Abstract
Immunoglobulin gamma (IgG) type 4–related disease (IgG4-RD) is a chronic immunologic systemic disorder that could affect multiple organs, which may cause irreversible organ damage or even death. Skin involvement is rare and associated especially with systemic disease. The dermatologist must be equipped to recognize IgG4-RD to prevent delayed identification and treatment. This case reports a very rare case of IgG4-related skin disease (IgG4-RSD) presenting with a generalized angiolymphoid hyperplasia with eosinophilia (ALHE)-like lesions in a middle-aged male patient with no other organ involvement. He was treated with oral glucocorticoid and cyclophosphamide, which resulted in complete remission. No relapse and disease progression were seen with a follow-up for 8 years.
Case presentation
A 56-year-old male presented with a 12-year history of enlarging and pruritic dorsonasal plaques and 2-year history of multiple erythematous papulonodular lesions of different sizes on the trunk and limbs (). Intermittent treatment with topical corticosteroids and oral antihistamine drugs had failed to improve his clinical condition. The patient’s condition was in general normal. He had no known allergies, and denied history of trauma, fever or weight loss. Clinical examination revealed scattered red plaques, papules and nodules on his face, limbs, and trunk. Enlarged lymph node on the axilla and the groin was palpable and could move freely over the bridge. There was no swelling in the eyelids and submandibular region; Oculomotricity and visual acuity were normal.
Figure 1. Clinical examination revealed scattered red plaques, papules and nodules on his face (a), limbs (C,D), and trunk (B,C).

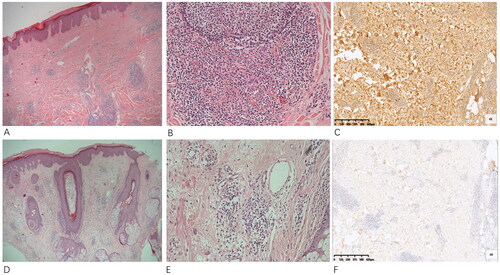
A blood routine examination revealed a significantly increase in the level of serum IgG4 compared with normal range limits (>4.040 g/L; normal range, 0.03–2.01g/l), a mild increase in eosinophilia (0.57*109/L) and a significantly increase in IgE (2036 UI/ml). Renal function, liver transaminase, and lactate dehydrogenase levels were normal; serum immunofixation electrophoresis did not reveal monoclonal gammopathy; serum and urine kappa/lambda light chain ratio was normal. Antinuclear autoantibodies were negative. Ultrasound images revealed lymphadenopathy of the axillary and inguinal regions, and the largest measuring 3.3 × 1.0 cm in diameter. Bone marrow aspirate did not demonstrate an excess of plasma cells or blasts. Chest RX and abdominal ultrasound did not reveal any pancreatic, biliary, or renal abnormality. Two biopsy specimens () obtained from the bridge of the nose and back displaying similar histopathologic features of numerous vascular proliferation with cuboidal endothelium in the dermis, a lymphohistiocytic infiltrate with eosinophil and plasma cell accumulation, and moderately increased dermal collagen. The specimen obtained from the back also revealed one lymphoid follicle with distinct germinal centers in the superficial and middle dermis. Immunohistochemical studies of the back lesion revealed that the infiltrate was positive for CD2, CD3, CD4, CD5, CD19, CD20, CD34 and CD138. Rare CD8+ T cells and CD30+ T cells were also identified. Clonal TCR gene rearrangement of the skin lesion was negative. Biopsy of an enlarged lymph node in the right groin showed the pattern of dermatopathic lymphadenitis with an eosinophil infiltrate. These clinical and histogical findings were more similar to those of ALHE. But in ALHE, the lesions are most common in the head-neck region [Citation1], diffuse skin lesions all over the body was unusual. In addition, the increased serum IgG4 level and the multifocal distribution of plasma cells made the diagnose of IgG4-related skin disease should be considered. Further immunohistochemically study showed that most of the infiltrated plasma cells were positive for IgG4, with an IgG4+/IgG + ratio of approximately 40% and the number of IgG4 + plasma cells per high-power field > 50. Therefore, a final diagnosis of IgG4-related skin disease was made according to the 2020 revised comprehensive diagnostic (RCD) criteria for IgG4-RD [Citation2]- organ involvement, serum IgG4 levels >135 mg/dl, dense lymphocyte and plasma cell infiltration with fibrosis, ratio of IgG4-positive plasma cells/IgG-positive cells greater than 40% and the number of IgG4-positive plasma cells greater than 10 per high powered field. Treatment with oral prednisone (30 mg/d) and cyclophosphamide (50 mg/d) was started. The patient improved within 2 weeks, with marked reduction of both skin lesions and clinical symptoms, with no adverse effects. After 2 months of treatment, the dose of oral prednisone reduced gradually. After a follow-up of 8 years, the patient remained in complete remission after withdrawal of prednisolone and no relapse was seen with continuous cyclophosphamide monotherapy. Surprisingly, he remained healthy with no additional signs or symptoms of systemic involvement.
Figure 2. Histopathology of the back specimen (A,B) and the nose specimen (D,E) revealed a lymphohistiocytic infiltrate with eosinophil and plasma cell accumulation with numerous vessels. Immunoperoxidase staining for IgG (C) and IgG4 (F) shows more than 50 positively staining plasma cells per high-powered field with an IgG to IgG4 ratio close to 40%.
Discussion
IgG4-RD is an immune-mediated disorder characterized by elevated levels of circulating IgG4, and tissue infiltration of IgG4+ plasma cells. The disease typically affects the middle‐aged to elderly people with clinical symptoms depending on lesion location [Citation3,Citation4]. It has been found that skin is the potential isolated involvements in the disease [Citation5,Citation6]. Tokura et al. [Citation7]. have divided the skin lesions into primary eruptions with massive plasma‐cell infiltrates and secondary eruptions without mass formation by plasma cells. The primary eruptions consisted of cutaneous plasmacytosis, pseudolymphoma, ALHE and Mikulicz disease. No reports of an IgG4-RSD, presenting with generalized ALHE-like eruptions are available to date, to the best of our knowledge.
The diagnosis of IgG4-RD is often challenging because it can mimic various diseases, including inflammatory, malignancy, infection, or other immune-mediated conditions [Citation8,Citation9].
The diagnosis of IgG4-RD should be considered in any eruption containing polytypic and abundant plasma cells either with or without an eosinophilic infiltrate and fibrosis. Like our experience, sometimes IgG4-RSD are confusingly similar in appearance and histology to ALHE [Citation10,Citation11], But in a small group study from Yasuhito et al. [Citation10], IgG4-positive plasma cell infiltration was not observed in tissues from patients with ALHE. Thus, in our case, a dense plasmacytic infiltrate of IgG4+ plasma cells (>50 per HPF) and the high IgG4+/IgG + ratio (approximately 40%) were in keeping with a diagnosis of IgG4-RD.
Our case with literature review suggests that skin lesions can be an isolated lesion or primary involvement of systemic IgG4-RD [Citation5], with an average time to development of systemic disease of 4 years [Citation1]. Peripheral blood eosinophilia and increased serum IgE concentrations occur in almost 30% of patients with IgG4-RD [Citation7]. In patients with IgG4-related skin disease, lesions were frequently present on the skin of the periauricular, cheek, and mandible regions, and were frequently accompanied by IgG4-related lymphadenopathy [Citation12]. Histologically, IgG4-RD is characterized by 3 main features: dense lymphoplasmacytic infiltration with the predominance of IgG4 positive plasma cells, storiform fibrosis, and obliterative phlebitis. There are some pathological differences among organs. In IgG4-related skin disease, plasmacyte infiltration and storiform fibrosis are prominent, but obliterative phlebitisis is less marked in skin lesions [Citation3].
There are multiple ways to manage immunoglobulin G4-related disease (IgG4-RD), including treatment with glucocorticoids (GCs), immunosuppressive drugs (such as disease modifying anti-rheumatic drugs, azathioprine, mycophenolate mofetil, methotrexate, leflunomide, tacrolimus, ciclosporin A, iguratimod, and cyclophosphamide), or biologic agents (such as rituximab, abatacept, infliximab, and dupilumab)[Citation8]. However, relapse is frequently seen on drug withdrawal [Citation8,Citation13]. An Chinese prospective clinical trial showed a reduced relapse rate at one year when oral cyclophosphamide (50–100 mg/day) was added to low dose corticosteroids, compared with steroid treatment alone [Citation13]. Based on a review of literature and our own experience, GCs combined with cyclophosphamide seemed to be particularly effective for maintenance treatment in an effort to minimize disease relapse.
IgG4-RSD have not been as widely studied as those in other organs. There should be more research to explore the relationship between ALHE and ALHE-like IgG4-RSD.
No conflict of interests to declare
Authors declare no conflict of interests for this article.
Patient consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Additional information
Funding
References
- Adler BL, Krausz AE, Minuti A, et al. Epidemiology and treatment of angiolymphoid hyperplasia with eosinophilia (ALHE): a systematic review. J Am Acad Dermatol. 2016;74(3):1–4. doi:10.1016/j.jaad.2015.10.011.
- Umehara H, Okazaki K, Kawa S, et al. The 2020 revised comprehensive diagnostic (RCD) criteria for IgG4-RD. Mod Rheumatol. 2021;31(3):529–533. doi:10.1080/14397595.2020.1859710.
- Bennett AE, Fenske NA, Rodriguez-Waitkus P, et al. IgG4-related skin disease may have distinct systemic manifestations: a systematic review. Int J Dermatol. 2016;55(11):1184–1195. doi:10.1111/ijd.13369.
- Umehara H, Okazaki K, Kawano M, et al. How to diagnose IgG4-related disease. Ann Rheum Dis. 2017;76(11):e46–e46. doi:10.1136/annrheumdis-2017-211330.
- Ingen-Housz-Oro S, Ortonne N, Elhai M, et al. IgG4-related skin disease successfully treated by thalidomide: a report of 2 cases with emphasis on pathological aspects. JAMA Dermatol. 2013;149(6):742–747. doi:10.1001/jamadermatol.2013.2625.
- Hegde P, Relhan V, Tomar R. IgG4-related disease: a rare case of isolated cutaneous involvement. Clin Exp Dermatol. 2021;46(2):343–345. doi:10.1111/ced.14334.
- Tokura Y, Yagi H, Yanaguchi H, et al. IgG4-related skin disease. Br J Dermatol. 2014;171(5):959–967. doi:10.1111/bjd.13296.
- Lanzillotta M, Mancuso G, Della-Torre E. Advances in the diagnosis and management of IgG4 related disease. BMJ. 2020;369:m1067. doi:10.1136/bmj.m1067.
- Liu Z, Nie Y, Peng Y, et al. The external validation of the 2019 ACR/EULAR classification criteria for IgG4-related disease in a large cohort from China. Semin Arthritis Rheum. 2023;61:152202. doi:10.1016/j.semarthrit.2023.152202.
- Hamaguchi Y, Fujimoto M, Matsushita Y, et al. IgG4-related skin disease, a mimic of angiolymphoid hyperplasia with eosinophilia. Dermatology. 2011;223(4):301–305. doi:10.1159/000335372.
- Fernandez-Flores A, Cassarino DS. Three unusual histopathological presentations of angiolymphoid hyperplasia with eosinophilia. J Cutan Pathol. 2017;44(3):300–306. doi:10.1111/cup.12886.
- Sato Y, Takeuchi M, Takata K, et al. Clinicopathologic analysis of IgG4-related skin disease. Mod Pathol. 2013;26(4):523–532. doi:10.1038/modpathol.2012.196.
- Yunyun F, Yu C, Panpan Z, et al. Efficacy of cyclophosphamide treatment for immunoglobulin G4-related disease with addition of glucocorticoids. Sci Rep. 2017;7(1):6195. doi:10.1038/s41598-017-06520-5.

