Abstract
Aim
Low-level light therapy (LLLT) may offer an adjunctive therapeutic tool for inflammatory skin conditions. This pilot study assessed the efficacy of a red/near-infrared (NIR)-emitting fabric for psoriasis, polymorphous light eruption (PMLE), and alopecia areata (AA).
Methods
Fourteen patients (five with psoriasis, five with PMLE, and four with AA) were instructed to wear a red/NIR-emitting (Lumiton®) garment during the 12-week study. Efficacy was assessed subjectively by patient-reported improvement and objectively by the redness, thickness, and scale of elbow psoriasis plaques, the frequency of PMLE flares, and the Severity of Alopecia Tool (SALT) score.
Results
Three patients with psoriasis completed the study while two self-discontinued. The three patients who completed the study noted improvement and two had improvements in lesion redness, thickness, or scale, while one was clinically stable. Three patients with PMLE completed the study, and none had a disease flare during the study period. Three patients with AA completed the study: two reported disease improvement and all three had an improved SALT score.
Conclusion
Use of a wellness apparel that emits red and NIR light may be associated with improved disease severity in patients with mild elbow psoriasis, PMLE, and limited AA. Limitations of this study include continuation on topical, intralesional, or systemic medications and small sample size.
Introduction
Phototherapy is a frequently employed treatment for cutaneous conditions and typically involves the administration of light at wavelengths ranging from 290 nm (broadband ultraviolet [UV] B) to 400 nm (UVA) (Citation1). The therapeutic effects of phototherapy are mediated by absorption of energy by chromophores including DNA, nucleotides, amino acids, lipids, and melanin. Modified molecules, termed photoproducts, participate in processes that vary between modalities but may include inflammation, apoptosis, immunosuppression, and photocarcinogenesis (Citation1). Larger wavelengths include red light (600–780 nm), near-infrared (NIR; 780–1,400 nm), mid-infrared (1400–3000 nm), and far-infrared (FIR; 3–1000 μm). Absorption of infrared wavelengths by cytochrome c oxidase (COX) mediates the production of adenosine triphosphate (ATP) and reactive oxygen species (ROS), modulation of nitric oxide (NO), and changes in transcription factors and cytokines (Citation2,Citation3). Red-to-NIR wavelengths also have anti-inflammatory properties that have been utilized to stimulate healing and to improve tissue oxygenation (Citation3).
Low-level light therapy (LLLT), also known as photobiomodulation, is a light-based therapeutic modality that involves a cascade of cellular responses to the absorption of nonablative red and NIR light energy (600–1000 nm). Unlike other light-based medical therapies, LLLT has an energy level below that causing thermal, ablative, or coagulative effects (Citation4). Irradiance is calculated by power in watts (W)/area (cm2), which for phototherapy is around 1 mW–5 W/cm2 (Citation5,Citation6). LLLT is administered in office via lamps and lasers as well as via at-home light-emitting diode (LED) devices that are increasingly commercially available. The primary mechanism of action of LLLT involves the absorption of a range of red-to-NIR wavelengths by COX in the mitochondrial respiratory chain, which increases mitochondrial ATP production and stimulates cellular metabolic activity—increasing cell signaling, activation of transcription factors, and oxygen metabolism and ROS production (Citation5). LLLT is based on effects observed after irradiation with defocused red laser that include hair regrowth (Citation7), enhanced wound healing (Citation8), and increased cell proliferation (Citation9). These effects occur without tissue injury or photothermal effects (Citation10).
In psoriasis, the induction of apoptosis of pathogenic T cells and keratinocytes reduces the overactive immune response and epidermal hyperproliferation. Phototherapy is efficacious for other cutaneous conditions, including polymorphous light eruption (PMLE) and alopecia areata (AA) (Citation1). Different wavelengths have varying penetration depths, defined as the depth at which the intensity or power of the field decays to 1/e of its surface value. Red light penetrates to a depth of 3.5 mm while NIR penetrates to approximately 8 mm. The radiation modality is selected according to the condition treated. In addition, UV radiation can reduce the number of macrophages and proinflammatory cytokines.
The purpose of this pilot study is to identify the potential of clothing made with red-to-NIR-emitting fabric technology to improve clinical severity in patients with psoriasis, PMLE, and AA. The LLLT apparel is intended to be worn in direct contact with the skin under ambient light. Light absorption of the technology is related to the intensity and wavelength of the ambient light, with peak effectiveness under sunlight. While the power density emitted by LLLT apparel is very small when compared with that of electrically powered LLLT lamps and lasers, LLLT apparel is intended to be worn for extended periods of time (hours and entire days), whereas LLLT lamps and lasers are typically only used for minutes at a time. The benefits of LLLT apparel may extend beyond red and NIR light therapy. Under sunlight, LLLT apparel’s light absorption and emission processes usually render the ultraviolet protection factor (UPF) of LLLT apparel 50+ and cooler than ordinary apparel due to decreased energy available to convert to heat in the fabric layer.
Methods
LLLT yarn (Lumiton®) is embedded with light-emitting dyes that absorb wavelengths in the visible red UV spectrum (approximately 200–700 nm) and emit wavelengths in the red to NIR region (600–1000 nm). Garments made from this fabric and used in this study included long-sleeved shirts and shirt sleeves ( and , used for psoriasis and PMLE) and baseball caps (, used for AA). Patients were given a garment that covered the skin or hair involved.
Figure 1. (A) Low-level light therapy sleeves used for patients with psoriasis. (B) Long-sleeved shirt used either for patients with psoriasis or polymorphous light eruption. (C) Cap used for patients with alopecia areata.

Following approval by the Wake Forest IRB (IRB00084854), patients were approached between August 2022 and February 2023 at Atrium Health Wake Forest Baptist’s dermatology clinic or identified through the Department of Dermatology database. Eligible patients were ≥18 years and were current patients of the dermatology department for psoriasis involving the elbows, PMLE, or AA. Fourteen participants with elbow psoriasis (n = 5), PMLE (n = 5), and AA (n = 4) were enrolled. Patients with elbow psoriasis and PMLE received their choice of either a long-sleeved shirt or a pair of shirt sleeves, and those with AA received a baseball cap. Photographs were obtained at the time of enrollment, and patients were instructed to continue their current treatment regimens as normal and to wear the garment daily for 12 weeks both indoors and outdoors. Patients were asked to record the number of hours they wore the garment each week.
Patients were surveyed regarding the level of improvement they noticed (“moderate,” “slight,” “no improvement,” or “worse”), as well as the overall comfort of the garment on a scale of 1 (not comfortable) to 5 (very comfortable). Patients with elbow psoriasis were assessed for the redness, thickness, and scale of elbow plaques on a scale from 0 (none) to 4 (highest), which was summed to provide a numerical score for the extent of disease. Patients with PMLE were further asked to record the number of disease flares they experienced during the study period. Patients with AA were assessed using the Severity of Alopecia Tool (SALT). Garment comfort was assessed on a scale of 1 (not comfortable) to 5 (very comfortable) and all patient surveys were aggregated by disease (i.e., aggregated all psoriasis, PMLE, and AA patients). Twelve patients responded to the survey of overall garment comfort.
Results
Psoriasis
Patients with psoriasis had a median age of 42 years (range: 34–66) and were 80% female (). Four patients identified as White and one identified as Black. Two patients stopped wearing the garment after the first week while the remaining three wore the garment between four to five days per week. Two patients had improvement in the summed score for elbow plaque redness, thickness, and scale, while one remained clinically stable (). Regarding patient-reported improvement, of the three patients who completed the study, two noted slight improvement and one noted moderate improvement.
Table 1. Patient demographics, concomitant treatments, frequency worn, patient-reported level of improvement, and overall garment comfort.
Polymorphous light eruption
PMLE participants had a median age of 57 years (range: 40–67), and 80% were female. Three patients identified as White, one identified as Black, and one identified as Asian Indian. Three patients completed the study, wearing the garment between approximately one half-day to one full day per week. None of the patients noted a PMLE flare during the study. For patient-reported improvement, two noted slight improvement, one reported moderate improvement, and two did not complete the study.
Alopecia areata
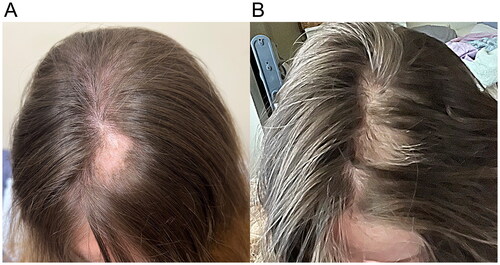
Patients with AA had a median age of 28 years (range: 22–69) and were 50% female. Two patients identified as Black and two identified as White. One AA patient was lost to follow-up. Two patients reported wearing the cap one day per week, and another wore the cap daily for two hours each day. Regarding the objective level of improvement, the three patients who completed the study had an improved SALT score (). Regarding patient-observed improvement, one patient reported slight improvement, one reported moderate improvement, and one reported no improvement.
Figure 3. (A,B) Before (week 0) and after (week 12) photographs of alopecia areata of the vertex scalp.
Patients enrolled in this study continued use of their current treatment modalities: (i) regarding the PMLE patients, one used topical corticosteroids, three used sun-protective measures, and all had no treatment changes in the 12 months prior to study onset; (ii) regarding the psoriasis patients, one used methotrexate in combination with a home light unit, two used methotrexate alone in combination with topical corticosteroids, and two used a systemic immune modulator (an interleukin-17 inhibitor); and (iii) regarding the AA patients, the three who completed the study had received intralesional triamcinolone injections, either three months or one year prior to study onset. Overall garment comfort was rated highly with an overall score of 3 (on a 5-point scale) ( and ).
Table 2. Disease outcomes at beginning and end of study.
Table 3. Assessment of elbow plaque redness, thickness, and scale for psoriasis patients who completed the study.
Discussion
LLLT is also known as photobiomodulation, and is used clinically to improve wound healing, pain, inflammation, and edema. LLLT involves application of red-to-NIR spectrum light, which is below the energy densities used for thermal, ablative, or coagulative effects and therefore has very few adverse effects. LLLT has a range of molecular, cellular, and tissue effects that are attributed to the absorption of photons in the mitochondria, leading to increased ATP production, release of NO, modulation of ROS, and production of transcription factors (Citation4).
Absorption of a photon of light causes an electron in the chromophore to become excited and to jump from a lower-energy orbit into a higher-energy orbit. The relevant chromophore has been identified to be complex IV (COX) in the electron transport chain of the mitochondria (Citation11). LLLT may cause photodissociation of NO from COX, which prevents NO-mediated displacement of oxygen from COX and leads to increased ATP production (Citation10). Because LLLT increases electron transport and oxygen is the final electron acceptor, ROS production is also increased, which leads to activation of transcription factors that play a role in cellular proliferation and migration. ROS production also leads to changes in levels of cytokines, growth factors, inflammatory molecules, and increased tissue oxygenation. Other therapeutic effects of LLLT are nitric oxide-mediated vasodilation, modulation of immune cells, and proliferation and maturation of fibroblasts.
LLLT has been studied in a wide range of clinical settings including wound healing, androgenetic alopecia, periodontics, back pain, osteoarthritis, strokes, and tendinopathies (Citation12–14). The variability in results are likely attributed to great variability among different studies in the large number of parameters including wavelength, power density and fluence, pulse structure and timing of the applied light, as well as frequency of use (Citation4).
Apparel made of yarns and fabrics that absorb energy from approximately 200–700 nm (the light spectrum from UV to visible red light) and emit energy from 600–1000 nm (red and NIR) may offer therapeutic benefits. LLLT could be a useful adjunct to other inflammatory disease treatments. In our study, three patients with PMLE, three with psoriasis, and three with AA had clinical stability or improved disease severity after 12 weeks of LLLT apparel use.
Our study has limitations: this was a small, proof-of-concept study not powered for statistical significance. Patients with limited psoriasis and AA were enrolled; one with more extensive psoriasis lesions self-discontinued due to lesion irritation from the arm sleeves. In addition, the fabric technology was not the sole mode of treatment in the majority of patients (all except one patient with AA). Therefore, the contribution of topical and systemic treatments cannot be distinguished from any possible benefit from the garment. LLLT garments may be a safe intervention, and additional study as adjunctive therapy for patients with inflammatory cutaneous conditions may be worthwhile.
IRB approval status
Reviewed and approved by Wake Forest IRB; approval number IRB00084854.
Ethical statement
Informed consent for the study and publication of photographs was obtained from all subjects.
Disclosures
Feldman has received research, speaking and/or consulting support from AbbVie, Accordant, Almirall, Alvotech, Amgen, Arcutis, Arena, Argenx, Biocon, Boehringer Ingelheim, Bristol-Myers Squibb, Dermavant, Eli Lilly and Company, Eurofins, Forte, Galderma, Helsinn, Janssen, Leo Pharma, Micreos, Mylan, Novartis, Ono, Ortho Dermatology, Pfizer, Regeneron, Samsung, Sanofi, Sun Pharma, UCB, Verrica, Voluntis, and vTv Therapeutics. He is founder and part owner of Causa Research and holds stock in Sensal Health.
Additional information
Funding
References
- Barros NM, Sbroglio LL, Buffara MO, et al. Phototherapy. An Bras Dermatol. 2021;96(4):1–5. doi: 10.1016/j.abd.2021.03.001.
- Tsai SR, Hamblin MR. Biological effects and medical applications of infrared radiation. J Photochem Photobiol B. 2017;170:197–207. doi: 10.1016/j.jphotobiol.2017.04.014.
- Walski T, Dąbrowska K, Drohomirecka A, et al. The effect of red-to-near-infrared (R/NIR) irradiation on inflammatory processes. Int J Radiat Biol. 2019;95(9):1326–1336. doi: 10.1080/09553002.2019.1625464.
- Chung H, Dai T, Sharma SK, et al. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516–533. doi: 10.1007/s10439-011-0454-7.
- Glass GE. Photobiomodulation: the clinical applications of low-level light therapy. Aesthet Surg J. 2021;41(6):723–738. doi: 10.1093/asj/sjab025.
- Huang YY, Chen AC, Carroll JD, et al. Biphasic dose response in low level light therapy. Dose Response. 2009;7(4):358–383.
- Mester E, Szende B, Gärtner P. [The effect of laser beams on the growth of hair in mice. ]. Radiobiol Radiother. 1968;9(5):621–626.
- Mester E, Spiry T, Szende B, et al. Effect of laser rays on wound healing. Am J Surg. 1971;122(4):532–535. doi: 10.1016/0002-9610(71)90482-x.
- Bosatra M, Jucci A, Olliaro P, et al. In vitro fibroblast and dermis fibroblast activation by laser irradiation at low energy. An electron microscopic study. Dermatologica. 1984;168(4):157–162. doi: 10.1159/000249691.
- Karu TI, Pyatibrat LV, Afanasyeva NI. Cellular effects of low power laser therapy can be mediated by nitric oxide. Lasers Surg Med. 2005;36(4):307–314. doi: 10.1002/lsm.20148.
- Karu T. Photobiology of low-power laser effects. Health Phys. 1989;56(5):691–704. doi: 10.1097/00004032-198905000-00015.
- Leavitt M, Charles G, Heyman E, et al. HairMax LaserComb laser phototherapy device in the treatment of male androgenetic alopecia: a randomized, double-blind, sham device-controlled, multicentre trial. Clin Drug Investig. 2009;29(5):283–292. doi: 10.2165/00044011-200929050-00001.
- Bjordal JM, Couppé C, Chow RT, et al. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003;49(2):107–116. doi: 10.1016/s0004-9514(14)60127-6.
- Wahl G, Bastänier S. [Soft laser in postoperative care in dentoalveolar treatment]. ZWR. 1991;100(8):512–515.


