nails (including ill-fitting shoes and osteoarthritis) (Citation1), the resulting transverse overcurvature occurring in each case may cause symptoms ranging from mild discomfort to intolerable pain (Citation3). This, in turn, affects the ability of patients to walk or wear shoes (Citation1,Citation4,Citation5), thereby negatively affecting their daily life.
Current treatment for pincer nails is divided into preservative procedures (which aim to retain the nail and nail bed) and surgical intervention (in which the nail and underlying nail bed undergo invasive manipulation via e.g. incision, excision, detachment, or ablation) (Citation6). Preservative methods, such as plates and wires, are used to correct deformation, revert the transverse curvature to a near normal state, and relieve the subjective symptoms experienced by patients (Citation6). However, such procedures take a long time to produce change, and for patients with very thick nails, additional wires or repeated procedures may be required to successfully resculpt the nail (Citation1). Surgery may be recommended in cases of severe deformity (Citation2,Citation7,Citation8). but this is invasive and may itself result in severe discomfort or poor cosmetic appearance.
Topical agents to chemically soften the nail have also been evaluated as a treatment for pincer nail (Citation1,Citation9), with the aim of decreasing the time taken to reduce the transverse curvature and prevent recurrence. Acetylcysteine (AC) is a compound containing a thiol group which is able to cleave the disulfide bonds within keratin, a key nail constituent (Citation10,Citation11); thus, AC is able to destabilize the keratin structure of the nail and soften it.
While there is no accepted standard treatment for pincer nails, overcurvature-correcting devices containing super-elastic nickel-titanium wires have shown good therapeutic results (Citation12); however, the time period needed for effective treatment is in the region of 3–6 months. We hypothesized that the addition of AC alongside an overcurvature-correcting device might reduce the treatment period, and conducted this study to evaluate the effectiveness and safety of combination treatment, and define the optimal concentration of AC. Moreover, since combination treatment with AC plus device is a new technique without established measures of effectiveness, we conducted an exploratory study to confirm the usefulness of an objective evaluation method for the incurvated nail correction effect.
Patients and methods
Patients
Eligible patients were aged 20 years or older, with a pincer nail on the right or left hallux. The pincer nail was required to have a distal narrowed nail width (dNNW) ratio of not less than 20% and not more than 50%. In the case that both the left and right halluces met the inclusion criteria, the one with the smaller dNNW ratio was selected as the pincer nail to be assessed. Exclusion criteria are described in Supplemental Text S1. Use of any pharmaceutical drug, alternative therapy, and cosmetic around the pincer nail was prohibited throughout the study, and nail clipping was also not allowed. All patients provided written informed consent for study participation.
Study design, treatments and blinding
This was a phase I/II, randomized, vehicle-controlled, investigator-blind, parallel-group, comparative and dose-finding study in patients with hallux pincer nail. This study was conducted in compliance with the Declaration of Helsinki, Good Clinical Practice ordinance, and all other legal and regulatory requirements, and was registered at clinicaltrials.jp with the identifier jRCT-2080224657. The study was conducted at a single center (Medical Corporation Shinanokai Shinanozaka Clinic, Tokyo, Japan) between 8 April and 28 July 2019, and the protocol and all associated documentation were approved by the Institutional Review Board of the clinic.
Following confirmation of eligibility on study day 1, patients were randomly assigned (1:1:1:1) to AC gel 10%, 20%, 30%, or vehicle (Supplemental Figure S1). All study treatments (active gel and vehicle comparator) were provided by the study sponsor (Maruho Co., Ltd.). All patients were fitted with the overcurvature-correcting device (Makizume Meister®; Maruho Hatsujyo Kogyo Co., Ltd.). This comprises a nickel-titanium wire and coiled spring which is attached to the nail edges via U-hooks.
During visit 1 (day 1), the device was affixed by the clinician, following which the area around the nail was protected with masking material to prevent the chemical treatment from adhering to the skin. A single topical administration of approximately 0.5 g of AC gel or vehicle was applied to the entire incurvated nail plate, and a polyurethane film used as a dressing. Because of the formulation characteristics of AC gel, it was considered difficult to ensure complete blinding. Thus, the medical personnel responsible for drug allocation and application, and the patients themselves were not blinded, but the investigator/outcome evaluator, all other study personnel, and the sponsor remained blinded until the end of the study. The dressing and topical treatment were removed after 24 h (visit 2). The device remained in position for a total of 7 days before removal during visit 3 (day 8). There was a further observation period to assess the outcomes of treatment, with visit 4 occurring on day 15.
Efficacy outcomes
Efficacy endpoints were dNNW ratio (calculated using a previously published method (Citation13)); changes in the dNNW ratio; third-party evaluation of morphological improvement and recovery using photographs of the nail; dose-response for the dNNW ratio; proximal NNW (pNNW) ratio, and subjective outcomes of nail shape and pain using questionnaires.
The dNNW ratio was calculated using measurements of actual width (A, measured at baseline), distal bilateral margin width of the nail plate (B, measured at each visit), and apparent width of the proximal nail plate (C, measured at each visit) (see Supplemental Figure S2). The distal ratio was calculated as B/A × 100%, and the proximal ratio as C/A × 100%. Third-party evaluations were conducted by three experienced dermatologists familiar with the treatment of pincer nails; prior to the trial commencing, these evaluators agreed a consensus for the photographic evaluation methodology and standardized the evaluation criteria. Morphological improvement was assessed as ‘significant improvement’, ‘improvement’, and ‘unchanged’. Similarly, morphological recovery was assessed on a 3-point scale, where 1 denoted no ‘excessive transverse curvature’ on distal bilateral margins of nail plate (patient recovered), 2 denoted slight ‘excessive transverse curvature’ (patient not recovered; corrective treatment may or may not be given), and 3 denoted ‘excessive transverse curvature’ (corrective treatment was recommended).
Safety outcomes
Safety evaluations included adverse events (AEs; comprising subjective symptoms, objective findings, and abnormal laboratory test fluctuations), and laboratory test values. AEs were categorized using the Medical Dictionary for Regulatory Activities/Japanese edition version 22.0. Events were assessed for severity, and for relationship to the topical treatment. AEs of special interest (AESIs) were any AE leading to inflammation (e.g. erythema, edema) around the nail to which the topical treatment was applied, or any AE leading to removal of the overcurvature-correcting device. Blood samples were obtained at each visit to assess hematological and biochemical parameters.
Statistical analyses
As this was not a confirmatory study, no specific sample size calculations were performed. It was intended to enroll 15 patients per treatment group. Efficacy outcomes were evaluated using the full analysis set (FAS), which included all enrolled patients who received topical treatment and had data available for analysis. The safety set included additional patients who were enrolled in the study as part of a separate pharmacokinetic analysis of AC gel (not reported herein).
The dNNW ratio was analyzed using mixed-effects models for repeated measures (MMRM). The model included the baseline as a response variable under the assumption that the expected value would be equal between the treatment groups, and included the treatment group-by-visit interaction as the fixed effect. No structure was specified for the variance-covariance matrix. Missing values were not imputed and multiplicity adjustment was not applied. The morphological improvement evaluation, reduction evaluation, and questionnaires were analyzed using the two-sample Wilcoxon test. All statistical calculations were performed using SAS software version 9.4 (SAS Institute, Inc., Cary, NC).
Results
Patients
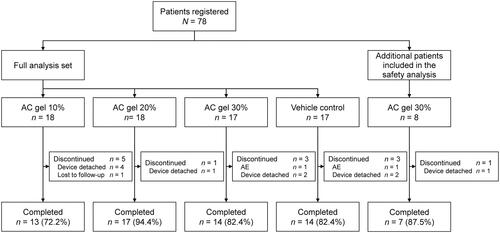
The FAS included 70 patients and the safety set comprised 78 patients; disposition is shown in . The most common reason for study discontinuation was detachment of the overcurvature-correcting device. Two patients (2.6%) discontinued due to AEs, and one (1.3%) failed to complete study visits and was lost to follow-up.
Figure 1. Patient disposition. The full analysis set (N = 70) used for efficacy outcomes included all patients randomized to treatment in the main part of the study. The safety set (N = 78) included an additional eight patients. AC: acetylcysteine gel; AE: adverse event.
Baseline demographic and clinical characteristics are shown in . The majority of patients were female (75.7% [53 of 70] in the FAS, and all of the additional patients [8 of 8] included in the safety set). Age distribution was similar across treatment groups, and around three quarters of patients (72.2–88.2% across the treatment groups) had no prior history of pincer nail. Overall, the mean narrowed nail width ratios were 38.4% (distal) and 68.9% (proximal).
Table 1. Baseline demographic and clinical characteristics (safety set).
Results for the dNNW ratio
At baseline, the mean values for the dNNW ratios were similar among AC gel groups (38.6–39.8%) and the vehicle control group (38.9%). By visit 2, all groups showed improvement, with no significant differences between AC gel or vehicle (); the least squares mean values were 66.0–72.6% in the AC groups and 66.5% in the vehicle group. However, by visit 3, ratios in the vehicle group had decreased and there were significant differences between all AC gel groups and the vehicle group (p ≤ 0.01 for all); these were maintained to visit 4 (p < 0.0001 for all).
Figure 2. Distal narrowed nail width ratios. (A) Time course of change, (B) absolute change, and (C) rate of change (full analysis set). Data are shown as mean ± standard deviation, and missing values were not imputed.
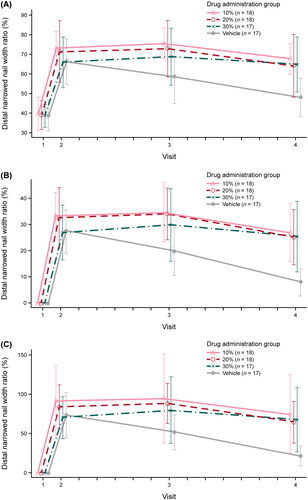
The least squares mean value of the absolute change in the dNNW ratio in the AC groups at visit 2 was 33.5% for 10% AC, 32.6% for 20% AC, and 26.9% for 30% AC (). The change in the 10% AC group was statistically significantly different from the vehicle group (27.4%; p = 0.0700) but was not statistically significant for the 20% and 30% AC groups. However, values in all three AC groups were statistically significantly different from vehicle at visit 3 (10% AC, p < 0.0001; 20% AC, p = 0.0003; 30% AC, p = 0.0109) and visit 4 (all, p < 0.0001)
The least squares mean value for change in the rate of dNNW ratio () at visit 2 was 93.3% in the 10% AC group, showing a statistically significant difference from the vehicle group (72.6%; p = 0.0342). There were no statistically significant differences between the 20% AC group (83.1%) and the 30% AC group (69.2%) and vehicle. However, statistically significant differences between all three AC groups and vehicle were observed at visit 3 (10% AC, p < 0.0001; 20% AC, p = 0.0020; 30% AC, p = 0.0211) and visit 4 (all, p < 0.0001).
Before and after photographs of a patient treated with 10% AC gel plus the overcurvature-correcting device are provided in Supplemental Figure S3. The improvement in nail curvature can be observed following the removal of the device (visit 3) and remains improved at visit 4.
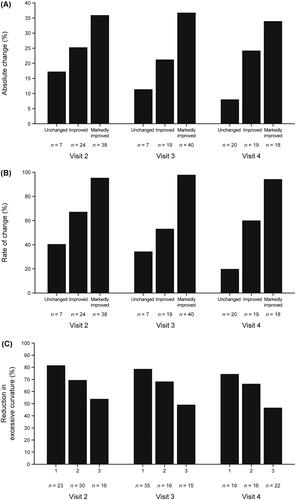
Evaluation of changes in the dNNW ratio
The average value of the change in the dNNW ratio in the patients who showed ‘significant improvement’ was 33.9–36.8%, and that of the patients who showed ‘improvement’ or were ‘unchanged’ was 21.2–25.2% and 8.0–17.1%, respectively (). The average rate of change in the dNNW ratio was 94.2–97.7% for patients who had ‘significant improvement’, 53.9–67.6% for patients who were ‘improved’, and 20.8–40.9% for those who were ‘unchanged’ (). In patients who were judged to have no excessive transverse curvature and were recovered (score of 1), the mean value of the dNNW ratio was 74.2–80.7%. In patients with a score of 2 (some excessive transverse curvature), the mean value was 66.2–68.9%; in patients who still had excessive transverse curvature and required further treatment (score 3), the mean value was 46.3–53.8% (). In all cases, patients who were assessed as improved had increased ratios, and those who were not improved had lower ratios.
Figure 3. Assessments of morphological changes in distal narrowed nail width. (A) Absolute improvement in narrowing, (B) rate of change of narrowing, and (C) reduction in excessive transverse curvature (full analysis set). in panel ‘C’, 1 denotes no ‘excessive transverse curvature’ was observed on distal bilateral margins of nail plate, and the patient was judged to be recovered; 2 denotes slight ‘excessive transverse curvature’ was observed on distal bilateral margins of nail plate, and the patient was not recovered (corrective treatment may or may not be given); 3 denotes ‘excessive transverse curvature’ on distal bilateral margins of the nail plate was observed, and corrective treatment was recommended.
Third-party morphological evaluation using photographs
At visit 2, there were no statistically significant differences between AC and vehicle groups for either morphological improvement or recovery. By visit 4, there were significant differences between all AC groups and vehicle for morphological improvement (p ≤ 0.0180) and morphological recovery (p ≤ 0.0044). Full details are provided in Supplemental Tables S1–S2.
Dose response for dNNW ratio
Although the dNNW ratio on day 8 was higher in all AC groups than in the vehicle group, there were no notable differences according to drug concentration.
Results for the pNNW ratio
No significant differences were seen between AC gel groups and vehicle. At visit 3, the least squares mean value was 70.8–71.3% in the AC groups and 71.4% in the vehicle group.
Results of patient questionnaires
Results of the patient questionnaires are shown in Supplemental Figure S4 and Supplemental Table S3. By visit 4, all groups showed a decrease in dissatisfaction with nail shape and a decrease in pain associated with pincer nails.
Safety
The incidence of AEs was 16.7% (3 of 18 patients) in the 10% AC group; 27.8% (5 of 18) in the 20% AC group; 28.0% (7 of 25) in the 30% AC group; and 5.9% (1 of 17) in the vehicle group (). All events were mild in severity. No deaths were reported during the study. One serious AE occurred (uterine leiomyoma in one patient in the 10% AC group), but this was judged unrelated to AC gel or the overcurvature-correcting device by the investigator. The only AE occurring in ≥ 1 patient was nail bed bleeding (in two patients in the 20% AC group) (Supplemental Table S4). No AEs related to laboratory test values were observed in this study.
Table 2. Summary of safety outcomes (safety set).
The incidence of treatment-related AEs that occurred at or around the administration site of the AC gel was 5.6% (1 of 18) in the 10% AC group, 16.7% (3 of 18) in the 20% AC group, and 8.0% (2 of 25) in the 30% AC group. No dose dependence was observed in the frequency of events.
One patient in the 10% AC group had an AESI of erythema, but this was judged not be related to AC gel by the investigator. One patient each in the 30% AC and vehicle groups had an AE of nail damage which required removal of the device. The event in the 30% AC group was determined to be causally-related to treatment, while that in the vehicle group was not. Both events were mild and the patients recovered.
Discussion
Overcurvature-correcting devices are widely used to treat pincer nails because of their therapeutic benefit and relative simplicity (Citation1), but successful treatment may take several months. We found that the addition of AC gel during the first 24 h of use of the device facilitated sustained improvements at an earlier stage than the device alone. Moreover, we found that a concentration of 10% was efficacious, being both successful in improving nail curvature and well-tolerated by patients.
The patient population included in this study was relatively small, but was nonetheless representative of the patients seen in routine clinical practice; patient demographic characteristics at baseline were also aligned with prior studies of pincer nail treatments (Citation7,Citation9,Citation12,Citation14), with a preponderance of females and a mean age of 47.6–55.3 years. This suggests that the results from this study will be generalizable to the wider patient population presenting at dermatology clinics for treatment.
Although the use of the device alone (vehicle control group) also showed improvements in the dNNW ratio, the vehicle provided only short-term softening and did not break the disulfide bonds in the nail keratin. Thus, while results were similar after 24 h of topical treatment, only AC gel maintained the device-induced improvements of the pincer nail at visits 3 and 4, and showed statistically significant divergence from vehicle. After the removal of the overcurvature-correcting device, ratios in the vehicle group at visits 3 and 4 were lower than at visit 2. In the AC gel groups, no change was seen in the dNNW ratios in a drug concentration-dependent manner. Overall, this combination treatment was found to improve pincer nails from an early stage and maintain those improvements compared with the device alone (vehicle control).
The use of a compound with the ability to break disulfide bonds within keratin is not without precedent, as a study conducted more than a decade ago used thioglycolic acid (TGA; a commercial depilatory agent) for a similar purpose (Citation9). However, TGA is potentially hazardous and may cause skin irritation or chemical burns (Citation15), and a more recent publication suggested that it may be necessary to combine TGA with surgery in order to obtain adequate results (Citation16). In contrast, topical AC gel compounds have shown both efficacy and tolerability in the treatment of several dermatologic conditions with disturbed keratinization, including atopic dermatitis, and lamellar ichthyosis (Citation17,Citation18). As such, many dermatologists are likely to be familiar with the properties of AC, and the application of 10% AC gel to treat pincer nail is a rational clinical extension of its use.
Although there have been prior studies reporting third-party morphologic evaluation for pincer nails (Citation19,Citation20), this is the first clinical study in which such methodology has been validated. Our exploratory analyses suggested that when the dNNW ratios improved, the photo evaluation and patient evaluation by a third party also improved. Thus, we consider that the dNNW ratios would be useful as an objective evaluation index for pincer nails.
Importantly, all AEs reported in this study were mild, and there were no deaths and few AC-related events. AEs related to treatment (AC gel or device) were erythema (one patient in the 10% AC group) and damaged nails (two patients; one each in the 30% AC group and the vehicle group), but these were mild and recovered. No drug-related serious AEs occurred. There was also no increase in AE incidence with drug concentration. In this study, based on the potential for skin irritation when using AC gel, the skin around the pincer nails to be evaluated was protected with a masking material. Based on the lack of concentration-dependent effects, we consider that in clinical use, protecting the skin around the pincer nails with a masking material will be effective in preventing AEs of skin irritation caused by AC gel.
The main study limitation was the small study size and exploratory nature of the endpoints. In addition, the exclusion criteria meant that patients with an ingrown toenail were not eligible for evaluation due to differing treatment recommendations, and those with brittle pincer nails and pincer nails less than 1 mm thickness were not eligible as a result of difficulty in attaching the device. Further studies in a wider patient base will be needed to confirm these findings across the full clinical population. Finally, in this study, the follow-up period after removing the nail correction devices was set to 7 days. Studies with a longer duration of follow-up are warranted in order to confirm the maintenance of the pincer nail correction effect over time.
Conclusions
The results of this study, to evaluate the combined use of AC gel and an overcurvature-correcting device to improve pincer nails, support the clinical utility of (1) the use of AC gel at a concentration of 10% and (2) the implementation of dNNW ratios as an objective index to numerically gauge the corrective effect. Crucially, we confirmed that the combined use of AC gel and an overcurvature-correcting device was able to provide early and sustained improvements in pincer nails compared with the device alone (vehicle control), thereby potentially improving the patient experience and reducing inconvenience.
Supplemental Material
Download PDF (344.3 KB)Acknowledgments
The authors wish to express their gratitude to the patients and their families for their contributions to the study, and to the project members at Maruho Co., Ltd., especially Kanako Ito. We thank Kazutoshi Harada (Tokyo Medical University), Kaoru Takayama (Sokuiku Laboratory), and Tomo Sakiyama for their assistance in performing the third-party morphological evaluations. We also thank Sally-Anne Mitchell, PhD, of McCann Health CMC, Japan, for providing medical writing support, which was funded by Maruho Co., Ltd.
Disclosure statement
MS has received personal fees from Maruho Co., Ltd. AI, AF, and KT are employees of Maruho Co., Ltd.
Data availability statement
The research data underlying this study are subject to restrictions and cannot be shared.
Additional information
Funding
References
- Huang C, Huang R, Yu M, et al. Pincer nail deformity: clinical characteristics, causes, and managements. Biomed Res Int. 2020;2020:1.
- Baran R, Haneke E, Richert B. Pincer nails: definition and surgical treatment. Dermatol Surg. 2001;27(3):261–8.
- Plusje LG. Pincer nails: a new surgical treatment. Dermatol Surg. 2001;27(1):41–43.
- Cornelius CE3rd, Shelley WB. Pincer nail syndrome. Arch Surg. 1968;96(2):321–322.
- Pang HN, Yi-Liang Lee J, Beng-Hoi Tan A. Pincer nails complicated by distal phalangeal osteomyelitis. J Plast Reconstr Aesthet Surg. 2009;62(2):254–257.
- Kasuya A, Tokura Y. Preservative and surgical interventions to treat ingrown nail and pincer nail. J Cutan Immunol Allergy. 2018;1(5):165–169.
- Jung DJ, Kim JH, Lee HY, et al. Anatomical characteristics and surgical treatments of pincer nail deformity. Arch Plast Surg. 2015;42(02):207–213.
- Shin WJ, Chang BK, Shim JW, et al. Nail plate and bed reconstruction for pincer nail deformity. Clin Orthop Surg. 2018;10(3):385–388.
- Okada K, Okada E. Novel treatment using thioglycolic acid for pincer nails. J Dermatol. 2012;39(12):996–999.
- Murdan S. Drug delivery to the nail following topical application. Int J Pharm. 2002;236(1–2):1–26.
- Saner MV, Kulkarni AD, Pardeshi CV. Insights into drug delivery across the nail plate barrier. J Drug Target. 2014;22(9):769–789.
- Tseng JT, Ho WT, Hsu CH, et al. A simple therapeutic approach to pincer nail deformity using a memory alloy: measurement of response. Dermatol Surg. 2013;39(3 Pt 1):398–405.
- Sakiyama T, Chaya A, Shimizu T, et al. A simple and useful method for evaluating pincer nail deformity. Jpn J Dermatol. 2016;126(12):2275–2280.
- Lee JI, Lee YB, Oh ST, et al. A clinical study of 35 cases of pincer nails. Ann Dermatol. 2011;23(4):417–423.
- Burnett CL, Bergfeld WF, Belsito DV, et al. Final amended report on the safety assessment of ammonium thioglycolate, butyl thioglycolate, calcium thioglycolate, ethanolamine thioglycolate, ethyl thioglycolate, glyceryl thioglycolate, isooctyl thioglycolate, isopropyl thioglycolate, magnesium thioglycolate, methyl thioglycolate, potassium thioglycolate, sodium thioglycolate, and thioglycolic acid. Int J Toxicol. 2009;28(4 Suppl):68–133.
- Dikmen A, Ozer K, Ulusoy MG, et al. Triple combination therapy for pincer nail deformity: surgical matricectomy, thioglycolic acid, and anticonvex sutures. Dermatol Surg. 2017;43(12):1474–1482.
- Janeczek M, Moy L, Riopelle A, et al. The potential uses of N-acetylcysteine in dermatology: a review. J Clin Aesthet Dermatol. 2019;12(5):20–26.
- Adil M, Amin SS, Mohtashim M. N-acetylcysteine in dermatology. Indian J Dermatol Venereol Leprol. 2018;84(6):652–659.
- Kosaka M, Kamiishi H. New strategy for the treatment and assessment of pincer nail. Plast Reconstr Surg. 2003;111(6):2014–2019.
- Yabe T. Curvature index of pincer nail. Plast Reconstr Surg Glob Open. 2013;1(7):e49.

