Abstract
Background
Nevus depigmentosus (ND) is one of the pigmentary conditions that is characterized by a hypopigmented patch with an irregular border. It is usually present at birth or shortly after birth. It is not a progressive condition, but it may increase in size in proportion to the growth of the body. Despite many treatment modalities, there is no effective treatment for this condition.
Objective
To review all articles about the treatment options for ND.
Methods
Pubmed database were searched for this study, and relative clinical trials were included in the review. Descriptive findings, including age, gender, and treatment modality and response, were reported.
Results
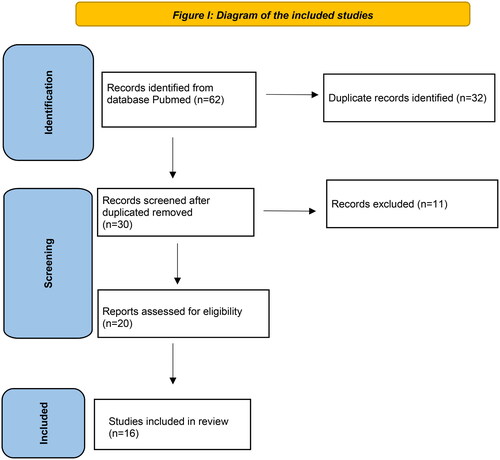
A total of 62 articles were identified, and 16 relevant articles were included in this review after screening and removing the duplicates.
Conclusion
In the literature, a limited number of treatment modalities have been employed for ND. Among these, surgical interventions and phototherapy have been the most commonly studied, but their efficacy has varied. Unfortunately, there is no definitive cure for ND, and recurrence of the lesion is not an uncommon occurrence even after complete clearance. Furthermore, there is a dearth of large-scale clinical studies that comprehensively analyze the different treatment modalities for ND.
Introduction
Nevus depigmentosus (ND) is an uncommon congenital hypopigmentary disorder characterized by focal, stable, well-defined hypopigmented lesions with irregular borders [Citation1]. These lesions are most commonly observed on the trunk, extremities, and face [Citation2]. It typically presents at birth or shortly thereafter and tends to remain stable throughout the patient’s life [Citation3]. The exact pathogenesis is unknown, but the proposed etiopathogenesis is a transportation defect from melanocyte to keratinocyte [Citation2,Citation4,Citation5].
Despite the lack of an effective treatment for ND, various treatment modalities have been attempted, including phototherapy and surgical intervention [Citation6]. The results are variable and there is no consensus regarding the treatment of choice for this condition. Here we review the literature about the modalities of treatment for ND.
Methods
A thorough literature search was conducted on Pubmed to assess all published studies in the English language from the earliest available date up to February 28th, 2023. The search terms used were pre-identified and included ‘nevus depigmentosus,’ ‘nevus achromicus,’ ‘achromic nevus,’ ‘treatment,’ and ‘therapy.’ Non-English papers without any available translations were excluded from the analysis.
Results
Our search yielded a total of 62 articles. After removing duplicates, animal studies, and articles that did not include therapy, we included a total of 16 articles (). Upon applying these exclusions, 18 studies met the inclusion criteria. The characteristics of these studies are presented in (). Given the rarity of ND, the majority of the studies were comprised of case reports or case series. There are a few retrospective and prospective studies but they included patients with other diseases like vitiligo ().
Table 1. Characteristics of ND treatment modality studies.
Surgical interventions
In the existing literature, surgical intervention is the most frequently employed approach for the treatment of ND. The technique used was either MKTP or tissue grafting via suction blister.
Non-cultured melanocyte-keratinocyte transplantation (MKTP)
One study examined the efficacy of MKTP in treating six patients with ND, with varying outcomes [Citation6]. In this study, while two patients showed limited improvement, three experienced significant repigmentation. Notably, the treatment plan included excimer laser therapy, and one patient experienced recurrence later. In another case study, they injected the melanocyte-keratinocyte suspension in the created blister in the recipient area [Citation7]. It was followed by solar ultraviolet A (UVA) and showed 80% of repigmentation. Other case reports used MKTP solely and showed variable results ranging from poor to excellent hyperpigmentation [Citation2,Citation8–10]. However, none of these studies reported the recurrence rate during long-term follow-up.
Suction blister grafting
The available literature on this treatment modality consists solely of case reports. In one report, the ND was treated by tissue graft harvested using suction blister followed by topical psoralen plus ultraviolet A of solar origin (PUVASOL) [Citation1]. The repigmentation was excellent with no recurrence after 10 years of follow-up. In another report, the used tissue graft harvested using suction blister too but added oral 4,5,8-trimethylpsoralen instead of topical treatment [Citation11]. The patient had good repigmentation that was limited only to the grafted area, with no repigmentation in the intergraft areas. Other case reports using suction blister grafting reported satisfactory repigmentation with one case of recurrence after 8 years while others did not report the recurrence rate [Citation12–14].
Phototherapy
There is a scarcity of literature examining the effectiveness of phototherapy as a standalone treatment for ND. The largest study to date was a retrospective analysis that included 14 patients who underwent excimer laser treatment [Citation15]. The study revealed complete repigmentation in more than 70% of the patients, and of the six patients who were monitored for six months, four experienced a recurrence of hypopigmentation. Other studies used excimer laser and narrowband ultraviolet B (NBUVB). These studies were all case reports and the repigmentation was significant [Citation3,Citation16,Citation17].
Other therapies
There is only one study that included one patient who was treated with topical and oral steroids [Citation18]. The patient was having ND coexistent with vitiligo. After eight weeks of treatment, ND did not improve.
Discussion
Due to its rarity, there is a paucity of large-scale studies on ND, and most previous reports comprise either case reports or case series. Surgical interventions have been the most commonly used modalities in the literature. Although many reports have shown positive outcomes, there are concerns regarding the use of this modality. The primary concern associated with surgical interventions for ND is the potential for hypopigmentation recurrence after a few months post-procedure. While several reports in the literature have not commented on the recurrence rate, only a few have reported the incidence of recurrence within the study population [Citation6,Citation14]. This may limit the use of this procedure in the treatment of ND. Gupta and Goel proposed that the use of skin grafts may result in superior pigmentation outcomes compared to cellular grafts [Citation11]. Their explanation is grounded in the potential for abnormal keratinocyte functionality, which can impede the transfer of melanosomes from transplanted melanocytes. In their case report, the intergraft area did not exhibit pigmentation, which may further support their theory. Another concern in this modality is the color mismatch which was reported significantly in a case series [Citation6].
Phototherapy has been utilized in several reports with satisfactory outcomes. However, all of these reports employed the excimer laser except for one, which utilized NBUVB [Citation3,Citation15–17]. In one retrospective study, four out of six followed patients reported loss of pigmentation after three to six months [Citation15]. This observation has also been noted in the patient who was treated surgically, which can lead to unsatisfactory long-term treatment outcomes for ND. Some of the reports combine surgical intervention with phototherapy with satisfactory results [Citation6,Citation7,Citation11].
In conclusion, the current literature on the treatment of ND is limited. While surgical interventions hold promise as a treatment modality, the possibility of recurrence remains a concern. Phototherapy has also shown promising results, particularly when used in conjunction with surgical therapy. However, more extensive studies are necessary to determine the most effective treatment option for this condition.
Disclosure statement
No potential conflict of interest was reported by the author.
Additional information
Funding
References
- Kar BR. Nevus depigmentosus treated with suction blister grafting: follow-up after 10 years. Indian J Dermatol. 2013;58(2):1. doi: 10.4103/0019-5154.108074.
- Sritanyarat T, Wongpraparut C, Jansuwan N, et al. Outcomes of autologous non-cultured melanocyte keratinocyte transplantation in vitiligo and nevus depigmentosus. J Dermatolog Treat. 2022;33(2):935–4. doi: 10.1080/09546634.2020.1793885.
- Zeng Q, Shi Q, Huang J, et al. Facial nevus depigmentosus getting remarkable repigmentation by treatment with a 308-nm excimer laser: a case report. Dermatol Ther. 2018;31(5):e12662. doi: 10.1111/dth.12662.
- Xu AE, Huang B, Li YW, et al. Clinical, histopathological and ultrastructural characteristics of naevus depigmentosus. Clin Exp Dermatol. 2008;33(4):400–405. doi: 10.1111/j.1365-2230.2008.02714.x.
- Ullah F, Schwartz RA. Nevus depigmentosus: review of a mark of distinction. Int J Dermatol. 2019;58(12):1366–1370. doi: 10.1111/ijd.14393.
- Mulekar SV, Al Issa A, Al Eisa A. Nevus depigmentosus treated by melanocyte-keratinocyte transplantation. J Cutan Aesthet Surg. 2011;4(1):29–32. doi: 10.4103/0974-2077.79185.
- Gauthier Y, Surleve-Bazeille JE. Autologous grafting with noncultured melanocytes: a simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26(2 Pt 1):191–194. doi: 10.1016/0190-9622(92)70024-a.
- Olsson MJ, Juhlin L. Leucoderma treated by transplantation of a basal cell layer enriched suspension. Br J Dermatol. 1998;138(4):644–648. doi: 10.1046/j.1365-2133.1998.02177.x.
- van Geel N, Wallaeys E, Goh BK, et al. Long-term results of noncultured epidermal cellular grafting in vitiligo, halo naevi, piebaldism and naevus depigmentosus. Br J Dermatol. 2010;163(6):1186–1193. doi: 10.1111/j.1365-2133.2010.10014.x.
- Raskovic D, Bondanza S, Gobello T, et al. Autologous in vitro reconstituted epidermis in the treatment of a large nevus depigmentosus. J Am Acad Dermatol. 2006;54(5 Suppl):S238–S40. doi: 10.1016/j.jaad.2005.08.013.
- Gupta S, Goel A. Letter to the editor: nevus depigmentosus needs transplant of epidermal sheets. Dermatol Surg. 2005;31(12):1746–1747. doi: 10.2310/6350.2005.31327.
- Ravikumar BC, Sabitha L, Balachandran C. Naevus depiomentosus treated with suction blister grafting. Indian J Dermatol Venereol Leprol. 2000;66(2):89–90.
- Ashique KT, Kaliyadan F. Is blister grafting an acceptable answer to treating nevus depigmentosus? Int J Dermatol. 2019;58(5):e95–e96. doi: 10.1111/ijd.14354.
- Kim DY, Park YK, Hann SK. Recurrence of nevus depigmentosus after an autologous epidermal graft. J Am Acad Dermatol. 2008;58(3):527–529. doi: 10.1016/j.jaad.2006.09.018.
- Bae JM, Jung HM, Chang HS, et al. Treatment of nevus depigmentosus using the 308-nm excimer laser: a retrospective study of 14 patients. J Am Acad Dermatol. 2016;75(3):626–627. doi: 10.1016/j.jaad.2016.04.002.
- Hwang SW, Kang JH, Jung SY, et al. Vitiligo coexistent with nevus depigmentosus: this was treated with narrow-band UVB and these lesions were followed using the mexameter®, a pigment-measuring device. Ann Dermatol. 2010;22(4):482–485. doi: 10.5021/ad.2010.22.4.482.
- Kim DY, Lee KY, Park YK. Use of the 308-nm excimer laser for nevus depigmentosus: a promising treatment for either nevus depigmentosus or vitiligo. J Dermatol. 2007;34(3):217–218. doi: 10.1111/j.1346-8138.2007.00254.x.
- Kang IK, Hann SK. Vitiligo coexistent with nevus depigmentosus. J Dermatol. 1996;23(3):187–190. doi: 10.1111/j.1346-8138.1996.tb03995.x.