ABSTRACT
Relationships make important contributions to wellbeing and maintenance of self-worth. For those who sustain traumatic brain injury (TBI), life is frequently characterized by declining interpersonal relationships. The aim of this study was to understand the post-injury experience of friendship from the perspective of adults with severe TBI. Participants were 23 adults who had sustained severe TBI on average 10 years earlier; the majority was between 25 and 45 years old. The experience of friendship was explored using a convergent mixed methods design (quantitative self-report measures and in-depth interviews). Qualitative analysis of interview transcripts employed open and focussed coding to reveal themes and categories. Participants nominated on average 3.35 (SD 2.19) friends. When paid carers and family members were excluded, the mean dropped to 1.52 (SD 1.38). Exploratory correlations between number of friends and quality of life, depression and strong-tie support revealed significant associations of moderate to large effects. The post-injury experience of friendship was broadly conceptualized as “going downhill” with four overlapping phases: losing contact, being misunderstood, wanting to share and hanging on. Participants’ stories illustrated how rehabilitation can focus on friendship by supporting established relationships and facilitating access to activities that afford interpersonal encounters and opportunities to share experiences.
Introduction
Close relationships make an important contribution to wellbeing and the maintenance of a positive sense of self-worth. In fact, relationships with others are the most frequently reported source of life meaning across the lifespan (Delle Fave, Brdar, Wissing, & & Vella-Brodrick, Citation2013; O’Connor & Chamberlain, Citation2000). Further, relationships have long been acknowledged to be powerful moderators of stress and wellbeing (Cohen & Wills, Citation1985; Douglas, Citation2013; Jetten, Haslam, Haslam, & A, Citation2012), and evidence linking social relationships to both psychological and physical health is as strong as evidence linking smoking, obesity, blood pressure and physical activity to health (House, Landis, & Umberson, Citation1988; Umberson & Montez, Citation2010; Umberson, Williams, Powers, Liu, & Needham, Citation2006).
Lack of social relationships and challenges within existing relationships are common and enduring experiences for many people who acquire neurological disorders during adulthood. Social relational outcomes have been explored for survivors of stroke (Northcott & Hilari, Citation2011; Northcott, Marshall, & Hilari, Citation2016; Northcott, Moss, Harrison, & Hilari, Citation2016; Pound, Gompertz, & Ebrahim, Citation1998; Sarre et al., Citation2014), including those with aphasia (Barry & Douglas, Citation2000; Brown, Davidson, Worrall, & Howe, Citation2013; Davidson, Howe, Worrall, Hickson, & Togher, Citation2008; Ford, Douglas, & O’Halloran, Citation2018; Fotiadou, Northcott, Chatzidaki, & Hilari, Citation2014), people diagnosed with dementia (Clare et al., Citation2012; Pozzebon, Douglas, & Ames, Citation2016; Citation2018) and survivors of traumatic brain injury (TBI) (Dikman, Machamer, Powell, & Temkin, Citation2003; Douglas & Spellacy, Citation2000; Douglas, Drummond, Knox, & Mealings, Citation2015; Draper, Ponsford, & Schönberger, Citation2007; Jourdan et al., Citation2016; Lefebvre, Cloutier, & Levert, Citation2008; Tate, Broe, Cameron, Hodgkinson, & Soo, Citation2005; Tate, Lulham, Broe, Strettles, & Pfaff, Citation1989). This body of research provides both quantitative and qualitative evidence of the negative impact that these acquired neurological disorders can have within the domain of relationships, including friendships and intimate partnerships.
While social relationship challenges may characterize outcome for many people with acquired neurological disability, the epidemiological and neuropathological features of the disorder type can shape the context within which and how these challenges play out. Consider the influence of the age-related peak incidence of a disorder and when in the life course a disorder is likely to arise. For example, dementia is by definition a degenerative disorder with declining and varying profiles dependent on the disease (e.g., Alzheimer’s Disease vs. Frontotemporal Dementia vs. variant forms of Primary Progressive Aphasia). Typically the dementia-related disease process becomes apparent with aging and later in life when existing relational connections (family and friends) are well established and may be more likely to withstand the changes wrought by the disease as it progresses. Indeed, the very presence of established family and friend support networks has been reported by spouses as being crucial in maintaining their sense of connectedness towards their partners, as well as keeping these couples socially engaged (Pozzebon, Douglas, & Ames, Citation2018).
In the case of stroke, incidence increases with age as evidenced by recent figures published by Public Health England (PHE). These figures (2007–2016) show that 38% of the total estimated incidence of stroke in England occurred in people aged 40–69 and 59% in people over 70 (PHE, Citation2018). Thus, most stroke survivors are in the mid to later stages of life with established intimate partnerships, family relationships and friendships that are frequently described by participants in qualitative studies as providing vital support through the adjustment process (Brown et al., Citation2013; Cruice, Worrall, & Hickson, Citation2006; Ford et al., Citation2018; Fotiadou et al., Citation2014). Further, based on the results of their systematic review of quantitative studies, Northcott, Moss, et al. (Citation2016) reported that on average people with stroke perceived themselves to be well-supported following their stroke and over time. Contact with immediate family and close attachment figures remained stable, but number of friends, contact with friends and network size was seen to reduce in comparison with controls, as did involvement in social activities. Depression was consistently associated with poor social support and reduced social network (Northcott, Marshall, et al., Citation2016).
In contrast to dementia and stroke, TBI typically affects young people (mostly men) aged 18–35 years (Australian Institute of Health and Welfare [AIHW], Citation2007). Many of these young people are at a point in their lives where they are transitioning (from secondary to higher level education, from education to work, from family home to self-supported living environments). They are becoming part of new social networks, maintaining some old friendships while developing new ones including intimate partnerships and beginning their own families. It is a time of flux and a time when friends are particularly important. During late adolescence, friends are crucial to support our developing identity. As we move into adulthood (20–30), we need to build a diverse group of friends supporting our social and professional lives and helping us make sense of the adult we are becoming (Degges-White & Van Tieghem, Citation2015). Thus, the peak incidence of TBI occurs during a life period characterized by change, when friendships are more likely to be vulnerable and less stable and when individuals are actively finding a way into their adult identity. In this context, it is unsurprising that outcome studies show that adults who sustain TBI can continue to experience restricted relationships over many years (Dikman et al., Citation2003; Draper et al., Citation2007; Jourdan et al., Citation2016; Lefebvre et al., Citation2008; Tate et al., Citation1989; Tate et al., Citation2005). Given differences in the epidemiology and neuropathology across acquired neurological disorders, exploration of social outcome to inform the development of rehabilitation strategies is best conducted within a specific disorder population (e.g., TBI) rather than across populations in a general category of disorders (e.g., acquired neurological disorders). Comparison of data measuring constructs of interest (e.g., number of friends) with data from the healthy population can be informative. Where possible, a matched control data set is clearly preferred. However, without matched control data, general population survey data can provide some useful comparative information.
Social relationships can be indexed by several variables including the size of social networks, the social support perceived and received, the quality and quantity of friendships and feelings of loneliness. Results of large population surveys generally indicate that the majority of the population is satisfied with the number of personal friends they have and the quality of these relationships. In 2004, Carroll reported the results of a Gallup survey based on telephone interviews with a randomly selected national USA sample of 1,011 adults, aged 18 and older. Respondents reported having a mean of 8.6 close friends (median 5), not including their relatives. Nearly half (45%) said they had six or more close friends, 39% reported between three and five close friends and 14% reported one or two close friends. Only 2% said they had no close friends. No statistically significant differences were evident between men and women but those aged 65 and older reported significantly more close friends with an average of 13, compared with 9 friends for those aged 18–29 and 50–64 and 7 friends for 30–49-year-olds. Overall, most respondents were satisfied with their number of friends (73%) and the closeness of their relationships with friends (82%).
These various indices of social connection have all drawn research attention in the context of acquired neurological disorders generally and TBI specifically where loss of friendship, social isolation and loneliness have emerged as consistent findings (Douglas & Spellacy, Citation2000; Eames, Cotterill, Kneale, Storrar, & Yeomans, Citation1996; Hoofien, Gilboa, Vakil, & Donovick, Citation2001; Lefebvre et al., Citation2008; Salas, Casassus, Rowlands, Pimm, & Flanagan, Citation2018; Shorland & Douglas, Citation2010). Both loss and lack of friendship are particularly prominent themes in qualitative studies exploring the lived experience of people with TBI (Douglas, Citation2015; Paterson & Stewart, Citation2002; Salas et al., Citation2018; Shorland & Douglas, Citation2010) and participants have frequently provided moving descriptions of their problems with friendship and their desire to make new friends, for example:
I’m a loner; friends who were there at the time have just gone. I’m still at home; … . (I want) to be accepted by other people, to have friends. I go out by myself on Saturdays just to tell people at work I’ve been out. (Douglas & Spellacy, Citation2000, p. 82)
In this context of frequent interpersonal problems and restricted relationships for adults with severe TBI, the aim of this study was to understand the post-injury experience of friendship from the perspective of those who had been living with the consequences of severe TBI over several years. There are a number of reasons why the experience of friendship for people with severe TBI in the longer term requires specific research attention. First, long-term outcome for this group is less likely to be positive (Draper et al., Citation2007; Ponsford, Draper, & Schönberger, Citation2008; Tate et al., Citation2005), particularly with respect to participation in employment (Cattelani, Tanzi, Lombardi, & Mazzucchi, Citation2002; Kreutzer et al., Citation2003) and education (Mealings, Douglas, & Olver, Citation2012; Willmott, Ponsford, Downing, & Carty, Citation2014). Community engagement and social integration are also more likely to be limited for these individuals in comparison with those with less severe injuries (Draper et al., Citation2007; Ponsford et al., Citation2008; Tate et al., Citation2005). In addition, the stories of those who have faced the challenges of maintaining and developing friendships for several years after severe TBI provide a critical perspective through which to characterize a process, build theory and inform rehabilitation efforts to address complex problems like this one. Indeed, a thorough understanding of the lived experience is considered by many to be essential in the development and evaluation of interventions (Campbell et al., Citation2000; Craig et al., Citation2008). With increased understanding of the insider’s perspective, it was hoped that concepts and insights would emerge that could inform the development of rehabilitation practices to facilitate maintenance and development of friendships and improve social connection for adults who have sustained severe TBI.
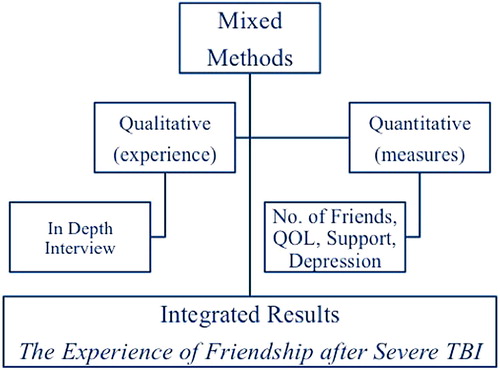
A convergent mixed method research (MMR) design (Creswell, Citation2015; Creswell, Klassen, Plano Clark, & Smith, Citation2011; Tashakkori, Citation2009; Tashakkori & Teddlie, Citation2010) employing elements of qualitative and quantitative paradigms was selected to meet the aim of the study: to understand the post-injury experience of friendship from the perspective of adults with severe TBI. The aim was conceptualized as being informed by participants’ reflective stories of their friendship experiences since injury and the magnitude and frequency of constructs measured by their responses on assessments capturing the number of friends they considered themselves to have, frequency of social support problems, their mood and quality of life at the time they participated in the study. The overall study with both the qualitative and quantitative components reflected a constructivist philosophical stance.
Given the intent of the qualitative arm of the study was to develop understanding grounded in the experiences of adults living with the consequences of severe TBI, friendship was explored within a constructivist Grounded Theory framework (Charmaz, Citation2006, Citation2009). Grounded Theory is well suited to social inquiry when there is a relative lack of established information about the phenomenon of interest and researchers believe they can learn from participants how to better understand that phenomenon (Bluff, Citation2005; Browne, Citation2004). Grounded Theory enables the research process to move from data to theory in contrast to the typical positivist process of testing a pre-existing theory (Browne, Citation2004).
A quantitative approach was used to index companionship through self-nomination of the number of friends in each individual’s life and to explore the strength of association between companionship (perceived number of friends) and three constructs that have typically signalled poor outcome in people with acquired neurological disorders and especially those with severe TBI: lack of perceived strong tie (social) support, poor quality of life and low mood/frequent symptoms of depression. The quantitative correlational analyses were not included to test apriori hypotheses but rather to examine the magnitude of the association between these constructs in order to appreciate the role that quantity of nominated friends plays in shaping these life parameters as perceived by this group of adults living in the community several years after sustaining severe TBI.
As recommended for MMR (Creswell, Citation2015; Creswell et al., Citation2011; Tashakkori & Teddlie, Citation2010), the study components were designed and implemented to address related aspects of the same broad question requiring real-life contextual understanding with the intention of integrating the results emerging from both approaches (see ). In this case, the constructivist grounded theory component of the study focused on understanding phenomena associated with friendship after injury and over time as revealed in participants’ reflections on their post-injury experiences. The quantitative component complemented exploration of the same aim, to gain an understanding of phenomena associated with friendship after injury, by using self-report measures to gain insight into associations between number of friends and aspects of social and emotional function known to be vulnerable following severe TBI.
Method
Participants
Purposive sampling was used to recruit 23 adults (20 men and 3 women) who had sustained severe TBI. Metropolitan community allied health practitioners and disability agencies known to provide services to people with TBI were provided with written information to pass on to potential participants. If an individual was willing to volunteer and meet the researcher, the potential participant’s contact details were passed to the researcher and the researcher’s contact details to the potential participant. All those who volunteered were able to provide informed consent and no individual had a guardian or administrator appointed to make decisions on their behalf. All were born in Australia and living in metropolitan cities or regional towns in the state of Victoria. Using the Australian Standard Classification of Cultural and Ethnic Groups (Australian Bureau of Statistics, Citation2011) participants’ backgrounds reflected the following groups: British (56%), Southern European (22%), Eastern European (13%), and Arab (9%).
Participants were required to have sustained severe TBI as indexed by either a Glasgow Coma Scale (GCS) score ≤ 8 (Jennett & Teasdale, Citation1981) or duration of post-traumatic amnesia (PTA) ≥ 14 days using the Westmead PTA Scale (Marosszeky, Ryan, Shores, Batchelor, & Marosszeky, Citation1997). GCS scores were available for 14 participants and ranged from 3 to 5. Length of PTA for the remaining 9 participants ranged from 28 days to greater than 4 months. All participants had sustained TBI as a result of motor vehicle-related trauma (8 drivers, 7 passengers, 2 cyclists, 6 pedestrians). People with a documented preinjury history of neurological or psychiatric disability or being currently treated for psychotic disorder were not eligible to participate in the study. As interview was a substantial component of the data collection procedure, participants were required to use speech or a speech-generating device (SGD) as their primary mode of communication. This selection criterion did not result in any exclusions and no participant was using an SGD.
Descriptive statistics for age and time post-injury (TPI) at the time of participation in the study are shown in . On average 10 years had elapsed since the injury and the majority of participants were between 25 and 45 years old. They all lived in the community with family or paid support and were receiving lifetime support through a no-fault, state government funded, 3rd party insurance scheme. Four were employed on a part-time basis, 3 were actively involved in volunteer work and the remaining 16 participants were not currently engaged in work activities.
Table 1. Descriptive statistics for demographic variables, quality of life social support and mood measures.
Methods of data generation
In-depth interviews, field notes, a personal demographic questionnaire, client files and three self-report rating scales were the sources of data used in this study. Textual data generated from interviews and field notes were analysed qualitatively and statistical analyses were applied to the quantitative data (see data analysis section). Information from the personal demographic questionnaire and clinical files was used for descriptive purposes.
In-depth interview
Conducting qualitative research interviews with people with severe TBI can be challenging due to the impact of memory deficits, impaired conversational and narrative discourse, and fatigue (Carlsson, Paterson, Scott-Findlay, Ehnfors, & Ehrenberg, Citation2007; Douglas, Citation2013). Despite these challenges, the in-depth interview was chosen as the primary method of qualitative data collection because it aligned with the aim of the qualitative arm of the study and because the author, a speech pathologist and clinical neuropsychologist, has considerable experience conducting in-depth interviews with people with TBI clinically and in research. The interview began with a broad open invitation to share information about life in general: Tell me how things have been going for you in the last while. You know, what you’ve been doing, who you’ve been seeing, what’s good, not so good. Follow-up probes were also identified to guide the conversation and to create links between each interview. Probes focused on exploring and understanding the participant’s experience of friendship and everyday companionship (e.g., ..and friends, how about friends, people you like to spend time with, go out with, people you trust, and talk to about stuff that’s important to you?). Probes were also used to cue recall of further information about a particular event (e.g., You were talking about name … , can you tell me more? what you were doing? how you felt?).
To minimize the impact that cognitive-communicative impairment associated with severe TBI has on conversational and narrative discourse (Coelho, Youse, & Le, Citation2002; Douglas, Citation2010; Snow, Douglas, & Ponsford, Citation1998; Citation1999), strategies and scaffolding procedures previously detailed by Douglas (Citation2013) were used to facilitate the interview process. All the interviews were conducted by the author and each of the participants engaged well in the interview process. While several participants presented with cognitive-communicative problems, no participant had primary language impairment (aphasia). Responses tended towards short sentences, expressing a series of information units not always clearly connected. Intelligibility was sometimes impaired due to dysarthria, but in most cases requests for clarification or more information successfully resolved intended meaning and facilitated transcription. Towards the end of the interview, participants were asked to nominate the people in their lives who they would consider friends; people they felt close to, trusted and could talk to about the good and not so good things that were happening in their lives. Most of the time they naturally indicated the person’s relationship to them (e.g., family member, friend from rehabilitation or work, paid carer/support worker); if the person’s relationship to the participant was not specified, clarification was sought.
Quantitative measures
Each of the three quantitative measures had acceptable reliability (content and test-retest indices ≥ .7), demonstrated construct validity, had been used previously to measure outcome following TBI, was easy to complete and could be administered in 15 minutes or less.
Quality of life. Self-rated “goodness” or “quality” of life was measured using the scale developed by Hadorn, Sorenson, and Holte (Citation1995). Participants are shown an 11-point scale with a sad face above 0 representing the worst possible QOL, progressing to the happiest face above 10, representing the best possible QOL. They are then asked to use the scale to indicate overall how they rate the quality of their life or how good they consider their life to be. Construct validity has been supported by significant correlations (ranging from .66 to .71) with the Quality of Life Health Questionnaire (Hadorn et al., Citation1995). The scale has also been used effectively with adults with severe TBI (Douglas, Dyson, & Foreman, Citation2006; Steadman-Pare, Colantonio, Ratcliff, Chase, & Vernich, Citation2001).
Depression was measured using the depression subscale of the Neurobehavioural Functioning Inventory (NFI-D; Kreutzer, Seel, & Marwitz, Citation1999), developed specifically for use with the TBI population. The subscale score range is 13–65 with scores increasing as a function of increasing frequency of symptoms. Cronbach’s alpha analysis revealed acceptably high internal reliability for all the NFI scales ranging from .86 to .95 (Kreutzer, Marwitz, Seel, & Serio, Citation1996).
Strong-tie social support. The Strong-tie support subscale (STS) of the Instrumental-Expressive Social Support-Scale (IESSS; Ensel & Woelfel, Citation1986) was used to measure perceived frequency of problems with companionship (e.g., not having a close companion; not having enough close friends). The items in the IESSS were constructed to allow for a description of types of support that were not strictly a function of socio-demographic differences (e.g., employment, marital status, and family situation). The STS subscale score ranges from 3 to 15 with higher scores being consistent with more frequent problems and has demonstrated adequate internal consistency as indicated by a Cronbach’s alpha of 0.7 (Ensel & Woelfel, Citation1986). The scale has been used previously to measure social support functions with adults with severe TBI (Douglas et al., Citation2006; Douglas & Spellacy, Citation2000).
Procedure
After a potential participant indicated willingness to be contacted, the researcher phoned the person to give further information and confirm the individual’s interest. If the potential participant expressed willingness to participate, a visit was arranged at a mutually suitable time and location. In all cases, the participants chose to be seen in their homes. The visit commenced with reconfirming the individual’s understanding of the project and completing the formal informed consent process. The audio-taped, interview was then completed, followed by administration of the three quantitative measures. The visit concluded with a brief discussion of how the participant felt and setting up a time for the researcher to phone the person in the next few days to check if there was anything they would like to clarify or discuss further. This follow-up phone call also served the function of evaluating whether the person was at all distressed by participating in the study. All participants indicated they appreciated the opportunity to talk about their experiences. Duration of the visit ranged from 1–3 hours. Field notes pertaining to the visit were completed by the researcher via audio-recording immediately after the interview. The purpose of the field notes was to record observations made by the researcher during the interview. Audio-taped interviews and field notes were transcribed verbatim as soon as possible and no more than 10 days after the visit. QSR NVivo (version11; QSR International Pty Ltd) software was used to assist data management. Institutional approval to conduct the study was granted by the University Human Research Ethics Committee prior to its commencement.
Data analysis
Qualitative
Grounded theory focuses on extracting meanings that people give to actions and events. It involves development of an integrated understanding of human behaviour grounded in the processes revealed in people’s experience. The theoretical perspective behind this inquiry was symbolic interactionism which views human behaviour as emergent and continually constructed through the process of interaction between people (Blumer, Citation1969). Data collection and analysis occurred simultaneously over a period of 18 months. Analysis moved through a process of data-driven open and focussed coding, identification of emergent friendship-related categories and exploration of relations between these categories using the method of constant comparison. Initially, verbatim transcripts were examined and textual excerpts were coded to reflect the meaning of the words recorded. As the data from each successive interview were compared and contrasted in an iterative process, codes became increasingly focused until clear categories and core concepts emerged. Categories were reviewed against the original transcripts to ensure they maintained the voice of the participants and were anchored in their life experience. This process of analysis led to a preliminary grounded theory of the experience of friendship after severe TBI.
Questions regarding credibility, originality, resonance and usefulness were applied to interpretations of the data throughout the analysis process (Charmaz, Citation2006). Memo writing was used to provide an audit trail from data collection to model building. In addition throughout the project, first the codes and then later the categories that resulted from data analysis were reviewed independently and discussed in detail with another experienced qualitative researcher who did not have clinical or research experience in the field of neurological rehabilitation. Where differences occurred, original interview transcripts, fieldnotes and coding memos were reviewed and the code, category or concept under consideration was discussed and revised until consensus about meaning was reached. Memos were used to ensure that data analysis decisions were documented. Further, the resonance and the usefulness of the findings were verified through presentation and discussion of interpretations in local, national and international professional forums during and at the conclusion of the research process. Finally, to show the reader that the analysis is fully grounded in the participants’ accounts of themselves, illustrative quotes from the interviews are presented throughout the text. In order to protect the identity of participants, the names used following each quote are pseudonyms.
Quantitative
Descriptive statistics were calculated for scores on the QOL, depression and strong-tie support (STS) scales. Following examination of scatterplots to evaluate linearity and homoscedasticity, exploratory correlational analyses (Pearson’s r) were conducted to ascertain the strength of relation between total number of nominated friends, both including and excluding family and paid carers, and QOL, depression (NFI-D) and STS. The coefficient of determination was also calculated to estimate how much variance each pair of variables shared. An alpha level of .05 was used to determine statistical significance, no adjustments were made for multiple comparisons due to the exploratory nature of the analyses and Cohen’s (Citation1988) guidelines for interpreting the strength of association were applied (small: .10 to .29; moderate: .30 to .49; large: .50 to 1.0).
Results
Number and source of friends after injury
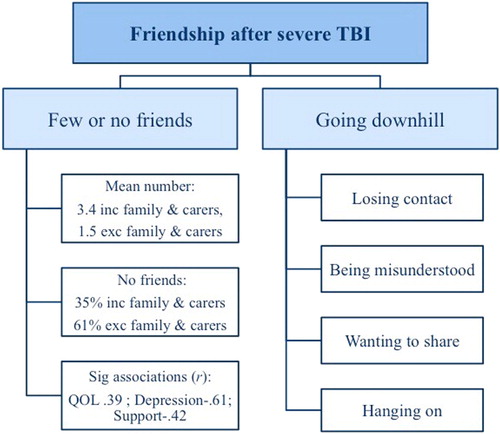
Descriptive statistics for number of friends nominated by participants and scores on the quantitative measures (QOL, NFI-D and STS) are shown in . When nominated friends included family and paid carers/support workers, 8 participants (35%) reported having no friends. With the exclusion of family and paid carers as friends, the number of participants reporting no friends increased to 14 (61%). Only 3 participants (13%) had maintained a friendship that was active before their injury.
Exploratory correlations between total number of friends including family and paid carers revealed significant associations of moderate to large effects across QOL, depression and strong-tie support (see ). The largest effect (r = −.61; 37.2% shared variance) was evident as a negative association between number of friends and frequency of depressive symptoms. The associations between number of friends and QOL and number of friends and strong-tie support were moderate in magnitude (.39 and −.42 respectively) with between 15 and 20% shared variance. Correlations between these three variables and number of friends excluding family and paid carers/support workers were less strong with only the relationship between depression and number of friends reaching statistical significance and showing moderate strength (−.45; 20.25% shared variance).
Table 2. Pearson correlation coefficients and shared variance between number of friends, quality of life (QOL), depression and strong-tie support.
The sources of relationship/friendship varied across participants. Family (parents, siblings and partners) including extended family or family friends (sister’s husband, cousins and old friend of the family, siblings’ friends) was the most frequently nominated source of friendship identified by 15 participants followed by paid carers or support workers identified by 9 participants. Eight participants identified people known through activities in the community as friends; activities included attending the local pub and community sporting clubs, art and music groups, gym, nightclub, disability groups and church groups. Three participants identified housemates as friends, two identified health professionals, one identified people met during rehabilitation and one identified people at work.
The experience of friendship after injury
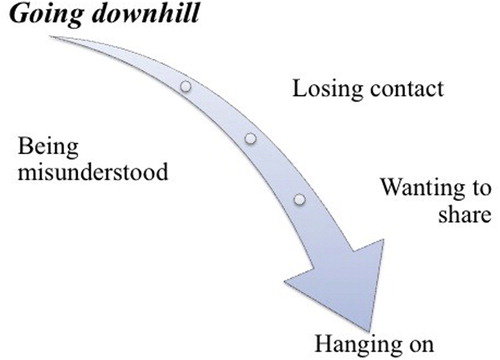
Analysis of the interview transcripts revealed that the post-injury experience of friendship was broadly characterized as “going downhill.” This downward trajectory accompanied by a sense of being rejected was captured by Ryan: “After head injury you know everything just changes and your whole, your whole like social life goes downhill you know, ‘cause nobody wants to know you.’” Four major categories emerged within this overall concept of going downhill: losing contact, being misunderstood, wanting to share and hanging on. While these categories overlapped and coexisted with each other, a temporal sense of the process of going downhill beginning with losing contact with friends and moving to a point of hanging on was also conveyed across participants’ construction of the experience. The overall process is illustrated in .
Losing contact reflected a consistent recognition that loss was associated with friends and friendship since the injury. This sense of loss was evident in similar comments made frequently across participants: “most friends dropped off after the accident” (Henry); “ … . (I‘ve) been a bit of a loner since the accident” (Mia); “No not many friends around since the accident” (George); “I don’t have many friends, well I don’t have any actually.” (Carl). As described by Bernard, losing contact was coupled with feeling bad and lonely “Bad and lonely at home just me without family, without friends.” and for Joseph it brought the experience of diminishing hope “Hope can only go on for so long and then it fades.”
Being misunderstood traversed much of the participants’ discourse throughout the interviews and quotes within this category were frequently delivered with a vocal tone that communicated both frustration and anger. Ryan was angry because “Other people think they’re kings and I’m not – I’ve had an accident and people don’t understand me.” Similarly, Bernard directed the following comment to people he encountered in the community: “They treat me like an idiot … really hate the way people treat me. People act like they’re going to catch something off me.” Greg pointed out that behaviour from others towards him came from a lack of understanding brain injury and in turn this lack of understanding prevented him from feeling a sense of belonging: “ … .the way other people treat me – they don’t understand ABI behaviour … it’s like I really don’t belong anywhere.” Jake brought up the notion that lack of understanding meant that negative assumptions about brain injury and its consequences were being made by people around him: “People assume that because you’ve had a head injury, you don’t know what they’re talking about” and Barry extended this to people not wanting to relate to him: “Most people can’t understand me – they won’t associate with me.” Mia pulled her experiences together by describing the attitude of people as being dismissive and therefore reflecting a lack of willingness to get to know her: “Many of the people I meet are dismissive because I’m a bit different. They’re just not willing to listen to me or get to know me.”
Wanting to share but not finding it easy to do so was a common experience for participants. Reduced or lack of opportunity to share emerged within the participants’ stories as a consequence of losing contact with friends, being misunderstood by people generally and being alone. This process was tough and left participants with the dilemma of wanting to socially participate but being isolated from others, as captured by Carl’s comment: “I don’t mind being alone, but I would like someone to share things with. I would do more things now because … I’m not doing anything now. I don’t have anything.” When only family members covered friendship functions, participants talked about how this restricted their ability to share thoughts, feelings and problems. Alistair noted: “there’s only certain things I’d discuss with family” and Greg likened his life to being like an old person with no mates to share times with: “Sometimes I become like a granddad … . no one to have fun with.” Lucas brought together a common experiential thread of missing social sharing and being known to others: “I miss being popular and having people know who I am.”
Hanging on brought to the fore the actions these participants employed to “hang in there” (Greg), “keep going” (Olga) and “make it through another year” (Mia). In many ways, this category encapsulated advice grounded in the participants’ personal experiences of friendship following TBI. Carl advocated looking for ways to be useful: “It’s good to feel useful,” Wayne previously “a workaholic” pointed out how now: “I appreciate the simplicity of life” and similarly for Steve his fundamental attitude of simple survival was crucial to hanging on, “every day is a good day if I’m breathing.” Olga reflected on the protective function of interaction stating how important it was to “always talk because if not you think too much and that’s not good and you never know who will become a friend.” Greg had moved on to taking some direct action and “learning how to be a friend” by attending a friendship skills group for people with brain injury and being ready to “ … .put myself out to please other people.”
Maintaining or developing activities was seen as a useful way of hanging on socially. Jake highlighted how pursuit of a long-held interest could bring chances of group participation: “I like music group … always loved playing instruments.” Bernard also stayed involved through group activity organized by the local disability support service: “There’s a group on a Thursday night where we have dinner, hang out and sometimes do things like go out and play pool” and Jim enjoyed working on his fitness level in a group rather than individual environment: “Got to get fit and I do it with a group. We have a great time.” Indeed Jim identified the link between group activities and friendship opportunity when he said: “I like activities because you meet friends.”
Integrating quantitative and qualitative results
Taken together the results of this mixed methods study reflect a current picture of few and for the majority no friends outside of family members in the lives of these individuals. Further, QOL, depression and support measures varied significantly and substantially as a function of number of friends nominated by participants. In the context of this diminished picture of friendship painted by current quantitative measures, these participants provided rich background and a temporal perspective to their lived experience of friendship following severe TBI through sharing their stories. Qualitative analysis revealed an overarching concept reflecting a process of going downhill characterized by four categories from underlying themes revealed within the interview data. presents an integrated formulation of the results from both arms of the study.
Discussion
Poor social integration including few and compromised friendships following TBI are findings previously reported in studies investigating short, medium and long-term outcomes in this population (Dikman et al., Citation2003; Draper et al., Citation2007; Hoofien et al., Citation2001; Tate et al., Citation1989; Tate, Kennedy, et al., Citation2014). This convergent mixed methods study set out to explore the post-injury experience of friendship from the perspective of adults who had been living with the consequences of severe TBI over several years. The majority of participants were between 25 and 45 years of age and most (20/23) were men. Participants talked in-depth about their experiences and completed self-report measures to evaluate the strength of associations between the number of friends they nominated and measures of depression, social support and quality of life. Through this exploration, it was hoped that crucial insights into processes active within the domain of friendship after injury would become apparent and ultimately inform the development of rehabilitation practices to maintain and foster friendships in the lives of people with severe TBI. The results paint a challenging picture. Even with our knowledge of poor social outcome following severe TBI, it is daunting to consider that nearly two in three of these participants (61%) had no friends outside family and paid carers and one in three (35%) had no friends even when family and paid carers were considered. For this group, the average number of 1.5 close friends excluding family fell well below that of 8.6 friends reported by the general population (Carroll, Citation2004). Similarly, the contrast between the 2% proportion of adults in the general population who report having no friends (Carroll, Citation2004) and the 61% proportion of participants in this study also emphasizes the severity of the problem.
Lack of friends has been shown to have considerable repercussions with respect to health generally and particularly emotional wellbeing (House et al., Citation1988; Umberson & Montez, Citation2010). A recent systematic review (Northcott, Moss, et al., Citation2016) of the impact of stroke on social support and social networks has revealed similar findings as has a prospective longitudinal observational study (Northcott, Moss, et al., Citation2016) investigating predictors of social networks following stroke. The average age of this group was 70 years and 45.1% lived alone or in institutional care. In terms of social network scores in the prospective study, only one subdomain that of friends significantly declined over the 6-month period following stroke. At 6 months, 1 in 5 (20%) participants reported having no close friends compared to 1 in 10 (10%) at baseline. While this figure is concerning, it also serves to emphasize the magnitude of the problem for the adults with TBI in this study, 61% of whom reported having no close friends.
In the current study, the relation between number of friends and emotional wellbeing was evident through a large and significant association between number of friends and depression indicating that number of friends helps to explain 37% of the variance in participants’ scores on the NFI depression subscale. Similarly, significant medium strength associations were evident between number of friends and STS and QOL, with number of friends helping to explain 18% of the variance in STS and 15% of the variance in QOL. These results add to previous evidence demonstrating that social connection and its component constructs are significant and reliable indicators of psychological functioning (Douglas & Spellacy, Citation2000; Ouellet, Morin, & Lavoie, Citation2009), community integration (McColl et al., Citation1998), family functioning (Douglas & Spellacy, Citation1996), life satisfaction (Pierce & Hanks, Citation2006), and QOL (Steadman-Pare et al., Citation2001) following TBI. Clearly, the need to address a lack of social connection for those with severe TBI is well justified.
This study has not only revealed the small number of friends and demonstrated the impact of diminished social connection on wellbeing, but it has also provided insight into the process underpinning the experience of friendship for adults living with the consequences of severe TBI. Experience reflected a post-injury downhill or deteriorating process that incorporated early loss of friends and social connections, ongoing lack of understanding with reduced opportunities to share and just hanging on to a place in society. The experience of loss and social disconnection has been reported by participants with TBI in a number of studies (Jumisko, Lexell, & Soderberg, Citation2005; Levack, Kayes, & Fadyl, Citation2010; Mealings, Douglas, & Olver, Citation2017; Muenchberger, Kendall, & Neal, Citation2008; Salas et al., Citation2018; Shorland & Douglas, Citation2010), as has more frequent contact with family when compared to little or no contact with friends (Douglas & Spellacy, Citation2000; Kinsella, Ford, & Moran, Citation1989; Kozloff, Citation1987). Feeling misunderstood or stigmatized is also consistent with the results of previous work (Knox, Douglas, & Bigby, Citation2017; Levack et al., Citation2010; Mealings et al., Citation2017; Nochi, Citation1998; Salas et al., Citation2018). The downhill process stretched over many years with some moderating factors but little or no resolution to the problem of loneliness in the lives of these participants. While knowledge of outcome captures the magnitude of the problem, knowledge of process within experience has important implications for rehabilitation and the design of interventions. Process moves the outcome lens from a static to a dynamic focus and enables identification of phases and interpersonal functions within friendship that are potentially amenable to both prevention and treatment strategies.
Rehabilitation implications and recommendations for future research
The process grounded in these participants’ lived experience points to the need for early efforts during rehabilitation to prevent losing contact with valued friends. As suggested by Palmer and Herbert (Citation2016), inpatient rehabilitation can distance a person from their preinjury social context and connections. Indeed the demands of rehabilitation activities have been noted by participants with TBI to impact negatively on the frequency of contact with friends and in turn reduce the sense of closeness within friendships (Mealings & Douglas, Citation2010; Nichols & Kosciulek, Citation2014). The rehabilitation environment is also foreign to most and can be readily perceived by friends as unwelcoming. Thus, early attention to supporting friendships is warranted and demands systematic consideration from the perspective of proactive and ongoing intervention. Palmer and Herbert’s (Citation2016) framework based on clinical cases is one example of work in this direction. Further, a number of authors have pointed to the importance of including friends in rehabilitation across the continuum from acute hospital to community settings and have identified specific clinical strategies to use (Callaway, Sloan, & Winkler, Citation2005; Mealings et al., Citation2017; Shorland & Douglas, Citation2010; Tate, Wakim, & Genders, Citation2014; Togher et al., Citation2014). Others have considered and/or trialed the benefits of peer mentoring (Hanks, Rapport, Wertheimer, & Koviak, Citation2012; Struchen et al., Citation2011), support group participation (Salas et al., Citation2018) and volunteer partnering (Johnson & Davis, Citation1998) as approaches to facilitate friendships with generally variable results. Such programmes require further development and rigorous evaluation to identify essential elements that deliver enduring positive change. Given the individualized and multifactorial nature of social connection, employment of single case experimental design (SCED) may be a particularly effective means of systematically developing an evidence base for treatment (Perdices & Tate, Citation2009).
Social networks have multiple sources, a number of which are evident in the results of this study. They comprise immediate family, extended family and family associates, old (preinjury) friends from school/college/university, work, sporting and leisure activities and shared living arrangements, new (post-injury) friends from rehabilitation, new pursuits and return to old pursuits (school/college/university, work, sporting and leisure activities), and casual acquaintances. Social network contacts can be initiated and maintained in several ways including in person and face-to-face, via text and email and through multiple social media environments. These sources and avenues for interaction provide useful contexts within which to place support and intervention strategies to maintain relationships with old friends and initiate friendships with new contacts.
The participants’ shared experience of being misunderstood reinforces the importance of education about TBI generally to the public and specifically tailored to the social network configuration of each individual. Personal stories available through the internet on Youtube and in the traditional media (newspapers, radio, television), through podcasts and incorporation of people with brain injury as authentic characters in film and stage productions have increased in recent times providing productive avenues to improving public understanding of the personal impact of brain injury and potentially reducing stigmatization. Generation and sharing of the self-narrative has also been shown to have the added advantage of building a strengths-based identity for individuals with TBI (D’Cruz, Douglas, & Serry, Citationin press). Internet support platforms as exemplified by the Genyus Network, an interactive trauma support platform, also provide opportunities for survivors of brain injury to share their stories, thoughts, feelings and problems and to support others with similar experiences.
Finally, the category of hanging on revealed that the opportunity to engage in activities, particularly interactive activities, is essential to maintaining a place in society across the post-injury trajectory. This finding adds further to a developing evidence base across a range of studies (Blake & Batson, Citation2009; Douglas et al., Citation2006; Mitchell, Veitch, & Passey, Citation2014; Powell, Rich, & Wise, Citation2016; Tate, Wakim, et al., Citation2014; Thomas, Citation2004). In turn, then, rehabilitation efforts need to continue to facilitate an individual’s participation in valued activities, skills and confidence in approaching new activity situations, re-approaching old pursuits and knowledge about and connection with community mechanisms and services that support activity participation for the general population and for those with disability. It is critical to view such efforts as ongoing with capacity to be more or less available as time and circumstances dictate.
Limitations
This study was limited by the nature of the group or more specifically two injury-related factors, severity and time post-injury. Participants had all sustained severe TBI and thus their experience cannot be generalized to those with mild to moderate injuries. In addition, on average 10 years with a range of 2–20 years had elapsed since injury and so the findings present the reflective views of people who have lived through years of experience after injury. Further, the participants had received and continued to receive support for rehabilitation through a state-funded compensation scheme. Thus, the experiences may be specific to TBI survivors who have ongoing state/insurance funded rehabilitation and support services available to them. Finally, while the sample size of 23 participants generated saturation of findings across the data, the findings are particular to the group and reflect its characteristics.
Recommendations for future research
The experiences of the participants in this research not only point to areas in which to develop interventions but also bring to awareness areas requiring further research. First, a number of injury and individual factors are just as likely to shape outcome in this domain as in others. Severity and chronicity of injury, and the associated neurobehavioural profile of the individual are likely to make important contributions to the experience of post-injury friendship. From an individual’s perspective age, sex, culture, living environment, family functioning and education as well as preinjury personal characteristics are also likely to play a role. Second, friends themselves and the nature of the connection will also contribute to differences in outcome and understanding these associations will help tailor interventions based on dyadic and group factors. Third, friendship development and maintenance are frequently underpinned by shared activity and experience and reinforced by concrete reminders of these times (i.e., social snacks, Douglas, Citation2013). Thus, research into the short and longer term outcomes of friendships built within shared activities is also warranted. Finally, working with people who have positive friendship outcomes to collaboratively explore the processes and strategies that have shaped these outcomes will undoubtedly be a fruitful endeavour.
Conclusion
This mixed methods project was undertaken to explore the post-injury experience of friendship from the perspective of those who had been living with the consequences of severe TBI over several years. Together the quantitative and qualitative findings reinforce the fragile nature of friendship and the adverse experiences associated with friendship after injury. The findings highlight the need for early and ongoing rehabilitation efforts to focus on friendship by supporting established relationships and facilitating access to activities that afford interpersonal encounters and opportunities to share experiences and develop new relationships.
Acknowledgements
Many thanks are extended to the participants who made the research possible by generously sharing their stories and time with the researcher.
Disclosure statement
No potential conflict of interest was reported by the author.
Additional information
Funding
References
- AIHW. (2007). Disability prevalence and trends. Disability series, AIHW Bulletin 55, Dec. Canberra, AIHW.
- Australian Bureau of Statistics (ABS). (2011). Australian Standard Classification of Cultural and Ethnic groups (2nd ed.). Canberra: Author.
- Barry, S., & Douglas, J. (2000). The social integration of individuals with aphasia. Advances in Speech Language Pathology, 2, 77–91.
- Blake, H., & Batson, M. (2009). Exercise intervention in brain injury: A pilot randomized study of Tai Chi Qigong. Clinical Rehabilitation, 23, 589–598.
- Bluff, R. (2005). Grounded theory: The methodology. In I. Holloway (Ed.), Qualitative research in health care (pp. 147–167). Maidenhead, Berkshire: Open University Press.
- Blumer, H. (1969). Symbolic interactionism: Perspective and method. Berkeley: University of California Press.
- Brown, K., Davidson, B., Worrall, L., & Howe, T. (2013). “Making a good time”: The role of friendship in living successfully with aphasia. International Journal of Speech-Language Pathology, 15, 165–175.
- Browne, J. (2004). Grounded theory analysis: Coming to data with questioning minds. In V. Minichiello, G. Sullivan, K. Greenwood, & R. Axford (Eds.), Research methods for nursing and health science (2nd ed., pp. 624–673). Frenchs Forest: Pearson Education Australia.
- Burleson, B., Samter, W., & Lucchetti, A. (1992). Similarity in communication values as a predictor of friendship choices: Studies of friends and best friends. Southern Communication Journal, 57, 260–276.
- Callaway, L., Sloan, S., & Winkler, D. (2005). Maintaining and developing friendships following severe traumatic brain injury: Principles of occupational therapy practice. Australian Occupational Therapy Journal, 52(3), 257–260.
- Campbell, M., Fitzpatrick, R., Haines, A., Kinmonth, A., Sandercock, P., Spiegelhalter, D., & Tyrer, P. (2000). Framework for design and evaluation of complex interventions to improve health. BMJ, 321, 694–696.
- Carlsson, E., Paterson, B., Scott-Findlay, S., Ehnfors, M., & Ehrenberg, A. (2007). Methodological issues in interviews involving people with communication impairments after acquired brain damage. Qualitative Health Research, 17, 1361–1371.
- Carroll, J. (2004). Americans satisfied with number of friends, closeness of friendships. Gallup. http://news.gallup.com/poll/10891/americans-satisfied-number-friends-closeness-friendships.aspx
- Cattelani, R., Tanzi, F., Lombardi, F., & Mazzucchi, A. (2002). Competitive re-employment after severe traumatic brain injury: Clinical, cognitive and behavioural predictive variables. Brain Injury, 16(1), 51–64.
- Channon, S., & Watts, M. (2003). Pragmatic language interpretation after closed head injury: Relationship to executive functioning. Cognitive Neuropsychiatry, 8, 243–260.
- Charmaz, K. (2006). Constructing grounded theory: A practical guide through qualitative analysis. London: Sage.
- Charmaz, K. (2009). Shifting the grounds: Constructivist grounded theory methods. In J. Morse, P. Noerager Stern, J. Corbin, B. Bowers, K. Charmaz, & A. Clarke (Eds.), Developing grounded theory: The second generation (pp. 127–193). Walnut Creek, CA: Left Coast Press.
- Clare, L., Nellis, S. M., Whitaker, C. J., Martyr, A., Markova, I. S., Roth, I., … Morris, R. G. (2012). Marital Relationship Quality in Early-Stage Dementia. Alzheimer Disease and Associated Disorders, 26, 148–158.
- Coelho, C., Youse, K., & Le, K. (2002). Conversational discourse in closed-head-injured and non-brain-injured adults. Aphasiology, 16, 659–672.
- Cohen, J. (1988). Statistical power analysis for the behavioural sciences (2nd ed.). Hillsdale, NJ: LEA.
- Cohen, S., & Wills, T. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357.
- Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth, I., & Petticrew, M. (2008). Developing and evaluating complex interventions: The new Medical research Council guidance. BMJ, 33, a1655.
- Creswell, J. (2015). Revisiting mixed methods and advancing scientific practices. In S. Hesse-Biber & R. Burke Johnson (Eds.), The Oxford handbook of multimethod and mixed methods research inquiry (pp. 39–65). Oxford: OUP.
- Creswell, J., Klassen, A., Plano Clark, V., & Smith, K. for the Office of Behavioral and Social Sciences Research. (2011). Best practices for mixed methods research in the health sciences. Washington, DC: National Institutes of Health.
- Cruice, M., Worrall, L., & Hickson, L. (2006). Quantifying aphasic people’s social lives in the context of non-aphasic peers. Aphasiology, 20, 1210–1225.
- Davidson, B., Howe, T., Worrall, L., Hickson, L., & Togher, L. (2008). Social participation for older people with aphasia: The impact of communication disability on friendships. Topics in Stroke Rehabilitation, 15, 325–340.
- D’Cruz, K., Douglas, J., & Serry, T. (in press). Personal narrative approaches in rehabilitation following traumatic brain injury: A synthesis of qualitative research. Neuropsychological Rehabilitation.
- Degges-White, S., & Van Tieghem, J. (2015). Toxic friendships. Lanham, MD: Rowman Littlefield.
- Delle Fave, A., Brdar, A., Wissing, M., & & Vella-Brodrick, D. (2013). Sources and motives for personal meaning in adulthood. The Journal of Positive Psychology, 8(6), 517–529.
- Dikman, S., Machamer, J., Powell, J., & Temkin, N. (2003). Outcome 3 to 5 years after moderate to severe traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 84, 1449–1457.
- Douglas, J. (2010). Relation of executive functioning to pragmatic outcome following severe traumatic brain injury. Journal of Speech, Language, and Hearing Research, 53, 365–382.
- Douglas, J. (2013). Conceptualizing self and maintaining social connection following severe traumatic brain injury. Brain Injury, 27(1), 60–74.
- Douglas, J. (2015). Elizabeth usher memorial lecture: Placing therapy in the context of the self and social connection. International Journal of Speech-Language Pathology, 17(3), 199–210.
- Douglas, J. (2017). “So that’s the way it is for me – always being left out.” Acquired pragmatic language impairment and social functioning following traumatic brain injury. Brain Impairment, 18, 321–331.
- Douglas, J., Drummond, M., Knox, L., & Mealings, M. (2015). Rethinking social-relational perspectives in rehabilitation: Traumatic brain injury as a case study (chapter 8). In K. McPherson, B. E. Gibson, & A. Leplege (Eds.), Rethinking rehabilitation theory (pp. 137–162). Boca Raton, FL: CRC Press.
- Douglas, J., Dyson, M., & Foreman, P. (2006). Increasing leisure activity following severe traumatic brain injury: Does it make a difference? Brain Impairment, 7, 107–118.
- Douglas, J., & Spellacy, F. (1996). Indicators of long-term family functioning following severe traumatic brain injury in adults. Brain Injury, 10, 819–840.
- Douglas, J., & Spellacy, F. J. (2000). Correlates of depression in adults with severe traumatic brain injury and their carers. Brain Injury, 14, 71–88.
- Draper, K., Ponsford, J., & Schönberger, M. (2007). Psychosocial and emotional outcomes 10 years following traumatic brain injury. Journal of Head Trauma Rehabilitation, 22(5), 278–287.
- Eames, P., Cotterill, G., Kneale, T., Storrar, A., & Yeomans, P. (1996). Outcome of intensive rehabilitation after severe brain injury: a long-term follow-up study. Brain Injury, 10, 631–650.
- Ensel, W., & Woelfel, M. (1986). Measuring the instrumental and expressive functions of social support. In N. Lin, A. Dean, & W. Ensel (Eds.), Social support, life events, and depression (pp. 129–152). Orlando, FL: Academic Press Inc.
- Ford, A., Douglas, J., & O’Halloran, R. (2018). The experience of close personal relationships from the perspective of people with aphasia: Thematic analysis of the literature. Aphasiology, 32(4), 367–393.
- Fotiadou, D., Northcott, S., Chatzidaki, A., & Hilari, K. (2014). Aphasia blog talk: How does stroke and aphasia affect a person’s social relationships? Aphasiology, 28, 1281–1300.
- Genyus Network. http://www.abc.net.au/radio/programs/sundayafternoon/caleb-rixon-stroke-survivor/8779380
- Hadorn, D., Sorenson, J., & Holte, J. (1995). Large-scale health outcomes evaluation: How should quality of life be measured? Part II – Questionnaire validation in a cohort of patients with advanced cancer Journal of Clinical Epidemiology, 48, 619–629.
- Hanks, R. A., Rapport, L. J., Wertheimer, J., & Koviak, C. (2012). Randomized controlled trial of peer mentoring for individuals with traumatic brain injury and their significant others. Archives of Physical Medicine and Rehabilitation, 93, 1297–1304.
- Hoofien, D., Gilboa, A., Vakil, E., & Donovick, P. (2001). Traumatic brain injury (TBI) 10?20 years later: A comprehensive outcome study of psychiatric symptomatology, cognitive abilities and psychosocial functioning. Brain Injury, 15, 189–209.
- House, J., Landis, K., & Umberson, D. (1988). Social relationships and health. Science, 241, 540–545.
- Jennett, B., & Teasdale, G. (1981). Management of head injuries. Contemporary neurology series. Philadelphia, PA: FA Davis Company.
- Jetten, J., Haslam, C., Haslam, S. A., & A, S. (2012). The social Cure: Identity, health & wellbeing. Hove, UK: Psychology Press.
- Johnson, K., & Davis, P. (1998). A supported relationships intervention to increase the social integration of persons with traumatic brain injuries. Behavior Modification, 22(4), 502–528.
- Jourdan, C., Bayen, E., Pradat-Diehl, P., Ghout, I., Darnoux, E., Azerad, S., … Azouvi, P. (2016). A comprehensive picture of 4-year outcome of severe brain injuries. Results from the Paris-TBI study. Annals of Physical and Rehabilitation Medicine, 59(2), 100–106.
- Jumisko, E., Lexell, J., & Soderberg, A. (2005). The meaning of living with traumatic brain injury in people with moderate or severe traumatic brain injury. Journal of Neuroscience Nursing, 37, 42–50.
- Kinsella, G., Ford, B., & Moran, C. (1989). Survival of social relationships following head injury. International Disability Studies, 11, 9–14.
- Knox, L., Douglas, J., & Bigby, C. (2017). “I’ve never been a yes person”: Decision-making participation and self-conceptualization after severe traumatic brain injury. Disability and Rehabilitation, 39(22), 2250–2260.
- Kozloff, R. (1987). Networks of social support and the outcome from severe head injury. Journal of Head Trauma Rehabilitation, 2, 14–23.
- Kreutzer, J., Marwitz, J., Seel, R., & Serio, C. (1996). Validation of a neurobehavioral functioning inventory for adults with traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 77, 116–124.
- Kreutzer, J., Marwitz, J., Walker, W., Sander, A., Sherer, M., & Bogner, J. (2003). Moderating factors in return to work and job stability after traumatic brain injury. Journal of Head Trauma Rehabilitation, 18, 128–138.
- Kreutzer, J., Seel, R., & Marwitz, J. (1999). The neurobehavioral functioning inventory. San Antonio, TX: The Psychological Corporation.
- Lefebvre, H., Cloutier, G., & Levert, J. (2008). Perspectives of survivors of traumatic brain injury and their caregivers on long-term social integration. Brain Injury, 22, 535–543.
- Levack, W., Kayes, N., & Fadyl, J. (2010). Experience of recovery and outcome following traumatic brain injury: A metasynthesis of qualitative research. Disability and Rehabilitation, 32, 986–999.
- Marosszeky, N. E. V., Ryan, L., Shores, E. A., Batchelor, J., & Marosszeky, J. E. (1997). The PTA protocol: Guidelines for using the westmead posttraumatic amnesia (PTA) scale. Sydney: Wild & Wooley.
- McColl, M., Carlson, P., Johnston, J., Minnes, P., Shue, K., & Davies, D. (1998). The definition of community integration: Perspectives of people with brain injuries. Brain Injury, 12, 15–30.
- McDonald, S. (1993). Pragmatic language skills after closed head injury: Ability to meet the informational needs of the listener. Brain and Language, 44, 28–46.
- Mealings, M., & Douglas, J. (2010). ‘School’s a big part of your life … ’: Adolescent Perspectives of Their School Participation Following Traumatic Brain Injury. Brain Impairment, 11(1), 1–16.
- Mealings, M., Douglas, J., & Olver, J. (2012). Considering the student perspective in returning to school after TBI: A literature review. Brain Injury, 26, 1165–1176.
- Mealings, M., Douglas, J., & Olver, J. (2017). Beyond academic performance: Practice implications for working with students following traumatic brain injury. International Journal of Speech-Language Pathology, 19(5), 441–453.
- Mitchell, E. J., Veitch, C., & Passey, M. (2014). Efficacy of leisure intervention groups in rehabilitation of people with an acquired brain injury. Disability and Rehabilitation, 36(17), 1474–1482.
- Muenchberger, H., Kendall, E., & Neal, R. (2008). Identity transition following traumatic brain injury: A dynamic process of contraction, expansion and tentative balance. Brain Injury, 22, 979–992.
- Nichols, J., & Kosciulek, J. (2014). Social interactions of individuals with traumatic brain injury. Journal of Rehabilitation, 80(2), 21–29.
- Nochi, M. (1998). “Loss of self” in the narratives of people with traumatic brain injuries: A qualitative analysis. Social Science and Medicine, 46, 869–878.
- Northcott, S., & Hilari, K. (2011). Why do people lose their friends after a stroke? International Journal of Language & Communication Disorders, 46, 524–534.
- Northcott, S., Marshall, J., & Hilari, K. (2016). What factors predict who will have a strong social network following a stroke? Journal of Speech, Language, and Hearing Research, 59, 772–783.
- Northcott, S., Moss, B., Harrison, K., & Hilari, K. (2016). A systematic review of the impact of stroke on social support and social networks: Associated factors and patterns of change. Clinical Rehabilitation, 30, 811–831.
- Nussbaum, J. (1994). Friendship in older adulthood. In M. L. Hummert, J. M. Wiemann, & J. F. Nussbaum (Eds.), Interpersonal communication in older adulthood: Interdisciplinary theory and research (pp. 209–225). Thousand Oaks, CA: Sage.
- O’Connor, K., & Chamberlain, K. (2000). Dimensions and discourses of meaning in life: Approaching meaning from qualitative perspectives. In G. T. Reker & K. Chamberlain (Eds.), Exploring existential meaning: Optimising human development across the life span (pp. 75–91). Thousand Oaks, CA: Sage.
- Ouellet, M., Morin, C., & Lavoie, A. (2009). Volunteer work and psychological health following traumatic brain injury. Journal of Head Trauma Rehabilitation, 24, 262–271.
- Palmer, S., & Herbert, C. (2016). Friendships and intimacy: Promoting the maintenance and development of relationships in residential neurorehabilitation. NeuroRehabilitation, 38, 291–298.
- Paterson, J., & Stewart, J. (2002). Adults with acquired brain injury: Perceptions of their social world. Rehabilitation Nursing, 27(1), 13–18.
- Perdices, M., & Tate, R. L. (2009). Single-subject designs as a tool for evidence-based clinical practice: Are they unrecognised and undervalued? Neuropsychological Rehabilitation, 19, 904–927.
- Pierce, C., & Hanks, R. (2006). Life satisfaction after traumatic brain injury and the World health Organization model of disability. American Journal of Physical Medicine and Rehabilitation, 85, 889–898.
- Ponsford, J., Draper, K., & Schönberger, M. (2008). Functional outcome 10 years after traumatic brain injury: Its relationship with demographic, injury severity, and cognitive and emotional status. Journal of the International Neuropsychological Society, 14, 233–242.
- Pound, P., Gompertz, P., & Ebrahim, S. (1998). A patient-centred study of the consequences of stroke. Clinical Rehabilitation, 12(4), 338–347.
- Powell, J. M., Rich, T. J., & Wise, E. K. (2016). Effectiveness of occupation- and activity-based interventions to improve everyday activities and social participation for people with traumatic brain injury: A systematic review. American Journal of Occupational Therapy, 70, 31–40.
- Pozzebon, M., Douglas, J., & Ames, D. (2016). Spouses’ experience of living with a Partner diagnosed with a dementia: A synthesis of the qualitative research. International Psychogeriatrics, 28, 537–556.
- Pozzebon, M., Douglas, J., & Ames, D. (2018). Facing the challenges of primary Progressive aphasia: The spousal perspective. Journal of Speech, Language, and Hearing Research, 61(9), 2292–2312.
- Public Health England (PHE). (2018). Briefing document. First incidence of stroke: Estimates for England 2007–2016. London: PHE.
- Salas, C., Casassus, M., Rowlands, L., Pimm, S., & Flanagan, D. (2018). “Relating through sameness”: a qualitative study of friendship and social isolation in chronic traumatic brain injury. Neuropsychological Rehabilitation, 28, 1161–1178.
- Sarre, S., Redlich, C., Tinker, A., Sadler, E., Bhalla, A., & McKevitt, C. (2014). A systematic review of qualitative studies on adjusting after stroke: Lessons for the study of resilience. Disability and Rehabilitation, 36, 716–726.
- Shorland, J., & Douglas, J. (2010). Understanding the role of communication in maintaining and forming friendships following traumatic brain injury. Brain Injury, 24(4), 569–580.
- Snow, P., & Douglas, J. (2017). Psychosocial aspects of pragmatic disorders. In L. Cummings (Ed.), Research in clinical Pragmatics, series: Perspectives in Pragmatics, Philosophy & Psychology, Vol. 11. Cham: Springer-Verlag. ISBN: 978-3-319-47487-8 (hardcover); 978-3-319-47489-2 (eBook), (617-649).
- Snow, P., Douglas, J., & Ponsford, J. (1997). Procedural discourse following traumatic brain injury. Aphasiology, 11, 947–967.
- Snow, P., Douglas, J., & Ponsford, J. (1998). Conversational discourse abilities following severe traumatic brain injury: a follow up study. Brain Injury, 12, 911–935.
- Snow, P., Douglas, J., & Ponsford, J. (1999). Narrative discourse following severe traumatic brain injury: A longitudinal follow-up. Aphasiology, 13, 529–551.
- Steadman-Pare, D., Colantonio, A., Ratcliff, G., Chase, S., & Vernich, L. (2001). Factors associated with perceived quality of life many years after traumatic brain injury. Journal of Head Trauma Rehabilitation, 16, 330–342.
- Struchen, M., Davis, L., Bogaards, J., Hudler Hall, T., Clark, A., Mazzei, D., … Caroselli, J. (2011). Making Connections After Brain Injury. Journal of Head Trauma Rehabilitation, 26, 4–19.
- Tashakkori, A. (2009). Are We There Yet?. Journal of Mixed Methods Research, 3, 287–291.
- Tashakkori, A., & Teddlie, C. ( Eds.) (2010). SAGE Handbook of mixed methods in social & Behavioral research (2nd ed.). Thousand Oaks, CA: Sage.
- Tate, R., Broe, G., Cameron, I., Hodgkinson, A., & Soo, C. (2005). Pre-injury, injury and early post-injury predictors of long-term functional and psychosocial recovery after severe traumatic brain injury. Brain Impairment, 6, 75–89.
- Tate, R., Kennedy, M., Ponsford, J., Douglas, J., Velikonja, M., Bayley, M., & Stergiou-Kita, M. On behalf of the INCOG Expert Panel (2014). INCOG Recommendations for Management of Cognition Following Traumatic Brain Injury, Part III. Journal of Head Trauma Rehabilitation, 29(4), 338–352.
- Tate, R., Lulham, J., Broe, G., Strettles, B., & Pfaff, A. (1989). Psychosocial outcome for the survivors of severe blunt head injury: The results from a consecutive series of 100 patients. Journal of Neurology, Neurosurgery, and Psychiatry, 52, 1128–1134.
- Tate, R., Wakim, D., & Genders, M. (2014). A systematic review of the Efficacy of community-based, leisure/social activity Programmes for people with traumatic brain injury. Brain Impairment, 15, 157–176.
- Thomas, M. (2004). The potential unlimited programme: An outdoor experiential education and group work approach that facilitates adjustment to brain injury. Brain Injury, 18, 1271–1286.
- Togher, L., Wiseman-Hakes, C., Douglas, J., Stergiou-Kita, M., Ponsford, J., Teasell, R., … Turkstra, L. (2014). INCOG Recommendations for Management of Cognition Following Traumatic Brain Injury, Part IV. Journal of Head Trauma Rehabilitation, 29(4), 353–368.
- Umberson, D., & Montez, J. (2010). Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior, 51, S54–S66.
- Umberson, D., Williams, K., Powers, D., Liu, H., & Needham, B. (2006). You make me sick: Marital quality and health over the life course. Journal of Health and Social Behavior, 47, 1–16.
- Willmott, P. (1987). Friendship networks and social support. London: Policy Studies Institute.
- Willmott, C., Ponsford, J., Downing, M., & Carty, M. (2014). Frequency and quality of return to study following traumatic brain injury. Journal of Head Trauma Rehabilitation, 29, 248–256.