Abstract
Q-switched neodymium-yttrium aluminum-garnet (Q-switched Nd:YAG) laser has been reported as an effective treatment for nevus of Ota and acquired bilateral nevus of Ota-like macules (ABNOM). Data on ectopic Mongolian spots have rarely been reported.
The present study was performed to investigate the treatment efficacy of a high-fluence 1064 nm Q-switched Nd:YAG laser without tissue whitening in ectopic Mongolian spots.
We included 61 patients with ectopic Mongolian spots, and 70 lesions were examined. Thirty-three lesions were treated with a high-fluence 1064 nm Q-switched Nd:YAG laser, and 38 lesions were observed without treatment. The results were assessed using a 5-quantile grading scale and melanin index using a Mexameter®.
Mean follow-up duration was 14.1 ± 6.8 months for the treatment group and 17.8 ± 10.0 months for the observation group. Mean 5-quintile grading scale at final follow-up was statistically different (p < 0.001) between the two groups (treatment: 2.85 ± 1.00, observation: 0.49 ± 0.73). There was a significant difference (p < 0.001) in the Δ melanin index (initial melanin index – final melanin index) between the observation (7.1 ± 62.7) and treatment (156.7 ± 78.4) groups.
High-fluence Q-switched Nd:YAG laser without tissue whitening showed good results and was well-tolerated in treating ectopic Mongolian spots.
Introduction
Mongolian spots are another name for dermal melanocytosis, usually characterized by a grayish-blue color and a variety of shapes and sizes (Citation1). They are very common in Asian and African populations but are relatively rare in Caucasian children and usually fade as the patient grows older. Most are located in the lumbosacral area; those located in the extrasacral area are called ectopic Mongolian spots (EMS) (Citation2). Typical Mongolian spots in the lumbosacral region are generally unnoticeable after 1–4 years, and eventually disappear completely (Citation3). Only 3–4% of typical Mongolian spots remain after this time, especially in Asian populations (Citation4). EMS are more likely to persist than typical sacral Mongolian spots (Citation5, Citation6). They have a benign course; however, patients with EMS in exposed areas can experience psychological distress because of the cosmetic appearance.
The Q-switched neodymium-yttrium aluminum-garnet (Q-switched Nd:YAG) laser has been reported as an effective treatment for the nevus of Ota and acquired bilateral nevus of Ota-like macules (ABNOM) (Citation7, Citation8). A few case reports have been published recently on the 1064 nm Q-switched Nd:YAG laser for the treatment of EMS (Citation9). However, no large-scale studies have been published to date.
In this study, we investigated the treatment efficacy of a high-fluence 1064 nm Q-switched Nd:YAG laser for EMS.
Materials and methods
Study population and study design
This retrospective study was performed between September 2013 and August 2018. We enrolled 61 patients who were clinically diagnosed with EMS and visited the dermatology department of the Pusan National University Hospital (Busan and Yangsan). Seventy ectopic Mongolian spot lesions were assessed in 61 patients. Thirty-three lesions were treated with a 1064 nm Q-switched Nd:YAG laser and the remaining 38 lesions were observed without treatment. None of the patients had a previous treatment history.
Treatment protocol
A 1064 nm Q-switched Nd:YAG laser (Spectra VRMIII®; Lutronic Corp., Seoul, South Korea) was used for 33 lesions. A fluence of 2.0–2.4 J/cm2, spot size of 7 mm, and 10-Hz repetition rate by sliding technique was used to treat the EMS. The fluence of the laser was adjusted according to the patient’s clinical response to previous treatment. The therapeutic endpoint was that the lesions showed minimal erythema without petechiae.
One hour before the treatment, topical anesthetic cream (a mixture of 2.5% lidocaine and 2.5% prilocaine; AstraZeneca AB, Soderatalje, Sweden) was applied to the skin over the EMS. The treatment sessions were continued at 4-week intervals.
Objective assessment of treatment efficacy
We took photographs of patients at every visit using the same camera and lighting. The objective assessment of clinical response was performed by three independent dermatologists by comparing post-treatment with baseline photographs at each treatment session. The improvements after each treatment session were evaluated based on the following 5-quantile grading scales: poor (less than 25%) improvement; fair (25–49%) improvement; good (50–74%) improvement; excellent (75–94%) improvement; and complete (>95%) improvement.
The melanin index was measured using a Mexameter® (MX18, CK electronic GmbH, Germany) during each session. The average melanin index was measured four times in the lesion area of the darkest pigmentation.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., NY, USA). For data comparison between the two groups, the t-test or Fisher’s exact test was performed. Continuous variables are presented as mean ± standard deviation, and p values <0.05 were considered statistically significant.
The study was approved by the Institutional Review Board of the Pusan National University Yangsan Hospital (IRB No. 05-2022-079), and all patients or their parents signed informed consent forms for the study.
Results
The demographic and clinical data of the patients are summarized in . A total of 61 patients (20 male and 41 female) with EMS were enrolled in this study. The mean age of the patients was 16.2 months (range: 2–84 months). Seventy EMS lesions were observed in 61 patients. The most common sites were the extremities (72.9%), including the lower (42.9%) and upper limbs (30.0%). The mean follow-up duration was 16.1 months (range: 5–34 months). In the treatment group, the average number of laser treatment sessions was 10.3 ± 4.9, and the mean duration of treatment was 14.1 months. The total duration of treatment was determined based on clinical improvement and parental satisfaction.
Table 1. Demographics and clinical features of patients with ectopic Mongolian spots.
The treatment responses are summarized in . A representative image of the treatment group is shown in . In the treatment group, approximately 70% of patients showed good or excellent improvement after the final session; 14 patients (42.4%) showed 76–95% clearance, and 9 patients (27.3%) showed greater than 95% improvement. In contrast, 64.9% of patients in the observation group showed poor improvement during the follow-up period. In addition, the melanin indices measured using the Mexameter® showed significant reductions after laser treatment. The average melanin index reduction at the final visit was 156.7 ± 78.4 in the treatment group and 7.5 ± 63.6 in the observation group (p < 0.001). In the treatment group, both the degree of improvement and the melanin index reduction were better than those of the observation group during the follow-up period ().
Figure 1. Excellent improvement of ectopic Mongolian spot after 1064 nm Q-switched Nd:YAG laser treatment. Case 1. Before (A) and 6 months after laser treatments (B), 12 months after laser treatments (C), 18 months after laser treatment (D) [number of total treatment sessions: 12]; case 2. Before (E) and 6 months after laser treatments (F), 12 months after laser treatments (G) [number of total treatment sessions: 10].
![Figure 1. Excellent improvement of ectopic Mongolian spot after 1064 nm Q-switched Nd:YAG laser treatment. Case 1. Before (A) and 6 months after laser treatments (B), 12 months after laser treatments (C), 18 months after laser treatment (D) [number of total treatment sessions: 12]; case 2. Before (E) and 6 months after laser treatments (F), 12 months after laser treatments (G) [number of total treatment sessions: 10].](/cms/asset/9dca9d0a-b504-4429-a9dd-1b812e4b011e/ijdt_a_2255057_f0001_c.jpg)
Figure 2. The degree of improvement of 5-quantile grading scale (A) and the change of the melanin index (B) in both treatment group and observation group.
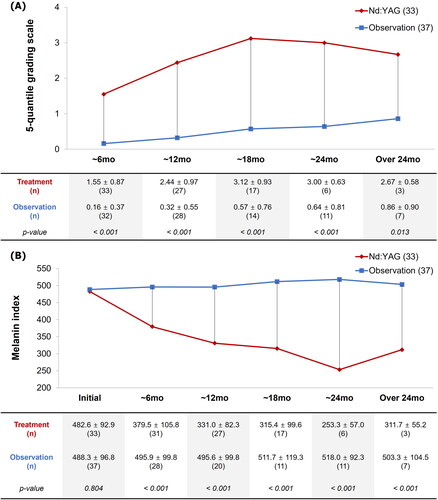
Table 2. Final 5-quantile grading scale and change in melanin index.
In this study, we encountered two lesions (6.1%) that scarred or blistered after laser treatment. These two lesions were very dark at presentation, with initial melanin indices of 637 and 602, respectively. All other side effects, including mild pain and edema, were as expected.
Discussion
Mongolian spots usually disappear as the patient grows, but occasionally, this does not occur, and they persist for a long time. If the spot is not in a typical location, like the buttock, or if it is darkly pigmented, it is more likely to persist and has a lower chance of spontaneous regression compared to a typical sacral Mongolian spot (Citation4–6). In addition, when EMS is in an exposed area, it can cause cosmetic concerns and interfere with socialization. With active treatment, it disappears earlier than it does in the natural course. The optimal timing of treatment has not yet been established. Several previous studies have reported that early treatment is better because the skin is thinner and has less pigment at an early age, resulting in better laser penetration (Citation10).
EMS treatment has not yet been established. Various treatment modalities have been explored for EMS, such as the Q-switched alexandrite laser (Citation11), Q-switched Ruby laser (Citation12), and intense pulsed light (Citation13). Several recent case reports have had good results with the 1064 nm Q-switched Nd:YAG laser (Citation9). We used a high-fluence 1064 nm Q-switched Nd:YAG laser to treat EMS. Our laser-treated patients showed better responses than the observation group. The proportion of lesions showing excellent or complete improvement in the laser treatment group was approximately 70%. In contrast, many cases in the observation group showed poor to fair improvement.
The mechanism of a high-fluence 1064 nm Q-switched Nd:YAG laser in the treatment of EMS is still unclear. It is thought to be a principle of selective photothermolysis, similar to that of Ota’s nevus (Citation14, Citation15). Through repetitive treatment sessions, its mechanism of action is to get rid of protective extracellular fibrous sheath which envelopes dermal melanocytes, instead of directly destroying dermal melanocytes. This can result in increased melanocyte apoptosis and indirectly destroy dermal melanocytes. EMS can be treated with minimal damage to the surrounding skin, resulting in less scarring.
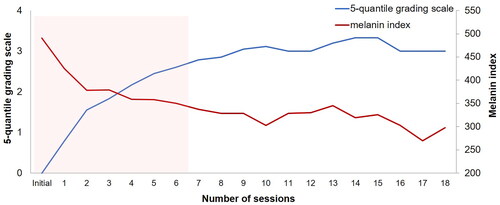
In the treatment group, the average improvement scale and melanin index according to the number of treatment sessions showed significant changes within the initial six treatments (). In addition, the average number of laser treatments required to show excellent improvement and complete improvement was 6.46 and 9.57 times, respectively. In the observation group, most patients showed less than 50% improvement, and no patients showed more than 75% improvement during the follow-up of 17.8 months. Since studies on the natural course of EMS are lacking, this study emphasized that the treatment group showed more improvements than the observation group.
Figure 3. Progress of average melanin index and 5-quantile grading scale according to the number of treatment sessions.
Complications following laser treatment, including hyperpigmentation and edema, were mild and transient in a few patients. One lesion blistered and one had scarring. Both lesions had high initial melanin indices (>600) compared to the average index observed (485.6). Prominently hyperpigmented EMS lesions contain a large number of melanocytes, which can cause strong reactions even with a low laser energy output. Therefore, if the initial color of the EMS is noticeably dark, a careful approach with a lower fluence rate is required.
In pediatric treatment, it is very important to increase compliance with proper pain control. Because conventional high-fluence Q-switched Nd:YAG lasers cause pain, it is difficult to treat children repeatedly. In addition, conventional high-fluence 1064 nm Q-switched Nd:YAG laser therapy with tissue whitening may cause purpura, crust, post-inflammatory hyperpigmentation, and scarring. In this study, a high-fluence 1064 nm Q-switched Nd:YAG laser therapy without tissue whitening was used so that treatment could be less painful and better tolerated. High-fluence Q-switched Nd:YAG laser treatment without tissue whitening EMS is also easy to manage post-treatment because of the short treatment downtime, with no post-treatment petechiae or crust formation.
This study has some limitations. This is a retrospective study with a small sample size. Assessment was based solely on clinical grounds, not on histopathological or electron microscopic features of the lesions. Although EMS may fade spontaneously, the clinical course compared with that of the observation group supports the role of a high-fluence 1064 nm Q-switched Nd:YAG laser for EMS.
We suggest that a high-fluence 1064 nm Q-switched Nd:YAG laser achieved good results in the treatment of EMS. It is well tolerated in children, with less pain than other treatments and minimal downtime. The therapeutic effect increased steeply during the first six treatment sessions. Reducing post-treatment complications requires a careful approach with lower fluence, especially for prominently hyperpigmented lesions before treatment. Future studies with larger samples and comparisons with conventional 1064 nm Q-switched Nd:YAG laser are needed.
Ethical approval
The study was approved by the ethics committee (05-2022-079).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Cordova A. The Mongolian spot: a study of ethnic differences and a literature review. Clin Pediatr. 1981;20(11):1–5. doi: 10.1177/000992288102001105.
- Kikuchi I, Inoue S. Natural history of the Mongolian spot. J Dermatol. 1980;7(6):449–450. doi: 10.1111/j.1346-8138.1980.tb02000.x.
- Schachner L, Hansen R, Krafchik B, et al. Pediatric dermatology. 4th ed. London: Elsevier; 2010.
- Leung AK. Mongolian spots in Chinese children. Int J Dermatol. 1988;27(2):106–108. doi: 10.1111/j.1365-4362.1988.tb01282.x.
- Cole HN, Jr., Hubler WR, Lund HZ. Persistent, aberrant Mongolian spots. Arch Derm Syphilol. 1950;61(2):244–260. doi: 10.1001/archderm.1950.01530090074007.
- Leung AK, Kao CP, Leung AA. Persistent Mongolian spots in Chinese adults. Int J Dermatol. 2005;44(1):43–45. doi: 10.1111/j.1365-4632.2004.02011.x.
- Hur H, Park CH, Kim YR, et al. The treatment of ota’s nevus using Dr. Hoon Hur’s golden parameter with a high fluence 1064 nm Nd: YAG laser without side effects. J Dermatol Res Ther. 2017;3(2):1–4. doi: 10.23937/2469-5750/1510047.
- Hur H, Kim YR. The treatment of hori’s nevus by new combination treatment without side effects: Dr. Hoon Hur’s golden parameter therapy and Dr. Hoon Hur’s optimal melanocytic suicide-2 parameter therapy. Clin Res Dermatol. 2017;4(5):1–5. doi: 10.15226/2378-1726/4/5/00171.
- Kim JYKWS. Beneficial effect of early treatment of aberrant Mongolian spots with 1,064-nm Q-switched neodymium-doped yttrium-aluminum-garnet laser. Lasers Med; Eng, Basic Res Clin Appl. 2017;6(2):99–101.
- Suzuki H, Anderson RR. Treatment of melanocytic nevi. Dermatol Ther. 2005;18(3):217–226. doi: 10.1111/j.1529-8019.2005.05021.x.
- Kagami S, Asahina A, Uwajima Y, et al. Treatment of persistent Mongolian spots with Q-switched alexandrite laser. Lasers Med Sci. 2012;27(6):1229–1232. doi: 10.1007/s10103-012-1113-4.
- Shirakawa M, Ozawa T, Ohasi N, et al. Comparison of regional efficacy and complications in the treatment of aberrant Mongolian spots with the Q-switched ruby laser. J Cosmet Laser Ther. 2010;12(3):138–142. doi: 10.3109/14764172.2010.487907.
- Shirakawa M, Ozawa T, Tateishi C, et al. Intense pulsed light therapy for aberrant Mongolian spots. Osaka City Med J. 2012;58(2):59–65. https://www.ncbi.nlm.nih.gov/pubmed/23610848.
- Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524–527. doi: 10.1126/science.6836297.
- Anderson RR, Margolis RJ, Watenabe S, et al. Selective photothermolysis of cutaneous pigmentation by Q-switched Nd: YAG laser pulses at 1064, 532, and 355 nm. J Invest Dermatol. 1989;93(1):28–32. doi: 10.1111/1523-1747.ep12277339.

