ABSTRACT
Providing long-term care for a family member diagnosed with a Prolonged Disorder of Consciousness (PDoC) can have a significant impact on the lives of family caregivers. This scoping review aimed to explore the current literature investigating the impact of caring for a person in a PDoC on family caregivers’ Quality of Life (QOL), as categorized using the WHOQOL-BREF model. We observed that articles employing quantitative methodologies mostly reported QOL outcomes relating to negative feelings, thinking, learning, memory and concentration, and personal relationships. Articles employing qualitative methodologies mostly reported QOL outcomes relating to negative feelings, personal relationships, positive feelings, and health and social care accessibility and quality. A descriptive content analysis of the QOL outcomes highlighted the limitations of the current literature base in representing the complexities of the experiences of family members providing care for a person in a PDoC. To provide valuable and personalized support to caregivers, without pathologizing or medicalizing their distress, it is vital to characterize more accurately the contextual subtleties of each person’s situation.
Introduction
Every year in the UK around 10,000 people are admitted to hospital with a moderate or severe head injury (National Institute for Health and Care Excellence, Citation2014). Due to advances in medical treatments, many of these individuals are now surviving the acute causes of their head injuries. However, a proportion of these survivors subsequently develop a disorder of consciousness (DoC) (Graham et al., Citation2015) due to their underlying acquired brain injury (ABI). Consciousness is defined as a state comprised of both wakefulness (eyes open and some arousal) and awareness (of the self or the surrounding environment) (Royal College of Physicians, Citation2020). People displaying an impairment in one or both elements of consciousness will receive a DoC diagnosis, with a diagnosis of prolonged disorder of consciousness (PDoC) currently given in the UK to anyone who remains in a DoC for longer than a month (Royal College of Physicians, Citation2020). It is estimated that the PDoC incidence and prevalence rates in England and Wales are approximately 5 people per 100,000 a year (Wade, Citation2018).
The challenges associated with providing long-term care for a loved one with an ABI can have severe adverse implications for family caregivers (Larkin et al., Citation2018). People recovering from ABIs can require extra support for many years, potentially permanently, with the majority of this support usually provided by unpaid family members (DeJong et al., Citation1990). Under these circumstances, it is reported that many families make significant personal sacrifices to provide appropriate care for their injured family member (Boschen et al., Citation2007). This undoubtedly has an impact on the mental health of these family members, with research reporting that a significant proportion of family caregivers of people with traumatic brain injuries (TBI) experience clinically significant emotional distress (Chan et al., Citation2009).
Although distress responses vary between individuals, it has been found that family caregivers who report a greater burden associated with providing care to a relative post-ABI also report having a significantly poorer health-related quality of life (QOL) (Mar et al., Citation2011). Similarly, family caregivers of people with more severe behavioural, communication and social difficulties post-brain injury report higher levels of psychological distress (Anderson et al., Citation2002). Therefore, it is not surprising that a recent systematic review found that many family caregivers of people diagnosed with a PDoC, a state in which individuals have the most severe functional deficits, experience significant changes in their QOL associated with high levels of emotional distress and burden (Soeterik et al., Citation2017).
While the findings of this quantitative systematic review provided a valuable insight into the psychological distress experienced by caregivers, we know that caring for a person with a brain injury can have complex effects on families’ lives (Larkin et al., Citation2018). Qualitative research suggests that family members of people diagnosed with a PDoC experience a complicated and conflicting emotional journey, arising from processing the ambiguous clinical situation in which the person lacks consciousness but is still alive (Hamama-Raz et al., Citation2013). This led the authors of the systematic review to question whether current research is focussing on the “right variables” (Soeterik et al., Citation2017, p. 1383). Indeed, given the severity of disability that leads to a PDoC diagnosis, it should not be assumed that the impact of being a family caregiver for a person with a PDoC diagnosis is represented by the findings of the general ABI or caregiving literature. To provide the most appropriate and useful support to families of people diagnosed with a PDoC, clinicians must understand the range of psychological, social, and practical outcomes that families experience as caregivers in this context (Kitzinger & Kitzinger, Citation2014).
To comprehensively address this topic, we conducted a systematic scoping review using an adapted version of the Arksey and O'Malley (Citation2005) scoping study framework as a guide. Scoping reviews enable researchers to map the existing literature in a given area, highlighting central ideas as well as potential gaps (Daudt et al., Citation2013). This approach allows us to achieve our aim of taking a wide view of the quantitative and qualitative literature, thereby informing future research directions, and supporting an evidence-based understanding of the experiences of family caregivers of people diagnosed with a PDoC. Consequently, our review addresses the following research question: what does the current literature tell us about the impact of PDoC on family caregiver's QOL? Furthermore, what key QOL outcomes have been addressed by researchers in this area, and which outcomes have a more limited, or absent, literature base?
Materials and methods
We used the Arksey and O'Malley (Citation2005) scoping study framework to guide our review methods, with some suggested modifications as proposed by Levac et al. (Citation2010) and Daudt et al. (Citation2013). This framework consists of six stages: (1) specifying the research question, (2) identifying relevant articles, (3) selecting the applicable articles, (4) extracting the data, (5) collating, summarizing, and reporting the results and (6) optional consultation with key stakeholders (Arksey & O'Malley, Citation2005). This review was conducted as part of the first author’s Master of Research degree; therefore, a protocol was developed based on the above framework but was not published. We structure this scoping review report in line with the Joanna Briggs Institute format (Peters et al., Citation2020).
Eligibility criteria
In keeping with the Arksey and O'Malley (Citation2005) recommendation to maintain a broad review scope, we aimed to comprehensively examine the research literature that investigates the impact of PDoC on family caregiver's QOL. Therefore, article inclusion was not constrained by the type of evidence. There was also no restriction on the publication date for article inclusion. All searches were limited to English language.
To clarify the scope of our review, the key population, concept, and context eligibility criteria were defined as follows.
Population
Articles were included in our review if their focal population was adult (aged 18+) family caregivers of people diagnosed with a PDoC. For the purposes of this review, the UK PDoC national clinical guidelines definition of family caregivers was used: “anyone who has a sufficiently close relationship with the patient to be actively concerned with their management and wellbeing” (Royal College of Physicians, Citation2020, p. 22). This is in line with the inclusion criteria of the related systematic review conducted by Soeterik et al. (Citation2017).
Concept
For the purposes of our scoping review, we used the WHOQOL-BREF model (WHOQOL Group, Citation1998) to guide our definition of QOL. This model proposes multiple facets of QOL in four domains: physical health, psychological, social, and environment. Articles were included in our review if they reported QOL outcomes addressing any of the facets within these four domains. See supplementary materials appendix 1 for the full list of WHOQOL-BREF domains and facets.
Context
Articles were included in our review if they focused on family caregiving in the context of a PDoC diagnosis. For the purposes of our review, we used the definition of PDoC provided by the recent Royal College of Physicians (Citation2020) clinical guidelines: a diagnosis given when the person has remained unconscious for more than 4 weeks following a sudden onset ABI. This includes the Vegetative State (VS), Minimally Conscious State (MCS) and Emerging MCS (Royal College of Physicians, Citation2020). As with Soeterik et al. (Citation2017), articles using traditional or international PDoC diagnostic terminology (e.g., unresponsive wakefulness syndrome) were also included to ensure a comprehensive coverage of the PDoC literature.
As coma is usually considered an acute DoC (Giacino et al., Citation2014), articles focusing on family caregiving in the context of coma were only included if the PDoC timeframe was met. In the interest of homogeneity, articles investigating family caregivers of people diagnosed with locked-in syndrome, or a DoC caused by a degenerative disease, were not included in our review as these diagnoses are outside of the Royal College of Physicians (Citation2020) definition of PDoC. Healthcare context was not considered during the inclusion or exclusion of articles.
Search strategy
As recommended by Peters et al. (Citation2020), an initial search was conducted via two online databases; PsycINFO and Web of Science, using broad search terms covering the population, concept, and context of the research question. These terms were chosen through discussion with research experts in this field. The titles, abstracts and index terms of the articles identified in this search were analyzed to determine keywords and phrases to be included as search terms in the full literature search. Based on the number of articles retrieved from the initial searches, we decided to conduct the full search using only the population and context search terms to increase the breadth of coverage.
A full search was subsequently conducted across all the relevant online databases (PsycINFO, Web of Science, PubMed, AMED, CINAHL Plus and Medline) on 30 and 31 July 2020 using the key search terms identified in step 1 (see supplementary materials appendix 2). An example search strategy is provided in supplementary materials appendix 3. An online search was also conducted using the same search terms to identify relevant grey literature, including: theses and dissertations (OATD, OpenThesis, EThOS), conference papers (ZETOC, Web of Science), preprints (medRxiv, preprints.org) and other relevant sources (OpenGrey, Bielefeld Academic Search Engine, Tripdatabase.com). Any additional keywords and phrases identified from relevant articles during these searches were included iteratively as search terms to improve the scope of the review coverage.
The lead reviewer (AC) searched the reference lists of all the articles included in the review for additional unidentified, relevant sources. Due to resource limitations, we were not able to contact the authors of the articles included in the review for further sources of information.
Source of evidence selection
All search results identified via the above search strategy were exported into Endnote and duplicate entries were removed by the lead reviewer. The remaining articles were reviewed, and selected for inclusion, using our specified eligibility criteria. In line with Peters et al. (Citation2020) scoping review methodology recommendations, two reviewers (AC and RP) completed both stages of article selection independently. Firstly, the titles and abstracts of all the articles were screened, with those not meeting the inclusion criteria excluded at this point. The full text of each article that passed the title/abstract screen was then obtained and examined for eligibility. Articles that passed this full-text screen were included in the review.
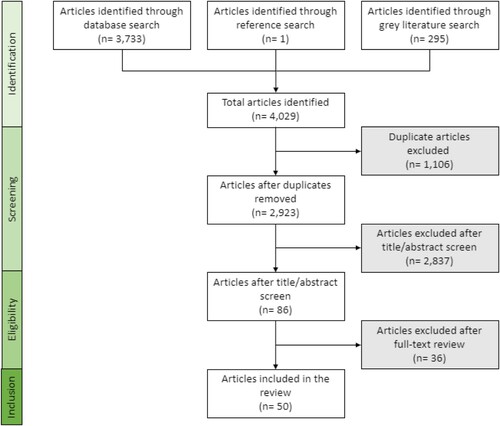
Discrepancies after the title/abstract screen were decided based on a comparison of comments provided by both reviewers. Discrepancies after the full-text screen (10.6% of the articles) were discussed by both reviewers to reach a consensus. See for a flow diagram, adapted from the PRISMA statement (Moher et al., Citation2009), detailing the number of articles included and excluded at each stage of the screening process.
Data extraction
The necessary data were extracted from the included articles using a data extraction form developed by the lead reviewer (see supplementary materials appendix 4) based on the JBI extraction instrument template (Peters et al., Citation2020). As recommended by Arksey and O'Malley (Citation2005), the data extraction form was designed to capture general information about the articles (e.g., names of authors, publication year, article type), as well as information directly relating to the research question (e.g., QOL outcomes assessed). The data extraction form was piloted on a small number of articles, and updated to improve functionality, prior to conducting the full search.
It is recommended that at least two reviewers complete the data extraction process (Peters et al., Citation2020). However, full data extraction by two reviewers was not feasible for this scoping review due to resource limitations. Instead, the lead reviewer extracted data from all the included articles, with the second reviewer (RP) independently extracting data from approximately half (48%) of the articles. Data extracted by each reviewer were compared to ensure replicability. On average the extracted general article data was 89.73% concordant between the reviewers, and the research data was 75% concordant. The lead reviewer then coded the extracted data against the WHOQOL-BREF facets.
Analysis and presentation of results
We conducted both quantitative and qualitative descriptive analyses of the extracted data as recommended by Arksey and O'Malley (Citation2005). For the quantitative analysis, frequency counts and averages were generated from the extracted article data to provide a detailed summary of the characteristics of the articles included in our review (Levac et al., Citation2010). To quantitatively report on the concept of our research question (QOL outcomes), frequency counts and percentages were generated to capture the number of articles addressing each outcome domain and facet from the WHOQOL-BREF model (WHOQOL Group, Citation1998).
For the qualitative summary, a descriptive content analysis was completed based on the method recommended by Sandelowski (Citation2000). Using this approach, we generated key themes reported across the articles using the WHOQOL-BREF domains as a template. This was an iterative process requiring multiple reviews of the extracted data, as well as the original articles. Altogether, this process ensured that the themes generated were driven by the article data itself, adapting the pre-existing WHOQOL-BREF coding system.
As scoping reviews aim to describe, not synthesize, available information (Peters et al., Citation2020), we deemed the above combination of methodologies to be the most appropriate to provide an overview of the range of research literature available. Unlike systematic reviews, scoping reviews do not aim to provide an assessment of the quality of the articles included (Arksey & O'Malley, Citation2005). Therefore, we did not conduct any quantitative analyses of article methodological quality for this scoping review.
Presentation of the results
We decided to present the results of the above quantitative analyses in tabular and narrative formats for clarity, divided by methodology to aid comparison. Based on Pelentsov et al. (Citation2015), a complete list of all the articles included in our review and their key characteristics is provided in a separate table (see supplementary materials appendix 5 – article reference numbers in superscript below correspond to this table). For the summary of the qualitative content analysis, we divided the narrative into WHOQOL-BREF domains, sub-divided by the generated themes.
Results
Characteristics of sources of evidence
General article characteristics
In total, 50 articles met the criteria for inclusion in this scoping review. The majority of these were journal articles (n = 44) but, due to the wide scope of our review, conference abstracts (n = 4), thesis chapters (n = 1) and book chapters (n = 1) were also included. Half (n = 25) of the articles were systematic quantitative studies, the other half of the articles consisted of qualitative studies (n = 11), commentaries/opinions (n = 8), case studies (n = 3), mixed-methods studies (n = 2) and a systematic review (n = 1). All the articles included in our review were published between 1990 and 2020. Only one article was published in the period 1990–1999, with six published in 2000–2009 and 43 published in 2010–2020. The geographical spread of the articles was not even, with half (n = 25) of the articles originating from Italy. This is thought to be due to multiple Italian research groups publishing on this topic, and the existence of two large-scale national Italian studies into VS and MCS (Covelli et al., Citation2016). The remaining half of the articles originated from nine different countries: UK (n = 7), USA (n = 4), Germany (n = 3), Iran (n = 3), Israel (n = 2), Norway (n = 2), Spain (n = 2), Brazil (n = 1) and China (n = 1).
Population characteristics
Most of the articles (n = 44) focussed on specific cohorts of family caregivers, ranging from one12,25,32,38 to 48717,27 caregivers, with some articles reporting on the same cohorts of family caregivers. Five articles did not report on specific cohorts of caregivers; instead, they provided personal reflections on family caregiving in the context of PDoC and/or the existing PDoC caregiving literature base10,11,24,43,50. Overall, family caregivers were mostly female and from across the adult lifespan (age range of 18–84). Family caregiver gender was reported in 39 articles, and age in 35 articles; however, caregiver ethnicity was only reported by three articles.
Thirty-eight of the articles reported the family caregivers’ relationship status with the person diagnosed with a PDoC. Of these, approximately 40% of the family caregivers were the individual’s spouse or partner, 20% were the individual’s parent, and 18% were the individual’s child. The remaining ∼22% was made up of siblings, extended family members (e.g., grandparents, nieces, and in-laws), friends and professional caregiversFootnoteA. A small proportion of the articles (n = 11) reported the caregiving time provided by the family caregivers – this ranged between 1 hour a week42 and 24 hours a day9,16,19,27.
Context characteristics
Although all the articles considered caregiving in the context of a PDoC diagnosis, only 36 articles reported specific diagnoses. Across these articles, the average percentage of people with a VS diagnosis was 77.1%, and the average percentage of people with an MCS diagnosis was 22.9%. In the 21 articles reporting the cause of the brain injury, the split between TBI and non-traumatic ABI (NT-ABI) varied greatly but overall was roughly equal (average percentage TBI 52.65%, NT-ABI 47.36%). NT-ABI included a range of aetiologies including anoxia, vascular events, and infections. Time post-injury ranged from 1.2 months9 to 27 years9,46. Healthcare settings included specialist long-term care units, rehabilitation centres and nursing homes, as well as within the family home.
Concept characteristics
Across the 50 articles included in our review, QOL outcomes covering all four of the WHOQOL-BREF (WHOQOL Group, Citation1998) domains were reported. The psychological domain was the most addressed, with almost every article (n = 49) reporting at least one psychological outcome. Although the physical health domain was the least frequently addressed, 30 articles still reported on at least one physical health outcome. Negative feelings, personal relationships and financial resources were the facets most reported upon across all the domains.
However, when the articles were divided by their methodologies, the prioritization of facets was not equal. For articles employing quantitative methodologies the facets most reported on were negative feelings, thinking, learning, memory & concentration, and personal relationships. For the articles employing more qualitative methodologies the most reported on facets were negative feelings, personal relationships, positive feelings, and health and social care: accessibility and quality. This suggests a potential disparity between the focus of systematic research in this area, and what caregivers and experts by experience denote as important. See for a detailed breakdown of the number of articles addressing each WHOQOL domain and facet.
Table 1. Table showing the number of articles addressing each domain, and the percentage of all articles, per article methodology, with outcomes addressing each WHOQOL facet (WHOQOL Group, Citation1998).
It should be noted that each individual article may address more than one facet, both within a domain and across domains. Also, some additional facets were added by the reviewer to capture article results that addressed the domain but did not fall into any specific facet.
Qualitative summary of sources of evidence
The themes generated from the descriptive content analysis are presented individually below within each WHOQOL domain. See for a summary of articles contributing to each theme.
Table 2. A summary of the themes identified in the content analysis within each WHOQOL domain (WHOQOL Group, Citation1998), and the percentage of articles within the domain that contributed to each theme by methodology.
Physical health
“Caring as a barrier to employment and occupational productivity”
This theme was contributed to by 42.9% of the quantitative articles, compared to 29.2% of the qualitative articles. Due to the broad age spectrum of people with a PDoC, many family caregivers in the articles were within the working age range. However, up to 65.7% of the caregivers reported having to resign from their jobs19, either temporarily or permanently, to provide care9,16,23,24,27,31,33,36,38. In one longitudinal study caregiver employment status did improve over time, however still only 42.6% of caregivers were in paid employment by the end of the study9. Even when caregivers did remain in paid employment, some reported experiencing severe difficulties functioning at work due to the ongoing emotional strain18,42,44. As well as affecting the employment of the primary caregiver, two articles reported that caring for an individual in a PDoC impacted significantly on the productivity of the wider family, with siblings dropping out of school to help cover care costs21,36.
“Physical impact”
Across the 18 quantitative and qualitative articles that contributed to this theme, eight investigated the physical manifestation of caregiver burden via increased psychosomatic28,50 and other physical symptoms. These included regular occurrences of insomnia, sleep disturbances and fatigue5,7,15,21,32, digestive problems5, headaches5, eczema15 and general physical stress15,24. However, caregivers self-reported ratings of their own physical health were variable. In three articles caregivers’ perceived physical health scores, measured using the standardized SF-12 questionnaire (Ware et al., Citation1996), were in line with population norms17,19,40, whereas in another article using the same measure they were reported as significantly lower27. In one longitudinal study, the impact of caring on caregivers self-rated health was found to become more of an issue over time15. Caregivers’ self-reported health satisfaction ratings were observed in another study using a standardized life satisfaction questionnaire (the FLZ) (Fahrenberg et al., Citation2000) to vary depending on the healthcare setting, with those caring for people within institutional care settings scoring lower than homecare settings, and lower than the population norm47. Two qualitative articles also highlighted the physicality of caring for individuals with such extensive and complex needs as a significant issue for caregivers32, with one article reporting physical injuries e.g., backache and arm/knee injuries, caused through the caring role21.
“Disrupted daily life”
In both the quantitative and qualitative articles, a significant negative impact of caring on caregivers’ daily activities and lifestyle is reported4,8,15,18,38,42,50. Due to the prioritization of patient-related activities, caregivers in three articles reported a reduction in their own lives to a point where their basic needs of self-care15,21 and nutrition21,32,50 were not always met. Adapting to these life changes can be extremely challenging, with one family highlighting the “life abdication” that was required to accommodate their new caring roles (Oliveira et al., Citation2020, p. 104). However, one longitudinal study suggested that, between 6 and 12-months post-injury, family caregivers begin to re-establish more sustainable daily routines and activities, moving away from a need to live day-to-day15. Overall, these issues of disruption and burden on caregivers’ daily lives were raised in 37.5% of the qualitative articles, compared to only 10.7% of the quantitative articles.
Psychological
“Psychological distress and burden”
Psychological distress was the most investigated outcome across all the articles, but more often this was by articles employing quantitative methodologies. Caregivers scored significantly high on a variety of standardized measures of depressive symptoms in 21 articles, and anxiety in 20 articles, with depression strongly predicting low QOL45. Twelve articles also reported increased incidence of Prolonged Grief Disorder (PGD) in cohorts of family caregivers of people with a PDoC using the standardized PGD measure, the PG-12 (Prigerson et al., Citation2008), with up to 60.4% of caregivers meeting the criteria for this disorder in one study14. In the only randomized control trial included in this review, caregivers’ psychological distress, measured using the Symptom Checklist-90-R (SCL-90-R) (Derogatis & Savitz, Citation1999), was significantly higher than normal at baseline but improved to near normative levels following a single-session group therapeutic intervention28. Distress is not limited to the primary caregiver, with significant effects on the mental health of the extended family also reported21.
Other psychological symptoms and disorders were also reported by caregivers, including: Post-Traumatic Stress Disorder (PTSD)22, anger20,31,45, psychophysiological symptoms28,33,34,35, hopelessness41, guilt32, and extreme behavioural responses15. One study also investigated the impact of caring for a person in a PDoC on family caregivers’ cognitive function, reporting a negative effect on tasks requiring attention, executive function, and verbal fluency and visuo-spatial memory35. Caregivers’ self-reported ratings of their own mental health were lower than the reference norms in three articles16,27,42, but two longitudinal studies suggest that caregivers’ self-reported mental health scores improve over time6,9. Another study found that caregivers mental health was inversely related to caregiving duration and associated with their family member’s location of residence17. The impact of time on emotional burden varied between the articles, with some suggesting that caregivers’ emotional burden worsens over time1,2, some suggesting emotional burden lessens over time9 and some suggesting it stays roughly the same45. One qualitative study reported that the emotional wellbeing of the caregiver echoed the medical state of the person in a PDoC15 which may suggest why these results are not consistent.
Using the short form of the Family Strain Questionnaire (FSQ-SF) (Vidotto et al., Citation2010), the majority of caregivers in two separate studies were assessed to be in need of psychological support, with 46.15%1 and 18%3 of the respective cohorts reported to be in urgent need. When asked about access to psychological support, 34.3% of caregivers in one study reported having access9, and 17.6% of caregivers in another study reported having asked for psychological support within the first year of caregiving4. Although many caregivers may, and indeed do, benefit from professional psychological help, it must be noted that the pathologization and medicalization of legitimate responses to a traumatic situation was also reported to increase caregivers’ distress25,26.
“Internal resources for coping”
The quantitative studies tended to focus on investigating the coping strategies employed by family caregivers using various versions of the COPE questionnaire (Carver, Citation1997; Sica et al., Citation1997). Overall, caregivers used problem-focussed and emotion-focussed coping strategies most frequently3,9,14,16,19,27,33,45, with avoidance/disengagement and humour used least frequently3,9,13,27,33. One study suggested that this may vary based on the diagnosis, with caregivers of people in a VS using avoidant coping strategies significantly more than caregivers of people in a MCS17, but another found no differences between caregiver groups47. Significant correlations were also reported between psychological distress and types of coping strategy used. Greater burden was positively associated with avoidance9, and anxiety, depression and PGD were positively associated with denial and self-blame13,14,45, but negatively associated with acceptance13,14. However, one study did not find any correlation between coping strategies and emotional burden42.
Only qualitative articles highlighted caregivers’ discovery of an unknown internal strength that enabled them to cope with the process of caring and the positive impact that this had on their self-esteem8,10,18,23,25,30. Religion as a coping strategy was referred to in both quantitative and qualitative articles. Three articles reported that faith helped caregivers cope and reason with their current situation32,38,50, with another reporting that use of spiritual support was associated with fewer sleep disturbances7. However, in two articles caregivers reported that religion either provided them no support2 or they did not use it as a strategy at all36.
“Loss without death”
A strong theme emerging from the qualitative articles was the complicated emotional processing that caregivers endure as a result of experiencing a bereavement without the ability to mourn10,23,24. Caregivers’ report struggling with conflicting emotions associated with a “living loss” (Crow, Citation2006, p. 185), including sorrow at the loss of the person the individual was before, while still hoping for improvements and feeling guilty when this hope diminishes20,23,25. Caregivers in one article described the situation as “worse than a death” (Soeterik et al., Citation2018, p. 1398) due to the ambiguous prognosis and constant threat of medical complications and death. In two quantitative studies, caregivers were reported to experience significant difficulties with making sense of the meaning of their own life in the context of the person’s diagnosis and ongoing condition44,47. These findings are consistent with the theory of ambiguous loss (Boss, Citation2007) where uncertainty about an individual’s state of presence obstructs grief and decision-making processes for those close to them.
The situation is further complicated by the difference in perceptions and reactions between family caregivers and medical professionals30,36, or between family members10, which can cause significant frustration, anger, and feelings of abandonment. These conflicts often arise around decisions regarding the continuation or withdrawal of life-sustaining treatments. One article reports significant distress caused to caregivers by the artificial medical maintenance of the person in a state they would not wish to be in26. However, in another article, five caregivers reported wanting to continue with life-sustaining treatments, regardless of what they thought the individual would want, rather than face losing them4.
“Time as a source of pain and healing”
Qualitatively, time was first seen as a source of pain for caregivers, with many articles reporting that caregivers lived day-to-day and avoided thinking about the future8,18,23,46. This enabled them to cope with the ongoing emotional challenges of the diagnosis and caregiving, supported by hope for a positive outcome. Generally, increasing time post-diagnosis led to an abandonment of hope for recovery10,20. One article reported that caregivers’ initial hope for a good outcome decreased at around 4–6 months post-injury11, and another reported that 45.8% of caregivers lost hope in the first year of caregiving4. For some caregivers, this decline in hope led to feelings of guilt at having given up on the individual12,25, but others reported shifting to smaller hopes for more attainable outcomes29,30.
As caregivers’ perspectives on the person’s prognosis changed, their realization of the situation resulted in feelings of devastation25, but also acceptance29,32. This acceptance allowed caregivers to start a process of renormalization in their daily lives, but also led to feelings of guilt at spending less time with their family member15. Quantitatively, caregivers’ overall needs, measured using the Caregivers Needs Assessment (Moroni et al., Citation2008), were reported to decrease over time, but only for caregivers of people in a VS6. Caregivers’ overall QOL was also reported to decrease over time1.
Social
“Social support: old and new relationships”
Caregivers’ need for, and sources of, social support were covered both quantitatively and qualitatively by almost every article in this domain. The deterioration of personal relationships was highlighted as a key issue4,8,18, and relationship quality was rated as significantly lower than normal in three articles using standardized measures2,16,17. Interpersonal hostility and sensitivity were reported to be high in seven articles both quantitatively using the SCL-90-R (Derogatis & Savitz, Citation1999)7,28, and qualitatively21,50. This was a particular issue within families due to differing emotional reactions to the person’s diagnosis10,20 and the prioritization of patient-related activities30. Some caregivers also reported the noticeable impact of their own coping on their wider family4, sometimes leading to the primary caregiver hiding their emotions from their family to protect them23.
Problems with social involvement and functioning were also described as a significant issue for caregivers2,5,9,27,33,42,44, with over 70% of caregivers in one article reporting a lack of opportunities to socialize2. Over time this led to increased social isolation for caregivers10,21,36 and loss of friendships4,8,24. The decline in social involvement was positively correlated with caregivers’ depressive symptoms2,9, and with their family members living in institutional care settings4,17. Caregivers in three articles also highlighted the negative impact of caregiving on their social status and identity, with the loss of their previous roles at work and at home18,24,26.
The support of relatives was highlighted as crucial in allowing caregivers to begin to renormalize their lives15,30, with relatives providing a source of strength23,37 and sharing the caring burden12,32. Caregivers also developed new supportive relationships with other families experiencing similar situations, or more formally with care staff8,10,24. However, when assessed quantitively using the COPE (Sica et al., Citation1997), even though social support was found to be a useful coping strategy, it was not the most used by caregivers16,17. This may be in part due to a reported decline in social support over time37,38,45,50, especially following discharge from hospital48, therefore making it an unreliable resource. Perceived social support scores did not vary between caregivers of people with a PDoC or other chronic conditions in one study16, suggesting that this may be an issue for caregivers more generally.
“Changing relationship with their family member”
Caregivers qualitatively described the initial need to be physically close to the person with a PDoC to be able to sustain their emotional connection, and to communicate their needs4,18,20,24. This allows caregivers to maintain their bonds with their family member8,44, upholding the importance of their relationship through continued commitment and love23, which some saw as their duty4,32. For some caregivers, part of this duty was to ensure that the individual continued to receive social visitors30, or that their absence in other relationships was compensated for by the caregiver18,46 in order to uphold the person’s continued existence.
Over time, the nature of caregivers’ relationship with their family member was reported to adapt to their new roles, with many non-parent caregivers reporting to now see the person in a PDoC as a child-like figure8,18,23. Some caregivers expressed a nostalgia for their past relationship8, often due to the loss of their main emotional support figure12,23 and the un-reciprocal nature of the new relationship46. Caregivers’ need for physical closeness with the individual in a PDoC was reported to lessen over time15. In the only quantitative study addressing this topic it was found, using the adapted Boundary Ambiguity Scale (Soeterik, Citation2017), that all caregivers had high confusion about their new relationship with their family member, and 54.5% of caregivers were unsure of the role the person now had within the family unit44.
“Fractious relationships with medical staff”
This theme was only reported on by qualitative articles. Clashing opinions about the medical condition and prognosis of the person in a PDoC were reported to lead to the development of stressful, negative relationships between family caregivers and clinical teams10,11,30. For some caregivers, deterioration of this relationship causes a distrust and avoidance of medical staff4,18,29. However, other caregivers report experiencing positive relationships with staff, from which they receive significant emotional and practical support8,37. One article suggests that caregivers’ relationships with staff reflect their adjustment to their family member’s prognosis10. However, as this puts the responsibility of relationship solely on the caregiver, we suggest that this is too simple a view of these complex relationships.
Environmental
“A burdensome care system”
The largest proportion of articles contributing to this theme were qualitative, with 79.2% of the qualitative articles reporting at least one outcome relating to systemically caused burden. In these articles, many caregivers expressed a need for simplified care pathways, with the requirement to navigate complicated, bureaucratic systems to advocate for their family member’s needs being reported as a cause of excessive burden and strain8,24,48. The system made it challenging for caregivers to attain, and trust that the person in a PDoC would receive, suitable continuity of care26,48. This was heightened by a reported lack of access to medical teams12,36,37, adequate care resources32,37,48 and respite/support services16,48. However, some caregivers did report having access to good professional and peer support services5,9,23,38.
Challenges communicating with health and social care services29,46 and negative experiences of uncaring communications from medical staff4 also added to caregivers’ difficulties. Good communication between staff and caregivers through the longitudinal process of advance care planning was reported as vital in supporting families to understand, and cope with, a PDoC diagnosis43. Caregivers in one article highlighted their view of staff nurses not only as vital care facilitators but also educators37. However, in the quantitative studies, caregivers’ scores on the FSQ (Rossi Ferrario et al., Citation1998) indicated an elevated need for knowledge and information5,9,17,27,33,35, suggesting that ongoing communication with staff may not be happening for all caregivers. One study did find that caregivers informational need decreased over time9, but another found no change in this need over 8 months33.
“(lack of) time for self”
In both quantitative and qualitative articles, the negative impact of caregiving on caregivers’ personal interests was reported8,15,20,27,38,42. In one study, 62% of caregivers reported a lack of time for themselves5, which echoed the findings from two qualitative articles8,18. Some caregivers reported a lack of opportunity to engage in outdoor and leisure activities2 and low engagement with previous hobbies10. However, in one longitudinal study, the negative impact on caregiver’s self-reported leisure activities was found to be less severe at 12 months post-injury than at six months15. Caregivers in another study reported no change in their physical activity over time6.
Qualitatively, caregivers highlighted their experience of “domestic imprisonment” (Goudarzi et al., Citation2015, p. 4) due to caring becoming their only purpose in life12,26. This issue of time spent providing care was also investigated quantitatively where it was found that caregivers reported spending large numbers of hours providing care every day16,36, and this significantly predicted overall caregiver burden17,45. Lack of freedom was particularly prominent for home-caregivers47, and approximately 25% of caregivers in two studies reported that they had taken on the caring role because no-one else was able to do so27,33. Despite this huge amount of personal sacrifice, caregivers in two qualitative studies reported that for them caring was not seen as an obligation but something they wanted to do for their family member23,38.
“Financial pressures”
A strong theme across quantitative and qualitative articles was the negative impact of caring on caregivers’ financial situations5,8,9,16,19,21,27,29,36,45. In one study 50% of caregivers reported having experienced economic problems2, with two other articles reporting that caregivers experienced reduced incomes due to their caring roles23,24. In two Italian studies, between 40% and 47% of families reported incomes below the national average of €17,000 a year27,42. However, when asked to rate their own economic status on a Likert scale, over 80% of caregivers in six Italian and Spanish studies rated their financial situation as average or above average9,13,14,19,27,33. This was supported by another German study, which reported that caregivers’ self-reported satisfaction with their financial situation on the FLZ (Fahrenberg et al., Citation2000) was within the normal range47. On the other hand, it has also been reported that caregivers’ self-rated financial concerns increase over time1, so one-off ratings may not be representative long-term. The financial burden of caring for a person with a PDoC was also shown to extend beyond the primary caregiver, with other family members stepping in to provide financial support21,37,38.
Reasons for caregivers’ financial difficulties were reported qualitatively. This included the loss of the family breadwinner and the caregiver becoming the sole earner10,38. Another issue was the high costs of caring for people with extensive medical needs20,21,38. This was particularly challenging for those providing care at home32, and for caregivers reliant on medical insurance32,36 as the insurance cover was not always sufficient, leading to medical debt. Despite these difficulties, only around 15% of the caregivers in two quantitative studies reported receiving economic aid16,33. Qualitatively, one caregiver discussed the necessary prioritization of the family finances, often having to make personal sacrifices, to ensure their family member received the right care38. However, in another article where financial problems were regularly mentioned by caregivers, negatively rated QOL was not perceived as related to wealth11.
Discussion
Through this scoping review, we have identified a wide range of psychological, social, and practical QOL outcomes that families experience as caregivers of people with a PDoC. This supports the argument that to determine the best support for each caregiver in this situation, we need to understand the context in which care is provided (Kitzinger & Kitzinger, Citation2014). However, despite the quantity and variety of articles included in this review, it is likely that the systematic literature addressing caregiver QOL in the context of PDoC is limited to preconceived areas of importance and therefore not representative of the true clinical picture.
It is frequently documented in the quantitative literature that having a family member diagnosed with a PDoC is an extremely traumatic event, with many caregivers shown to experience high levels of psychological distress (Soeterik et al., Citation2017). Although the negative impact of caring on psychological QOL is a strong theme in the qualitative literature too, caregivers also discuss some positive psychological aspects. This included recognizing their own inner strength and ability to cope, which can lead to improvements in self-esteem, as well as seeing caring as a way to continue to show love and commitment to their family member. These positive outcomes should not be overlooked when systematically researching QOL impact, as understanding the factors that may be protective or motivational is paramount to a person-centred psychological formulation (Division of Clinical Psychology, Citation2011), from which appropriate support structures can be developed.
Similarly, although the quantitative literature did address some of the everyday difficulties experienced by caregivers, the themes focussing on practical issues (e.g., disrupted daily living, and themes in the environmental domain) were more frequently addressed qualitatively. This was particularly noticeable regarding the distress caused to caregivers by the healthcare system itself. Qualitatively, many caregivers reported significant burden associated with navigating complex, bureaucratic systems, and fighting to access necessary care and support. However, quantitatively, this was only investigated via caregivers self-reported informational needs. This divergence in focus between the article methodologies indicates that researchers, and perhaps clinicians, perceive caregivers in a much more passive role within the care system than the caregivers themselves.
It is important that future systematic research addresses caregivers’ needs for practical support as active participants within the care system. Developing capable environments (McGill et al., Citation2014) that support caregivers throughout their caring journey, rather than just focussing on points of psychological crises, will enable a more proactive approach to improving caregivers’ QOL and help to reduce the pathologization of their legitimate distress responses (Kitzinger & Kitzinger, Citation2014). It is worth noting that the majority of the quantitative articles included in our review were Italian (n = 20), in line with the previous review by Soeterik et al. (Citation2017), whereas the qualitative articles were more geographically mixed. Due to the varying healthcare contexts and cultural expectations of caregiving across countries, further research needs to be undertaken to understand the specific QOL impacts and caregiver needs within local contexts of health and community care services.
It is also important to mention that most of the quantitative articles included in this review employed self-report measures. Although this allows a systematic approach to investigating caregivers’ perceptions of their own situation, the results are potentially impacted by limited response options and subject bias. The combination of these errors may mask the true impact of caring in these studies. For example, quantitatively, caregivers’ self-rated financial status indicated that they perceived their financial situation as average or above (Covelli et al., Citation2016). However, qualitatively, caregivers reported experiencing significant financial difficulties due to caring for a person with extensive medical needs (Oliveira et al., Citation2020). Similarly, caregivers were often asked to quantitatively rate their perceived physical health, but the physicality of providing care was only reported qualitatively (Goudarzi et al., Citation2015; Martone, Citation2000). Therefore, it is important to consider how the question asked may lead to significantly different results, which in turn could impact on the perceived support needs of a specific group.
Similarly, it is important to consider who is represented by the research being conducted. Contextual factors such as ethnicity and socioeconomic status were reported on infrequently (or not at all) by the articles include in our review. However, these factors provide significant context to the experiences of caregivers. For example, Black Asian and Minority Ethnic (BAME) caregivers have been reported to face significantly more health challenges than their white counterparts (Carers UK, Citation2011). By insufficiently exploring these contextual aspects, the lessons that we take from the literature will be limited and could result in serious underestimations or misrepresentations of caregivers’ needs.
Finally, it may be beneficial for future research in this area to focus more on caregivers’ needs rather than just QOL outcomes. By applying a needs-based template, such as the Supportive Care Needs Framework (Pelentsov et al., Citation2015), researchers could help develop practical, person-centred guidance on how to best support families providing long-term care for relatives in a PDoC.
Limitations of this review
Altogether we found that the WHOQOL-BREF (WHOQOL Group, Citation1998) was an acceptable model to capture the breadth of QOL outcomes experienced by caregivers of people in a PDoC, and a useful template for guiding this review. However, using a template in this way does potentially limit the scope of the analysis beyond the pre-existing model. For example, we felt that some of our themes addressed key issues that crossed multiple domains e.g., fractious relationships with medical staff could be usefully included within a burdensome care system. These inter-domain relationships were similarly highlighted by the significant number of correlations between QOL outcomes in different domains e.g., the association between depressive symptoms and perceived economic problems (Magnani et al., Citation2020). This suggests that the lack of representation of interactional pathways between domains in the WHOQOL-BREF model may be too reductionist.
Future research, and clinical practice, would benefit from exploring the interaction between factors affecting caregivers’ QOL. As most of the articles in our review employed cross-sectional approaches, a key part of this will be improving the investigation of the longitudinal impact of caring on family caregivers of people in a PDoC. This will be particularly important given the large variation in time post-injury in the articles included in our review, which could impact on the relative importance of different risk or protective factors. Additionally, due to the international nature of the articles included in our review, our results are not specifically reflective of local, religious, health and social care or funding contexts. Understanding the development of QOL outcomes over time within the specific caregiving context is paramount given the prolonged nature of the disorder, and the likely significant impact of the local context on PDoC service availability and expectations of the role of the caregiver.
Due to practical limitations for this scoping study, we were unable to formally conduct the optional sixth stage of the Arksey and O'Malley (Citation2005) framework: consultation with relevant stakeholders. Therefore, our interpretations may be limited by our own perceptions and preconceptions. We tried to minimize the effect of this limitation by consulting with research colleagues who have expertize working with people in a PDoC to shape an appropriate review focus and scope. However, future research in this area would benefit from consultation with family caregivers, as well as clinical staff working in this area.
Although the Arksey and O'Malley (Citation2005) framework dismisses quality assessment as a necessary part of a scoping review, it has been argued that this limits the ability to comment on the clinical implications of scoping review results (Daudt et al., Citation2013). As the purpose of our review was to map the research literature in a specific area, and not necessarily to provide clinical recommendations, we did not feel that a quality assessment of included articles was essential. However, it would be recommended that any future research assessing literature quality in this area employs both quantitative and qualitative quality assessment tools due to the highly diverse article methodologies addressing this topic.
As with any literature review, scoping reviews are limited by the availability of relevant sources of information (Peters et al., Citation2020). Although we did include many diverse articles in our review, it is possible that by focusing our research question on understanding the academic literature we could have missed important sources of alternative information (e.g., narrative accounts published in popular literature). Similarly, due to our stringent inclusion and exclusion criteria, we excluded some articles that could have provided useful additional information (e.g., caregiving in the context of PDoC caused by a degenerative disease, or articles not reported in English). Although this provided the homogeneity of articles needed to address our research question, this may not accurately reflect the entire clinical picture.
Conclusion
The current literature demonstrates that caring for a person diagnosed with a PDoC can have a wide-ranging and considerable impact on family caregiver's QOL. However, to date, most research in this area has consisted of systematic quantitative investigations of the negative consequences of caring on caregivers’ physical and mental health. This limited focus and methodology overlooks significant complexities in caregivers’ emotional and practical experiences. Understanding these sometimes subtle, contextually sensitive occurrences is vital in providing personalized support to caregivers without pathologizing or medicalizing their distress.
Altogether, our scoping review highlights the need for future research to take a more systemic view of caregiving within the context of a PDoC diagnosis. Changing the focus of future research in this way will allow us to improve three key areas of understanding: the relational interactions between different QOL outcomes (including how these relationships change over time), the contextual and cultural factors influencing QOL outcomes, and the practical needs of caregivers within the caregiving system.
Supplemental Material
Download PDF (355.5 KB)Acknowledgements
We thank the University of Birmingham Clinical Psychology MRes team for their support and feedback on this project.
Disclosure statement
)In accordance with Taylor & Francis policy, we report that the research reported in this paper was submitted as a part of the lead author’s thesis for the degree of Master of Research at the University of Birmingham.
Additional information
Funding
Notes
1 A. Two articles including professional caregivers in their cohorts were accepted for inclusion in this review as the focus was deemed to be sufficiently on the impact of PDoC on family caregivers to meet the inclusion criteria.
References
- Anderson, M. I., Parmenter, T. R., & Mok, M. (2002). The relationship between neurobehavioural problems of severe traumatic brain injury (TBI), family functioning and the psychological well being of the spouse/caregiver: Path model analysis. Brain Injury, 16(9), 743–757. https://doi.org/10.1080/02699050210128906
- Arksey, H., & O'Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology: Theory & Practice, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616
- Boschen, K., Gargaro, J., Gan, C., Gerber, G., & Brandys, C. (2007). Family interventions after acquired brain injury and other chronic conditions: A critical appraisal of the quality of the evidence. NeuroRehabilitation, 22(1), 19–41. https://doi.org/10.3233/NRE-2007-22104
- Boss, P. (2007). Ambiguous loss theory: Challenges for scholars and practitioners. Family Relations, 56(2), 105–110. https://doi.org/10.1111/j.1741-3729.2007.00444.x
- Carers UK. (2011). Half a million voices: Improving support for BAME carers. Retrieved from Carers UK.
- Carver, C. S. (1997). You want to measure coping but your protocol's too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. https://doi.org/10.1207/s15327558ijbm0401_6
- Chan, J., Parmenter, T., & Stancliffe, R. (2009). The impact of traumatic brain injury on the mental health outcomes of individuals and their family carers. Australian e-Journal for the Advancement of Mental Health, 8(2), 155–164. https://doi.org/10.5172/jamh.8.2.155
- Covelli, V., Sattin, D., Giovannetti, A. M., Scaratti, C., Willems, M., & Leonardi, M. (2016). Caregiver's burden in disorders of consciousness: A longitudinal study. Acta Neurologica Scandinavica, 134(5), 352–359. https://doi.org/10.1111/ane.12550
- Crow, L. (2006). Extreme measures: A personal story of letting go. Death Studies, 30(2), 177–186. https://doi.org/10.1080/07481180500455657
- Daudt, H. M., van Mossel, C., & Scott, S. J. (2013). Enhancing the scoping study methodology: A large, inter-professional team's experience with Arksey and O'Malley's framework. BMC Medical Research Methodology, 13(1), 48. https://doi.org/10.1186/1471-2288-13-48
- DeJong, G., Batavia, A., & Williams, J. (1990). Who is responsible for the lifelong well-being of a person with a head injury? Journal of Head Trauma Rehabilitation, 5(1), 9–22. https://doi.org/10.1097/00001199-199003000-00004
- Derogatis, L. R., & Savitz, K. L. (1999). The SCL-90-R, brief symptom inventory, and matching clinical rating scales. In M. E. Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment (pp. 679–724). Lawrence Erlbaum Associates Publishers.
- Division of Clinical Psychology. (2011). Good practice guidelines on the use of psychological formulation. Leicester. British Psychological Society.
- Fahrenberg, J., Myrtek, M., Schumacher, J., & Brahler, E. (2000). Fragebogen zur lebenszufriedenheit (FLZ): handanweisung. Hogrefe.
- Giacino, J. T., Fins, J. J., Laureys, S., & Schiff, N. D. (2014). Disorders of consciousness after acquired brain injury: The state of the science. Nature Reviews Neurology, 10(2), 99–114. https://doi.org/10.1038/nrneurol.2013.279
- Goudarzi, F., Abedi, H., Zarea, K., & Ahmadi, F. (2015). Multiple victims: The result of caring patients in vegetative state. Iranian Red Crescent Medical Journal, 17(6), e23571. https://doi.org/10.5812/ircmj.23571
- Graham, M., Weijer, C., Peterson, A., Naci, L., Cruse, D., Fernandez-Espejo, D., Gonzalez-Lara, L., & Owen, A. M. (2015). Acknowledging awareness: Informing families of individual research results for patients in the vegetative state. Journal of Medical Ethics: Journal of the Institute of Medical Ethics, 41(7), 534–538. https://doi.org/10.1136/medethics-2014-102078
- Hamama-Raz, Y., Zabari, Y., & Buchbinder, E. (2013). From hope to despair, and back: Being the wife of a patient in a persistent vegetative state. Qualitative Health Research, 23(2), 231–240. https://doi.org/10.1177/1049732312467537
- Kitzinger, C., & Kitzinger, J. (2014). Grief, anger and despair in relatives of severely brain injured patients: Responding without pathologising. Clinical Rehabilitation, 28(7), 627–631. https://doi.org/10.1177/0269215514527844
- Larkin, M., Henwood, M., & Milne, A. (2018). Carer-related research and knowledge: Findings from a scoping review. Health & Social Care in the Community, 27(1), 55–67. https://doi.org/10.1111/hsc.12586
- Levac, D., Colquhoun, H., & O'Brien, K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5(1), 69. https://doi.org/10.1186/1748-5908-5-69
- Magnani, F. G., Leonardi, M., & Sattin, D. (2020). Caregivers of people with disorders of consciousness: Which burden predictors? Neurological Sciences, https://doi.org/10.1007/s10072-020-04394-6
- Mar, J., Arrospide, A., Begiristain, J. M., Larranaga, I., Sanz-Guinea, A., & Quemada, I. (2011). Quality of life and burden of carers of patients with acquired brain injury. Revista Espanola de Geriatria y Gerontologia, 46(4), 200–205. https://doi.org/10.1016/j.regg.2011.01.010
- Martone, M. (2000). Making health care decisions without a prognosis: Life in a brain trauma unit. The Annual of the Society of Christian Ethics, 20, 309–327. https://doi.org/10.5840/asce20002021
- McGill, P., Bradshaw, J., Smyth, G., Hurman, M., & Roy, A. (2014). Capable environments. Retrieved from https://www.kcl.ac.uk/scwru/news/2014/newsfolder/McGill-et-al-Capable-environments.pdf
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ, 339(Jul 21 1), b2535. https://doi.org/10.1136/bmj.b2535
- Moroni, L., Sguazzin, C., Filipponi, L., Bruletti, G., Callegari, S., Galante, E., Giorgi, I., Majani, G., & Bertolotti, G. (2008). Caregiver need assessment: A questionnaire for caregiver demand. Giornale Italiano di Medicina del Lavoro ed Ergonomia, 30(3 Suppl B), B84–B90. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19288782
- National Institute for Health and Care Excellence. (2014). Head injury: assessment and early management (Clinical Guideline 176). Retrieved from https://www.nice.org.uk/guidance/cg176
- Oliveira, J. d. S., Rocha, R. M., Nery, A. A., & Constancio, J. F. (2020). Repercussions of motocyclical accident in the life of workers and their families. Revista De Pesquisa-Cuidado E Fundamental Online, 12, 95–101. https://doi.org/10.9789/2175-5361.rpcfo.v12.7074
- Pelentsov, L. J., Laws, T. A., & Esterman, A. J. (2015). The supportive care needs of parents caring for a child with a rare disease: A scoping review. Disability and Health Journal, 8(4), 475–491. https://doi.org/10.1016/j.dhjo.2015.03.009
- Peters, M., Godfrey, C., McInerney, P., Munn, Z., Tricco, A., & Khalil, H. (2020). Chapter 11: Scoping reviews (2020 version). In E Aromataris, & Z Munn (Eds.), JBI manual for evidence synthesis. Joanna Briggs Institute.
- Prigerson, H., Vanderwerker, L., & Maciejewski, P. (2008). Prolonged grief disorder: A case for inclusion. In D. S. M.-V. In H, R. Stroebe M, H. Schut, & W. Stroebe (Eds.), Handbook of bereavement research and practice: 21st century perspectives (pp. 165–186). American Psychological Association Press.
- Rossi Ferrario, S., Bacchetta, M., Omarini, G., & Zotti, A. (1998). Il family Strain Questionnaire: Una proposta per il caregiving assessment. Psicologia Salute, 2(3), 119–127.
- Royal College of Physicians. (2020). Prolonged disorders of consciousness following sudden onset brain injury: National clinical guidelines. RCP.
- Sandelowski, M. (2000). Whatever happened to qualitative description? Research in Nursing and Health, 23(4), 334–340. https://doi.org/10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G
- Sica, C., Novara, C., Dorz, S., & Sanavio, E. (1997). Coping orientation to problems experienced (COPE): traduzione e adattamento italiano. Bollettino Di Psicologia Applicata, 223, 25–34.
- Soeterik, S. (2017). The experience of families and healthcare professionals supporting people with prolonged disorders of consciousness. [PhD Dissertation]. Royal Holloway, University of London. Retrieved from https://pure.royalholloway.ac.uk/portal/files/29836788/2017_Soeterik_SM_PhD.pdf
- Soeterik, S., Connolly, S., Playford, D., Duport, S., & Riazi, A. (2017). The psychological impact of prolonged disorders of consciousness on caregivers: A systematic review of quantitative studies. Clinical Rehabilitation, 31(10), 1374–1385. https://doi.org/10.1177/0269215517695372
- Soeterik, S., Connolly, S., & Riazi, A. (2018). Neither a wife nor a widow": An interpretative phenomenological analysis of the experiences of female family caregivers in disorders of consciousness. Neuropsychological Rehabilitation, 28(8), 1392–1407. https://doi.org/10.1080/09602011.2018.1529603
- Vidotto, G., Ferrario, S. R., Bond, T. G., & Zotti, A. M. (2010). Family Strain Questionnaire - Short form for nurses and general practitioners. Journal of Clinical Nursing, 19(1–2), 275–283. https://doi.org/10.1111/j.1365-2702.2009.02965.x
- Wade, D. (2018). How many patients in a prolonged disorder of consciousness might need a best interests meeting about starting or continuing gastrostomy feeding? Clinical Rehabilitation, 32(11), 1551–1564. https://doi.org/10.1177/0269215518777285
- Ware, J., Kosinski, M., & Keller, S. D. (1996). A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233. https://doi.org/10.1097/00005650-199603000-00003
- WHOQOL Group. (1998). Development of the world health organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28(3), 551–558. https://doi.org/10.1017/S0033291798006667