ABSTRACT
A large proportion of stroke patients are unable to return to work (RTW), although figures vary greatly. A total of 121 mild-to-moderate stroke patients, who had a paid job at the time of their stroke were included (a) to quantify RTW and work satisfaction one-year post-stroke (using the Utrecht Scale for Evaluation of Rehabilitation-Participation) and (b) to determine factors predicting RTW post-stroke, based on stroke-related, personal and neuropsychological variables. Half of the patients were not in work (28%) or were working less (22%) than pre-stroke. Ninety percent of those in fulltime employment post-stroke were satisfied with their occupational situation, against 36% of the unemployed participants. In regards to factors predicting RTW, global cognitive functioning (r = .19, Montreal Cognitive Assessment) and depressive symptoms (r = −.16, Hospital Anxiety and Depression Scale) at two months post-stroke onset were associated with return to work within one year. Only global cognitive functioning was an independent predictor of RTW (11.3% variance, p = .013). Although the explained variance was not that high, neuropsychological factors probably play a pivotal role in returning to work and should be taken into account during rehabilitation after mild and moderate stroke.
Introduction
Employment is regarded as one of the most important predictors of quality of life (Donker-Cools, Wind, & Frings-Dresen, Citation2015; Passier, Visser-Meily, Rinkel, Lindeman, & Post, Citation2011; van Velzen, van Bennekom, Edelaar, Sluiter, & Frings-Dresen, Citation2009b). People who are employed report a better quality of life, less health service usage and a better health status than non-employed people (van Velzen et al., Citation2009b). Nowadays, the proportion of stroke patients who return to work ranges from 11% to 85% (Donker-Cools et al., Citation2015; Saeki & Toyonaga, Citation2010), with a mean of approximately 40% (van Velzen, van Bennekom, Edelaar, Sluiter, & Frings-Dresen, Citation2009a). This wide range is caused by different definitions of stroke and work, varying study samples, and different follow-up periods. It would be of great value to determine more precisely the proportion of stroke patients who return to work, and to know which factors might predict return to work post-stroke. This would enable better information and more targeted care to be provided, in order to improve the support for stroke patients in the process of reintegration into working life.
Although several studies have examined factors predicting return to work post-stroke, the majority have focused on stroke-related and demographic factors only, such as age, gender, functional status (e.g., Barthel Index (BI) and muscle strength), stroke characteristics (e.g., stroke type and lesion site), and level of education and work type (e.g., white and blue collar) pre-stroke (Donker-Cools et al., Citation2015; van Velzen et al., Citation2009b). However, many of these factors, especially those concerning motor functioning, are less relevant for mild stroke patients, because they more often suffer from the less visible consequences of stroke, such as mood disorders and cognitive complaints (Tellier & Rochette, Citation2009).
To our knowledge, few studies have so far examined the predictive value of personal (e.g., self-efficacy and coping style) and neuropsychological (e.g., mood and cognition) factors in relation to return to work in mild-to-moderate stroke patients. In regards to personal factors, higher self-efficacy has been mentioned as a common factor indicating positive outcomes in terms of return to work across multiple health conditions (Cancelliere et al., Citation2016). Furthermore, a qualitative meta-synthesis on patients perspectives (Brannigan et al., Citation2016) and a systematic review investigating the effects of intervention strategies and skills training on returning to work suggested that coping style might be an important trainable factor to facilitate returning to work after a stroke (Donker-Cools, Daams, Wind, & Frings-Dresen, Citation2016). A recent cross-sectional study with a limited number of participants by Arwert et al. (Citation2016) found an association between a less avoidant coping style and return to work, as well as between depressive symptoms and return to work. Regarding neuropsychological factors, some studies have claimed depressive symptoms to be predictive of return to work after a stroke (Hackett, Glozier, Jan, & Lindley, Citation2012; Waje-Andreassen et al., Citation2013), though others did not find such a relationship (Bonner et al., Citation2016; Tanaka, Toyonaga, & Hashimoto, Citation2011, Citation2014). With respect to cognitive functioning, inconsistent results have been obtained; three studies have shown that cognitive ability or executive functioning are associated with return to work (Culler, Wang, Byers, & Trierweiler, Citation2011; Fride et al., Citation2015; Vestling, Tufvesson, & Iwarsson, Citation2003), and in the study by Kauranen et al. (Citation2013), the number of cognitive disorders predicted the ability or inability to return to work post-stroke. However, three other studies have examined cognitive functioning but did not find any relations with return to work (Doucet, Muller, Verdun-Esquer, Debelleix, & Brochard, Citation2012; Hackett et al., Citation2012; Van Patten, Merz, Mulhauser, & Fucetola, Citation2016).
In sum, thorough investigation of factors predicting return to work after mild-to-moderate stroke is necessary to set realistic and attainable therapeutic goals, and to anticipate the need for occupational support by either rehabilitation care services or employers. Still, research findings on the proportion of stroke patients returning to work have varied greatly, and consensus on factors predicting return to work after mild-to-moderate stroke has not yet been established. Personal and neuropsychological factors in particular have received insufficient attention in this field. Therefore, the aims of this study were (1) to quantify return to work and work satisfaction one year after mild-to-moderate stroke, and (2) to determine factors predicting return to work after mild-to-moderate stroke, focusing particularly on personal and neuropsychological factors in addition to demographic and clinical characteristics.
Methods
Design
The current study was part of the prospective longitudinal multicentre Restore4Stroke Cohort Study, which followed stroke patients for up to two years post-stroke to determine associations between quality of life and health condition factors, personal factors and environmental factors (van Mierlo et al., Citation2014). Stroke patients were recruited in six participating general hospitals in the Netherlands between March 2011 and March 2013. The medical ethics committees of all participating hospitals approved the Restore4Stroke Cohort study, and informed consent was obtained from all included patients. The present study analysed data obtained at stroke onset, two months post-stroke and one-year post-stroke in the subgroup of patients that was employed prior to the stroke.
Participants
The current study sample comprised individuals of the Restore4Stroke Cohort Study who had experienced mild-to-moderate stroke. Stroke patients were eligible for this study if they were ≥18 years old, had a clinically confirmed diagnosis of stroke (ischemic or haemorrhagic lesion), had suffered their stroke within the last seven days, and had had a paid job at the time of their stroke. Patients were excluded if they had (a) another serious health condition that could be expected to interfere with the study outcomes; (b) already been dependent pre-stroke regarding activities of daily living, as defined by a BI of <18 (Collin, Wade, Davies, & Horne, Citation1988); (c) insufficient command of the Dutch language to understand and complete questionnaires, based on clinical judgement; (d) already been experiencing cognitive decline pre-stroke, as defined by a score of ≥1 on the Heteroanamnesis List Cognition (Meijer, van Limbeek, & de Haan, Citation2006); or (e) experienced severe stroke, as defined by a National Institutes of Health Stroke Scale (NIHSS) (Brott et al., Citation1989) score of ≥16.
Procedure
The first assessment took place in the first week after stroke onset and regarded demographic and stroke-related factors. After informed consent had been given, the stroke-related factors, examined by a neurologist, were extracted from the medical charts. Information on demographic factors was obtained from the patient or family members. During the second assessment, which took place after two months, the researcher visited the patients at their place of residence. Patients were asked to complete self-report scales for coping style, personality and mood, and global cognitive screening was conducted by trained research assistants. In the third assessment, which took place after one year, current occupational status and work satisfaction were examined by means of questionnaires, which could be completed online or on paper and returned by mail.
Outcome measures
Occupational status was evaluated in the first week after stroke onset to determine the premorbid situation and one-year post-stroke, using the Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-P), a validated tool to rate objective and subjective participation in persons with physical disabilities (Post et al., Citation2012). USER-P covers three different aspects of participation: frequency, restrictions, and satisfaction. Occupational status was measured using the first question of the USER-P, which asks the respondents how many hours a week they usually spend on a paid job. There are six answering options: 0 h, 1–8 h, 9–16 h, 17–24 h, 25–35 h, and >35 h.
As a secondary outcome, work satisfaction was also assessed one-year post-stroke, using one item of the USER-P: “How satisfied are you with your current daily life regarding paid work, unpaid work or education?” This question is scored from 1 (very dissatisfied) to 5 (very satisfied).
Determinants
Demographic and stroke-related factors were collected in the first week after stroke onset. Demographic factors included age, gender, relationship status, level of education, and place of residence. Patients were considered to be in a relationship when they were having a steady relationship, living together, living apart together, or married. The level of education was defined using the Dutch Verhage classification, ranging from 1 (did not complete primary school) to 7 (university graduation) (Verhage, Citation1964). Scores of 1 to 4 on this classification were regarded as lower education, while scores 5 to 7 represented higher education. Place of residence was determined two months post-stroke, differentiating between patients living at home and patients living in a rehabilitation setting. In regards to stroke-related factors, we collected data on type of stroke, location of stroke, vascular area, severity of stroke, and independence in activities of daily living (ADL). Type of stroke, location of stroke and vascular area were extracted from the medical charts. Severity of stroke was determined with the NIHSS, ranging from 0 to 42 (Brott et al., Citation1989). Independence in ADL was assessed using the BI, which is a validated measure and commonly used for stroke patients (Collin et al., Citation1988). BI scores range from 0 to 20, and patients with a score below 18 were regarded as dependent in ADL (Quinn, Langhorne, & Stott, Citation2011).
Two months post-stroke, personal and neuropsychological factors were assessed, including passive coping, self-efficacy, depressive and anxiety symptoms, and global cognitive functioning. Passive coping strategy was measured using the passive coping subscale (seven items) of the Utrecht Coping List (UCL-P). UCL-P scores range from 7 to 28, with higher scores indicating a greater use of passive coping styles (Eriksen, Olff, & Ursin, Citation1997). Self-efficacy was measured with the General Self-Efficacy Scale (GSES) (Scholz, Doña, Sud, & Schwarzer, Citation2002). This instrument consists of 10 items scored on a 4-point scale, which results in a total score between 10 and 40, with higher scores indicating a higher level of self-efficacy (Scholz et al., Citation2002). The presence of depressive and anxiety symptoms was assessed with the Hospital Anxiety and Depression Scale (HADS) (Spinhoven et al., Citation1997; Zigmond & Snaith, Citation1983), which includes two subscales of seven questions each concerning either depression or anxiety. Both subscales lead to a total score between 0 and 21, a higher score indicating more depressive symptoms or more anxiety symptoms. A score of 9 or higher was considered to suggest depression or anxiety (Bjelland, Dahl, Haug, & Neckelmann, Citation2002). The total HADS score, ranging from 0 to 42, was also determined to give an overall indication of emotional mood. Global cognitive functioning was assessed two months post-stroke using the Montreal Cognitive Assessment (MoCA), which is a brief and validated cognitive screening tool for use in stroke patients (Nasreddine et al., Citation2005). The MoCA ranges from 0 to 30, and patients scoring below 26 were considered cognitively impaired (Nasreddine et al., Citation2005).
Statistical analysis
Descriptive statistics were used to describe the stroke population and their work situation. To maintain adequate size of subgroups in the description of return to work and work satisfaction, the scores obtained by USER-P on occupational status were partially merged from six answering options to four subgroups based on the number of hours a week spent on paid work: 0 h, 1–16 h, 17–35 h, and >35 h. Chi-squared and Mann-Whitney-U tests were used to compare the participants who did (partially) and did not return to work within one-year post-stroke. For this comparative analysis, return to work one-year post-stroke was further dichotomised into two categories: “return to work” and “no return to work”. The former group comprised all people who spent 1 to >35 h a week on a paid job one-year post-stroke according to the USER-P.
The course of returning to work throughout the first-year post-stroke was evaluated by determining the frequencies of the four different subgroups (0 h, 1–16 h, 17–35 h, and >35 h) of return to work, at stroke onset and one-year post-stroke. Satisfaction with work one-year post-stroke was then assessed in relation to return to work. The 5-item work satisfaction scale was dichotomised by merging scores 1 (very dissatisfied) to 3 (neutral), and merging scores 4 (satisfied) and 5 (very satisfied). The former group was considered dissatisfied, the latter satisfied. The percentage of patients who were satisfied with their work was determined for all four subgroups of return to work.
Spearman’s correlation was computed to investigate correlations between return to work one-year post-stroke and demographic, stroke-related, personal, and neuropsychological factors. To maintain statistical power, 8 determinants were incorporated in this analysis (based on an event-variable ratio of 10:1). For this purpose, determinants were selected based on literature and on the gap of knowledge in personal and neuropsychological factors in relation to return to work. The following variables were included: age, level of education, independence in ADL, passive coping, self-efficacy, depressive and anxiety symptoms, and global cognitive functioning (all continuous scores). A correlation was considered weak at less than .3, moderate between .3 and .5, and strong at greater than .5 (Cohen, Citation1988).
Variables that were significantly associated with return to work one-year post-stroke, using an alpha level of .10, were entered as independent variables in the logistic regression analysis. This liberal significance level increased the power for the selection of true predictors. The candidate determinants were tested for multicollinearity (correlation coefficient, >.7), which did not reveal any problems. For the purpose of determining independent predictors of return to work, the critical value of alpha was set at .05.
All statistics were performed with the SPSS statistical software package (version 22 and 23).
Results
Study sample
The Restore4stroke cohort consisted of 395 patients of whom 121 patients had a paid job prior to their stroke and had a mild-to-moderate stroke according to NIHSS (Mean age, 56.3; Female, 27.3%; low mean NIHSS (2.3); NIHSS < 6, 86.8%; high mean BI (18.2); and high mean MoCA (25.3)). All descriptive characteristics of the study sample are presented in . It shows that global cognitive functioning at two months post-stroke was the only significantly different characteristic between the groups who had (n = 87) and had not (n = 34) returned to work within one year after their stroke: participants who had not returned to work within one-year post-stroke presented with more cognitive impairment than those who had returned to work (Z = −2.0; p = .048).
Table 1. Descriptive characteristics of participants (n = 121)€.
Return to work and work satisfaction
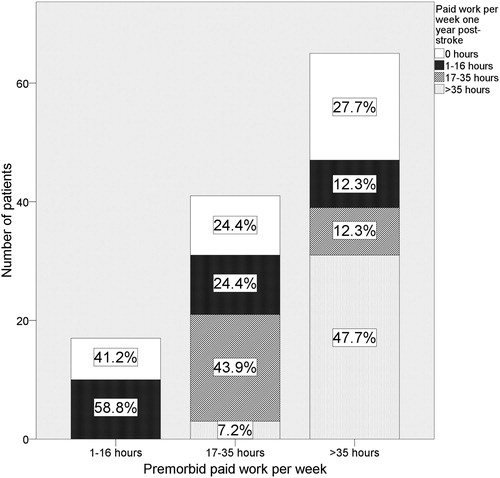
The findings regarding return to work one-year post-stroke are presented in and . One-year post-stroke, 28.1% had not returned to work, while 71.9% of all participants had returned to work. Almost 30% of whom had returned to work were working fewer hours a week than pre-stroke. As illustrated in , of the group who had worked between 1 and 16 h a week in the premorbid situation, 41.2% were not working at all one-year post-stroke. The other 58.8% were still working between 1 and 16 h a week. In the 17–35 h group, 24.4% were not in work one-year post-stroke, while 24.4% worked less, 43.9% were still working between 17 and 35 h, and 7.3% were working fulltime post-stroke. Of all participants who had worked fulltime pre-stroke, 27.0% were no longer in work one year later, while 24.4% were working fewer hours a week, and 47.6% were still working fulltime one year after their stroke.
Table 2. Work situation and work satisfaction (n = 121).
As presented in , work satisfaction increased with the number of hours a week spent on a paid job. More than a third (36.4%) of all participants who were not in paid occupation one year post-stroke, including those in unpaid jobs and education, were satisfied with their work situation. Ninety percent of the patients who spent more than 35 h a week on a job were satisfied. Of the people who were working between 1 and 16 h and between 17 and 35 h a week, 67.9% and 76.0%, respectively, were satisfied with their occupational situation.
Factors predicting return to work
shows bivariate relationships between eight variables (age, level of education, independence in ADL, passive coping, self-efficacy, depressive and anxiety symptoms, and global cognitive functioning) and return to work. Depressive symptoms (r = −.16) and global cognitive functioning (r = .19) were significantly associated with return to work one-year post-stroke.
Table 3. Bivariate correlation with return to work one-year post-stroke.
Logistic regression was used to assess the predictive value of these two independent variables (depressive symptoms and global cognitive functioning) for return to work one-year post-stroke. The full model containing all predictors was statistically significant, χ2, (2, n = 110) = 8.737, p = .013, indicating that it was able to distinguish between respondents who did and did not return to work. The model as a whole explained 11.3% (Nagelkerke R square) of the variance in return to work, and correctly classified 75.5% of cases. As shown in , only global cognitive functioning at two months made a unique statistically significant contribution to the model.
Table 4. Logistic regression model predicting return to work one-year post-stroke.
presents global cognitive functioning in relation to return to work and place of residence. As shown there, a quarter (25.2%) of all patients who were discharged home (90.4%) had not returned to work in the first-year post-stroke (average score on the MoCA of 23.8 [SD = 3.9] two months post-stroke). Patients who were discharged directly to their own home and had returned to work (67.5%) had an average MoCA score of 25.7 (2.7). Of all patients who were referred to a rehabilitation centre (9.6%), about 50% had returned to work (MoCA score of 24.3 [6.0]) while 50% had not (MoCA 27.0 [2.3]).
Table 5. Global cognitive functioning, place of residence, and return to work (n = 114)a.
Discussion
The aims of the current study were (1) to quantify return to work and work satisfaction one year after mild-to-moderate stroke, and (2) to determine factors predicting return to work post-stroke in a population with mild-to-moderate stroke. We found that only about half of the stroke patients were working the same number of hours a week one-year post-stroke as they had done pre-stroke, while the other half were working less or not at all. We also found that work satisfaction increased with the number of hours a week spent in a paid job, ranging from 36.4% of those who had not returned to work to 90.0% of those who were working fulltime. In regards to the factors predicting return to work, global cognitive functioning and depressive symptoms were significantly associated with return to work one-year post-stroke, but only impaired global cognitive functioning appeared to be a statistically significant independent predictor of return to work.
With respect to the study sample, which comprised only mild and moderate stroke patients, 86.8% could be discharged directly to their own homes (see ), which is more than described in other stroke studies (50% to 70%, irrespective of stroke severity) (Somerford, Lee, & Yau, Citation2004; Tuppin, Samson, Fagot-Campagna, & Woimant, Citation2016; van Mierlo et al., Citation2016). In addition, compared to other cohorts of stroke patients, a high percentage of our study sample had suffered an ischemic stroke (92.6%), compared to 75% of the total stroke population in the Netherlands (van Mierlo et al., Citation2016). This high proportion may be due to the fact that haemorrhagic strokes are generally more severe (Andersen, Olsen, Dehlendorff, & Kammersgaard, Citation2009), which could have led to exclusion because of high NIHSS scores (≥16), hospitalisation in academic centres (while we included patients in general hospitals), greater difficulty in understanding the instructions for the study, or not being able to give informed consent within the first week after stroke-onset.
Looking only at returning to work, and not at the number of working hours, the findings show that 71.9% of our subjects had returned to work one year after their mild-to-moderate strokes. This is in accordance with, and even at the higher end of, the wide range reported in the literature (11%–85%) (Donker-Cools et al., Citation2015; Saeki & Toyonaga, Citation2010). Two recent studies reported figures of 39% (Arwert et al., Citation2016) and 59% (Van Patten et al., Citation2016), both also concerning hospital cohorts. Among patients with mild stroke, the average percentage returning to work is just over 50% (Arwert et al., Citation2016; van Velzen et al., Citation2009a).
However, a large proportion of such patients return to work to a very limited degree (O’Brien & Wolf, Citation2010; van Velzen et al., Citation2009a), even though they are considered to be the group with the best chances of good outcome in rehabilitation. A similar phenomenon can be seen in our study sample, where only about half of our mild-to-moderate stroke patients worked the same number of hours as they did pre-stroke. This is alarming for two reasons. First, our study population comprised only mild and moderate stroke patients (mean NIHSS, 2.3; mean BI, 18.2; mean MoCA, 25.3); 86.8% of the participants had an NIHSS score of < 6 and are thus considered mild stroke patients (Edwards, Hahn, Baum, & Dromerick, Citation2006). These mild stroke patients are hardly provided with medical follow-up, and are presumed to continue with life, including their professional life, as it was pre-stroke (Boosman, Visser-meily, & Post, Citation2013; Edwards et al., Citation2006; Fride et al., Citation2015). Our study shows that this is not always the case. Secondly, it is generally assumed that a plateau phase in recovery is reached approximately six months post-stroke, including body functions and activities (Langhorne, Bernhardt, & Kwakkel, Citation2011) as well as quality of life (van Mierlo et al., Citation2016). Hence, the percentage of our study sample returning to work will probably not increase much during the subsequent years, unless external factors, such as adaptation of tasks, stability and structure of the work environment, and professional support, can be modified in such a way as to realise reintegration into an adequately adapted work place (Frostad Liaset & Lorås, Citation2016).
Nonetheless, fulltime employment turned out to generate high work satisfaction in the current study. An impressive 90.0% of the participants who were working fulltime one-year post-stroke were satisfied with their work situation. By contrast, only a third of unemployed participants, and two thirds of those who were working between 1 and 16 h a week were satisfied with their work situation. In the Netherlands, almost 80% of the healthy Dutch working population have been estimated to be satisfied with their work situation, and approximately 60% of the population were satisfied with the number of hours of work a week (Hupkens, Citation2012). The percentages in the current study were quite similar to this, but we also found that fulltime employment seems to be an important factor in work satisfaction. Hence, stroke survivors should be given the best possible support in the process of reintegration into working life.
In our population with mild-to-moderate stroke patients, global cognitive functioning at two months appeared to be the only factor predicting return to work one-year post-stroke. Though, the correlation coefficient was rather low (r = .19) and global cognitive functioning accounted for a small percentage of the variance of return to work (11.3%). Random variation in the study sample, differences in educational level, and external factors might also play a role in these results. Besides, the MoCA is a gross cognitive screening tool to measure cognitive impairment. However, we consider it a positive fact that even a gross measure of global cognitive functioning can demonstrate a difference between the two groups. Still, the difference of MoCA scores between the two groups was rather small (25.6 and 24.3) and would perhaps not be interpreted differently clinically. In two other studies an increase of ≥2 points at the MoCA has been used to indicate cognitive improvement, but no explanation for this cut-off has been given in these studies (Nijsse et al., Citation2017; Sivakumar et al., Citation2014). To our knowledge, no study has investigated the clinically relevant difference of the MoCA so far, but it would be useful for the future.
Nevertheless, the finding of cognition as a possible predicting factor of return to work after mild-to-moderate stroke confirms the idea that mild-to-moderate stroke patients with good functional outcomes can still be cognitively impaired, even though they are often discharged directly home from hospital (Boosman et al., Citation2013; van Mierlo et al., Citation2016). Our study showed that as much as a quarter of the participants who were discharged directly home had not returned to work in the first-year post-stroke. Importantly, this group showed global cognitive impairments at two months, with a lower score on the MoCA compared to those who had returned to work (see ). This demonstrates the importance of cognitive functioning for returning to work after mild stroke.
Our finding of global cognitive functioning as a predictor of return to work post-stroke is in line with other studies, which showed that cognitive ability (Culler et al., Citation2011; Vestling et al., Citation2003), executive function (Fride et al., Citation2015) and the number of cognitive disorders (Kauranen et al., Citation2013) are predictors of return to work post-stroke. However, three other studies assessed cognition without finding any associations between cognitive functioning and return to work (Doucet et al., Citation2012; Hackett et al., Citation2012; Van Patten et al., Citation2016). Their findings might be explained by the methods they used for cognitive assessment, as their data were extracted either from the medical charts (Doucet et al., Citation2012; Van Patten et al., Citation2016), or assessed by telephone (Hackett et al., Citation2012). In any case, it is plausible that impaired cognitive functioning, even with minor problems, is a predictor of return to work. Work place and work environment have changed dramatically over the last decades (e.g., in the intensive use of digital devices, globalisation, changes to worktime scheduling), which might have resulted in increased work pressure (Sparks, Faragher, & Cooper, Citation2001). Workplace intervention, including workability assessment and workplace visits, has been reported to facilitate return to work (Ntsiea, Van Aswegen, Lord, & Olorunju, Citation2015). Furthermore, some studies have investigated cognitive functioning in relation to occupational results, and show that executive functioning and social cognition difficulties following acquired brain injury have been linked to negative occupational outcomes, that is the perceptions and appraisal of colleagues (Yeates et al., Citation2016), and that a positive relationship exists between cognitive functioning and task performance (Corgnet, Hernán Gonzalez, & Mateo, Citation2015).
Last, it is remarkable that independence in activities of daily living as measured with the BI did not predict return to work in our study sample. Several other studies have found that BI, mRS, or FIM scores predict return to work post-stroke (Donker-Cools et al., Citation2015; van Velzen et al., Citation2009b). Perhaps the overall independence score of our study sample was too high because we selected patients with mild-to-moderate stroke. As a result, ceiling effects may have minimised the contrast between the participants who had returned and had not returned to work. More generally, with the decrease of mortality post-stroke and the incline of the proportion of people with milder strokes (Wolf, Barbee, & White, Citation2011), measures such as BI, mRS, or FIM are perhaps not sensitive enough to capture the more subtle impairment that a milder stroke survivor population experiences. Furthermore, we had expected personal factors to predict return to work based on literature (Arwert et al., Citation2016; Brannigan et al., Citation2016; Cancelliere et al., Citation2016; Donker-Cools et al., Citation2016). However, our study did not confirm this.
Limitations
Although this was a large-scale prospective study on return to work by patients with mild-to-moderate stroke, some limitations should be mentioned. First, the data on return to work did not cover the nature of the employment or the exact number of working hours; we only measured the number of hours a week spent in a paid job in categories, as reported by the patients. As a result, return to work could not be interpreted in the light of any possible changes in the difficulty of the occupational tasks or exact changes in working hours. Second, work type has been reported to be a possible predictor of return to work post-stroke (van Velzen et al., Citation2009b), and would have been an interesting variable to investigate. Also, adaptation of the work environment, flexibility in working hours, and professional support might be of influence to return to work (Donker-Cools et al., Citation2016; Frostad Liaset & Lorås, Citation2016; Ntsiea et al., Citation2015), and would also have been an interesting variable to investigate. As mentioned before, we used a gross cognitive screening tool to assess global cognitive functioning, which does not distinguish any subtasks of cognition. For clinical purposes, more comprehensive assessment of various cognitive tasks in returning to work would have given more insight into the exact impairments stroke patients experience in returning to work and the need for intervention. Furthermore, although our study sample consisted of a rather large group of working stroke patients, it may still have been too small for thorough analysis. The group that had not returned to work comprised only 34 patients, which was too small for subgroup analyses.
Clinical implications and directions for further research
Employment is one of the most important factors determining life satisfaction and quality of life (Passier et al., Citation2011; van Velzen et al., Citation2009b; Vestling et al., Citation2003). Hence, stroke patients should be given the best possible support in the process of reintegration into working life. In our study sample, which comprised mild-to-moderate stroke patients with good functional outcomes, global cognitive functioning at two months predicted return to work in the first-year post-stroke. We therefore suggest that all stroke patients of working age should be offered a cognitive screening, or a more comprehensive neuropsychological assessment to gain more insight into cognitive strengths and weaknesses, and if applicable should start cognitive rehabilitation. As the MoCA explained just 11% of the variance, external factors probably play a pivotal role in returning to work as well and should be taken into account during rehabilitation. To date, severe stroke patients, who are discharged to rehabilitation centres, have received more attention and support in the process of returning to work than patients discharged home. Patients with mild-to-moderate stroke, however, require attention and support as well. A rehabilitation team should provide these mild stroke patients with appropriate guidance in returning to work, including an explanation of the less visible consequences of stroke, to both the patients themselves and the company doctor, workplace management, and colleagues (Donker-Cools et al., Citation2016; Frostad Liaset & Lorås, Citation2016). Whether cognitive rehabilitation actually results in improved rates of return to work post-stroke should be investigated in future studies.
Conclusion
In this predictive cohort study regarding return to work post-stroke, approximately 50% of patients with mild-to-moderate stroke who had been employed pre-stroke had returned to the same number of working hours a week one year post-stroke. The other half were working less or not at all. As employment is of eminent importance for quality of life, life satisfaction, and work satisfaction, stroke patients should be offered the best possible support to reintegrate into working life. Global cognitive functioning was the only variable predicting return to work in this study. Hence, stroke patients with minor symptoms who have problems returning to work might benefit from cognitive screening and cognitive rehabilitation. Furthermore, cognitive screening of patients with mild-to-moderate stroke should receive more attention, so that patients with mild cognitive impairment can be better supported in returning to work from a very early period on, e.g., by learning compensational strategies. Whether cognitive rehabilitation actually results in higher rates of return to work post-stroke remains to be investigated further.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Tanja C. W. Nijboer http://orcid.org/0000-0001-6683-0267
Additional information
Funding
References
- Andersen, K. K., Olsen, T. S., Dehlendorff, C., & Kammersgaard, L. P. (2009). Hemorrhagic and ischemic strokes compared: Stroke severity, mortality, and risk factors. Stroke, 40(6), 2068–2072. doi:10.1161/STROKEAHA.108.540112
- Arwert, H., Schults, M., Meesters, J., Wolterbeek, R., Boiten, J., & Vliet Vlieland, T. (2016). Return to work 2–5 years after stroke: A cross sectional study in a hospital-based population. Journal of Occupational Rehabilitation. doi:10.1007/s10926-016-9651-4
- Bjelland, I., Dahl, A. A., Haug, T. T., & Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale. Journal of Psychosomatic Research, 52(2), 69–77. doi:10.1016/S0022-3999(01)00296-3
- Bonner, B., Pillai, R., Sarma, P. S., Lipska, K. J., Pandian, J., & Sylaja, P. N. (2016). Factors predictive of return to work after stroke in patients with mild−moderate disability in India. European Journal of Neurology, 23(3), 548–553. doi:10.1111/ene.12887
- Boosman, H., Visser-meily, J. M. A., & Post, M. W. M. (2013). Validity of the barrow neurological institute (BNI) screen for higher cerebral functions in stroke patients with good functional outcome. The Clinical Neuropsychologist, 27(4), 667–680. doi:10.1080/13854046.2013.777787
- Brannigan, C., Galvin, R., Walsh, M. E., Loughnane, C., Morrissey, E.-J., Macey, C., … Horgan, N. F. (2016). Barriers and facilitators associated with return to work after stroke: A qualitative meta-synthesis. Disability and Rehabilitation, 8288, 1–12. doi:10.3109/09638288.2016.1141242
- Brott, T., Adams, H. P., Olinger, C. P., Marler, J. R., Barsan, W. G., Biller, J., … Hertzberg, V. (1989). Measurements of acute cerebral infarction: A clinical examination scale. Stroke, 20(7), 864–870. doi:10.1161/01.STR.20.7.864
- Cancelliere, C., Donovan, J., Stochkendahl, M. J., Biscardi, M., Ammendolia, C., Myburgh, C., & Cassidy, J. D. (2016). Factors affecting return to work after injury or illness: Best evidence synthesis of systematic reviews. Chiropractic & Manual Therapies, 24(1), 32. doi:10.1186/s12998-016-0113-z
- Cohen, J. (1988). Statistical power analysis for the behavioural sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates.
- Collin, C., Wade, D. T., Davies, S., & Horne, V. (1988). The barthel ADL index: A reliability study. International Disability Studies, 10(2), 61–63. doi:10.3109/09638288809164103
- Corgnet, B., Hernán Gonzalez, R., & Mateo, R. (2015). Cognitive reflection and the diligent worker: An experimental study of millennials. PloS One, 10(11), e0141243. doi:10.1371/journal.pone.0141243
- Culler, K. H., Wang, Y.-C., Byers, K., & Trierweiler, R. (2011). Barriers and facilitators of return to work for individuals with strokes: Perspectives of the stroke survivor, vocational specialist, and employer. Topics in Stroke Rehabilitation, 18(4), 325–340. doi:10.1310/tsr1804-325
- Donker-Cools, B. H. P. M., Daams, J. G., Wind, H., & Frings-Dresen, M. H. W. (2016). Effective return-to-work interventions after acquired brain injury: A systematic review. Brain Injury, 30(2), 113–131. doi:10.3109/02699052.2015.1090014
- Donker-Cools, B. H. P. M., Wind, H., & Frings-Dresen, M. H. W. (2015). Prognostic factors of return to work after traumatic or non-traumatic acquired brain injury. Disability and Rehabilitation, 38(8), 733–741. doi:10.3109/09638288.2015.1061608
- Doucet, T., Muller, F., Verdun-Esquer, C., Debelleix, X., & Brochard, P. (2012). Returning to work after a stroke: A retrospective study at the physical and rehabilitation medicine center “La tour de gassies”. Annals of Physical and Rehabilitation Medicine, 55(2), 112–127. doi:10.1016/j.rehab.2012.01.007
- Edwards, D. F., Hahn, M., Baum, C., & Dromerick, A. W. (2006). The impact of mild stroke on meaningful activity and life satisfaction. Journal of Stroke and Cerebrovascular Diseases, 15(4), 151–157. doi:10.1016/j.jstrokecerebrovasdis.2006.04.001
- Eriksen, H. R., Olff, M., & Ursin, H. (1997). The CODE: A revised battery for coping and defense and its relations to subjective health. Scandinavian Journal of Psychology, 38(3), 175–182. doi:10.1111/1467-9450.00025
- Fride, Y., Adamit, T., Maeir, A., Ben Assayag, E., Bornstein, N. M., Korczyn, A. D., & Katz, N. (2015). What are the correlates of cognition and participation to return to work after first ever mild stroke? Topics in Stroke Rehabilitation, 22(5), 317–325. doi:10.1179/1074935714Z.0000000013
- Frostad Liaset, I., & Lorås, H. (2016). Perceived factors in return to work after acquired brain injury: A qualitative meta-synthesis. Scandinavian Journal of Occupational Therapy, 8128, 1–12. doi:10.3109/11038128.2016.1152294
- Hackett, M. L., Glozier, N., Jan, S., & Lindley, R. (2012). Returning to paid employment after stroke: The psychosocial outcomes in stroke (POISE) cohort study. PloS One, 7(7), e41795. doi:10.1371/journal.pone.0041795
- Hupkens, C. (2012). Meeste werknemers tevreden met aantal werkuren: Sociaaleconomische trends, 1e kwartaal 2012.
- Kauranen, T., Turunen, K., Laari, S., Mustanoja, S., Baumann, P., & Poutiainen, E. (2013). The severity of cognitive deficits predicts return to work after a first-ever ischaemic stroke. Journal of Neurology, Neurosurgery & Psychiatry, 84(3), 316–321. doi:10.1136/jnnp-2012-302629
- Langhorne, P., Bernhardt, J., & Kwakkel, G. (2011). Stroke rehabilitation. The Lancet, 377(9778), 1693–1702. doi:10.1016/S0140-6736(11)60325-5
- Meijer, R., van Limbeek, J., & de Haan, R. (2006). Development of the stroke-unit discharge guideline: Choice of assessment instruments for prediction in the subacute phase post-stroke. International Journal of Rehabilitation Research, 29(1), 1–8. doi:10.1097/01.mrr.0000175269.59788.41
- Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., … Chertkow, H. (2005). The Montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699. doi:10.1111/j.1532-5415.2005.53221.x
- Nijsse, B., Visser-Meily, J. M. A., van Mierlo, M. L., Post, M. W. M., de Kort, P. L. M., & van Heugten, C. M. (2017). Temporal evolution of poststroke cognitive impairment using the Montreal cognitive assessment. Stroke, 48, 98–104. doi:10.1161/STROKEAHA.116.014168
- Ntsiea, M. V., Van Aswegen, H., Lord, S., & Olorunju, S. S. (2015). The effect of a workplace intervention programme on return to work after stroke: A randomised controlled trial. Clinical Rehabilitation, 29(7), 663–673. doi:10.1177/0269215514554241
- O’Brien, A. N., & Wolf, T. J. (2010). Determining work outcomes in mild to moderate stroke survivors. Work, 36(4), 441–447. doi:10.3233/WOR-2010-1047
- Passier, P. E. C. A., Visser-Meily, J. M. A., Rinkel, G. J. E., Lindeman, E., & Post, M. W. M. (2011). Life satisfaction and return to work after aneurysmal subarachnoid hemorrhage. Journal of Stroke and Cerebrovascular Diseases, 20(4), 324–329. doi:10.1016/j.jstrokecerebrovasdis.2010.02.001
- Post, M. W. M., van der Zee, C. H., Hennink, J., Schafrat, C. G., Visser-Meily, J. M. A., & van Berlekom, S. B. (2012). Validity of the Utrecht scale for evaluation of rehabilitation-participation. Disability and Rehabilitation, 34(6), 478–485. doi:10.3109/09638288.2011.608148
- Quinn, T. J., Langhorne, P., & Stott, D. J. (2011). Barthel index for stroke trials: Development, properties, and application. Stroke, 42(4), 1146–1151. doi:10.1161/STROKEAHA.110.598540
- Saeki, S., & Toyonaga, T. (2010). Determinants of early return to work after first stroke in Japan. Journal of Rehabilitation Medicine, 42(3), 254–258. doi:10.2340/16501977-0503
- Scholz, U., Doña, B., Sud, S., & Schwarzer, R. (2002). Is general self-efficacy a universal construct? Psychometric findings from 25 countries. European Journal of Psychological Assessment, 18, 242–251. doi:10.1027//1015-5759.18.3.242
- Sivakumar, L., Mahesh, K., Jeerakathil, T., Camicioli, R., Buck, B., & Butcher, K. (2014). Serial Montreal cognitive assessments demonstrate reversible cognitive impairment in patients with acute transient ischemic attack and minor stroke. Stroke, 45, 1709–1715. doi:10.1161/STROKEAHA.114.004726
- Somerford, P., Lee, A., & Yau, K. (2004). Ischemic stroke hospital stay and discharge destination. Annals of Epidemiology, 14(10), 773–777. doi:10.1016/j.annepidem.2004.02.003
- Sparks, K., Faragher, B., & Cooper, C. L. (2001). Well-being and occupational health in the 21st century workplace. Journal of Occupational and Organizational Psychology, 74(4), 489–509. doi:10.1348/096317901167497
- Spinhoven, P., Ormel, J., Sloekers, P. P. A., Kempen, G. I. J. M., Speckens, A. E. M., & Hemert, A. M. VAN. (1997). A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch subjects. Psychological Medicine, 27(2), 363–370. doi:10.1017/S0033291796004382
- Tanaka, H., Toyonaga, T., & Hashimoto, H. (2011). Functional and occupational characteristics associated with very early return to work after stroke in Japan. Archives of Physical Medicine and Rehabilitation, 92(5), 743–748. doi:10.1016/j.apmr.2010.12.009
- Tanaka, H., Toyonaga, T., & Hashimoto, H. (2014). Functional and occupational characteristics predictive of a return to work within 18 months after stroke in Japan: Implications for rehabilitation. International Archives of Occupational and Environmental Health, 87(4), 445–453. doi:10.1007/s00420-013-0883-8
- Tellier, M., & Rochette, A. (2009). Falling through the cracks: A literature review to understand the reality of mild stroke survivors. Topics in Stroke Rehabilitation, 16(6), 454–462. doi:10.1310/tsr1606-454
- Tuppin, P., Samson, S., Fagot-Campagna, A., & Woimant, F. (2016). Care pathways and healthcare use of stroke survivors six months after admission to an acute-care hospital in France in 2012. Revue Neurologique, 172(4–5), 295–306. doi:10.1016/j.neurol.2016.01.398
- van Mierlo, M. L., van Heugten, C. M., Post, M. W. M., Hajos, T. R., Kappelle, L. J., & Visser-Meily, J. M. A. (2016). Quality of life during the first two years post stroke: The Restore4Stroke cohort study. Cerebrovascular Diseases, 41(1–2), 19–26. doi:10.1159/000441197
- van Mierlo, M. L., van Heugten, C. M., Post, M. W. M., Lindeman, E., de Kort, P. L. M., & Visser-Meily, J. M. A. (2014). A longitudinal cohort study on quality of life in stroke patients and their partners: Restore4Stroke cohort. International Journal of Stroke. doi:10.1111/j.1747-4949.2012.00882.x
- Van Patten, R., Merz, Z. C., Mulhauser, K., & Fucetola, R. (2016). Multivariable prediction of return to work at Six-month follow-up in mild to moderate acute stroke patients. Archives of Physical Medicine and Rehabilitation. doi:10.1016/j.apmr/2016.06.006
- van Velzen, J. M., van Bennekom, C. A. M., Edelaar, M. J. A., Sluiter, J. K., & Frings-Dresen, M. H. W. (2009a). How many people return to work after acquired brain injury?: A systematic review. Brain Injury, 23(6), 473–488. doi:10.1080/02699050902970737
- van Velzen, J. M., van Bennekom, C. A. M., Edelaar, M. J. A., Sluiter, J. K., & Frings-Dresen, M. H. W. (2009b). Prognostic factors of return to work after acquired brain injury: A systematic review. Brain Injury, 23(5), 385–395. doi:10.1080/02699050902838165
- Verhage, F. (1964). Intelligence and age: Study among Dutch people from age 12 to 77 [Dutch]. Assen: Van Gorcum.
- Vestling, M., Tufvesson, B., & Iwarsson, S. (2003). Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. Journal of Rehabilitation Medicine, 35(3), 127–131. doi:10.1080/16501970310010475
- Waje-Andreassen, U., Thomassen, L., Jusufovic, M., Power, K. N., Eide, G. E., Vedeler, C. A., & Naess, H. (2013). Ischaemic stroke at a young age is a serious event - final results of a population-based long-term follow-up in western norway. European Journal of Neurology, 20(5), 818–823. doi:10.1111/ene.12073
- Wolf, T. J., Barbee, A. R., & White, D. (2011). Executive dysfunction immediately after mild stroke. OTJR: Occupation, Participation and Health, 31(1), S23–S29. doi:10.3928/15394492-20101108-05
- Yeates, G., Rowberry, M., Dunne, S., Goshawk, M., Mahadevan, M., Tyerman, R., … Tyerman, A. (2016). Social cognition and executive functioning predictors of supervisors’ appraisal of interpersonal behaviour in the workplace following acquired brain injury. NeuroRehabilitation, 38(3), 299–310. doi:10.3233/NRE-161321
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. doi:10.1111/j.1600-0447.1983.tb09716.x