ABSTRACT
Sensory hypersensitivity (SHS) is a frequently heard complaint after acquired brain injury (ABI) and is related to reduced quality of life and physical and mental health. This study aimed to identify triggers for SHS after ABI and investigate how individuals cope with SHS. Nineteen adults with ABI took part in 45-min individual interviews. Data were audio-recorded and transcribed verbatim. Inductive thematic analysis revealed five themes: (1) A mismatch between resources and demands, (2) Altered experience of ordinary stimuli, (3) It affects all aspects of living, (4) Avoid, approach, accept, (5) It's highly heterogeneous. A model explaining the impact of triggers on subjective SHS after ABI is proposed, which states that SHS arises from a mismatch between the demands of a sensory environment (triggers) and the available biopsychosocial resources of an individual to meet these demands. The elicited SHS can affect and be affected by levels of fatigue, which limits the resources and creates a loop. Coping strategies can act on various stages of this model, i.e., to reduce the mismatch and potentially alter the loop. This model can contribute to the identification of mechanisms behind SHS in ABI patients and other populations, ultimately leading to evidence-based treatments.
Introduction
In order to function in our everyday lives, we need to be able to select and act upon relevant stimuli, while ignoring irrelevant and abundant input. Individuals can differ significantly in the level of sensitivity to this incoming sensory information (Brown & Dunn, Citation2002). For instance, individuals who experience sensory hypersensitivity (SHS), i.e., an over-responsiveness to sensory stimuli (Ward, Citation2019), can consequently experience a feeling of sensory overload (i.e., perceiving a stimulus as an atypical or excessive stimulation that exceeds the individual's usual level (Scheydt et al., Citation2017)). SHS can lead to feelings of being overwhelmed in stimulus-rich environments and to social isolation and, as such, is related to lower quality of life in physical, mental, emotional, and social domains (Costa-López et al., Citation2021; Shepherd et al., Citation2020).
SHS is a commonly reported complaint observed in various patient groups, including individuals with Attention Deficit Hyperactivity Disorder or Autism Spectrum Disorder, as well as in the general population (Ben-Sasson et al., Citation2019; Greven et al., Citation2019; Pfeiffer et al., Citation2015). In these cases, it is typically considered to be present, at least to some extent, from birth. However, SHS can also occur suddenly, for instance following an acquired brain injury (ABI). In this case, an individual must learn how to cope with SHS symptoms abruptly while also often struggling with other symptoms due to the ABI (e.g., physical or psychological consequences) (Jean & Deborah, Citation2007). SHS has been reported within various ABI groups, such as traumatic brain injury (TBI) or stroke, with varying reports on prevalence depending on modality, time after injury and methodology (Marzolla et al., Citation2023b; Thielen et al., Citation2022).
Our current knowledge of SHS after ABI is mostly limited to the presence and trajectory of symptoms after injury (Alwawi et al., Citation2020; Knoll et al., Citation2020; Marzolla et al., Citation2023b; Ochi et al., Citation2022). SHS symptoms are usually assessed using post-concussion symptoms questionnaires, such as the Rivermead Post-concussion Questionnaire (King et al., Citation1995), where only two items are devoted to noise and light sensitivity. A newly developed questionnaire, the Multi-Modal Evaluation of Sensory Sensitivity (MESSY) (Thielen et al., Citation2023), focuses on SHS complaints in all modalities after ABI and has been adapted to the needs of this population.
While these tools are useful to identify SHS, they do not provide information about the triggers and context of SHS symptoms, even though context by definition plays a role in SHS symptoms, as these symptoms are dependent on sensory input. Following, it is currently unclear which factors serve as triggers for SHS and to what extent these are context-dependent. Hereby, context is referring to the situation (internal and external) at the moment of the presentation of the stimulus, which can include a combination of triggers. Furthermore, the available questionnaires do not asses how individuals cope with SHS. Knowledge about triggers and coping would provide information for hypotheses about underlying mechanisms and the development of potential evidence-based interventions, which to date do not exist (note, that within the current paper, we use the term “coping” as the strategies or ways that an individual uses to “cope with” the SHS. We do not intend to make any claims about coping style as a personality trait). In order to gain this information, while abstaining from pre-emptively interpreting the concept, the use of qualitative research methods would be suitable. A qualitative description aims to depict people's experiences and understand these in their natural settings. This approach is useful for health science research as well as for clinical practitioners because it provides clear and direct information to improve clinical practice (Sandelowski, Citation2000).
Within this field, Alwawi et al. (Citation2020) investigated sensory changes (in all modalities) after stroke, using qualitative methods. Interviews with 13 stroke survivors revealed that they experienced numerous changes in their sensory processing, including being more sensitive to sensory inputs (i.e., noise, light, touch, smell, and/or taste). These changes had a substantial impact on their daily lives, and individuals reported experiencing heightened fatigue and anxiety in situations with multiple sensory stimuli at the same time. This effect of SHS on daily living and social participation has also been reported in another study including stroke patients (Carlsson et al., Citation2004). In a study that focused exclusively on noise sensitivity in the chronic stage after a traumatic brain injury, Landon et al. (Citation2012) identified four main themes. Firstly, Having to find out for myself describes the lack of knowledge available in healthcare about noise sensitivity after TBI. Participants in this study mentioned that information about their noise sensitivity at an early stage after their TBI would have considerably reduced the anxiety and stress they experienced. Hearing every footstep includes a change in sensitivity to noises compared to before the TBI. The positive and bi-directional relationships between noise, fatigue, and cognition are described in Being overwhelmed, and lastly, You have to plan depicts planning and avoidance behaviours as possible coping strategies for noise sensitivity.
In sum, we are (to some extent) aware of the presence and trajectory of SHS after ABI, and qualitative studies such as those by Landon et al. (Citation2012) and Alwawi et al. (Citation2020) have investigated the lived experience of SHS after stroke and TBI. However, information on the triggers and context in which SHS after ABI appears is still lacking. Studies have also shown that the severity of SHS complaints is not static, but can change intra-individually over time (Rabinowitz & Fisher, Citation2020; Truong et al., Citation2014). Within the current study, we aimed to accentuate the factors contributing to this variability, such as triggers and context, and propose a model for the mechanisms behind these triggers and how they can lead to symptoms of SHS. This information can be a basis for future experimental studies investigating these underlying mechanisms of SHS after ABI as well as in other clinical and non-clinical populations. Furthermore, we aimed to explore what coping strategies individuals find helpful to reduce their symptoms, as this could be directly informative for clinical practice and the development of evidence-based interventions. Therefore, the current study aimed to answer the following research questions:
What situations and factors trigger SHS after ABI?
How do individuals who experience SHS after ABI deal with their complaints?
Design
Participants
This study included 19 adults with SHS and ABI. To be included, participants had to: (a) be between 18 and 65 years old, (b) be fluent Dutch, (c) have sustained an ABI, and (d) indicate that they experience SHS, broadly defined as a heightened sensitivity to incoming sensory information across one or more sensory modalities. Participants were recruited between November 2021 and January 2022 through social media advertisements by the Dutch Brain Foundation, a non-profit organization. The Ethics Review Committee Psychology and Neuroscience of Maastricht University (NL) approved this study (ERCPN_231_149_12_2020_S1).
Data collection
After expressing interest in the study through phone or email, participants received the study information via email. If they were interested in taking part, a phone call was scheduled where the researcher (MM) explained the goal of the study and went over the inclusion criteria. Any remaining questions were answered during this phone interview and a date and time for a semi-structured interview were scheduled. The interviews were conducted either onsite in a quiet university lab room or online via video calls. If participants were interviewed on location at the university, they were picked up at the entrance by the researcher and offered something to drink. After giving them some time to settle down (both onsite and online), they were presented with an informed consent form (on paper or via an online form) and a demographics questionnaire collecting data about their age, sex, education, and diagnosis. The interview was conducted by a researcher trained for the interview protocol, which was either the first author (MSc, female) or a psychology student (female) who were trained on this project. Participants had no previous relationship with the researchers and were only aware of their relation to the current study. The interviews took approximately 45 min and participants were free to take breaks whenever necessary. The questions centred around three topics (in order): participants’ subjective experience of SHS, situations and factors that influenced or triggered this experience, and ways they dealt with SHS (The interview protocol can be found in supplementary material 1). This protocol was developed by researchers specializing in the field of ABI and SHS, and experienced with qualitative research methods. The questions were based on existing information and data about SHS, as well as on insights from clinicians who work with this patient group and its associated symptomatology. All interviews were audio recorded and transcribed verbatim, assuring the anonymity of the participants. Participants were reimbursed for their travel expenses and received a small gift as an appreciation for their participation. Initially, 22 participants signed up, where after two of them did not respond to emails or phone calls anymore and one of them cancelled the interview due to their health condition.
Data analysis
An inductive thematic analysis was conducted in ATLAS.ti 22 (Braun & Clarke, Citation2006). Two researchers (MCM and HT) coded the transcripts independently to allow for alternative interpretations. Discrepancies in interpretation were discussed in regular meetings to reach a consensus. Analysis was data-driven and a coding framework was based upon the coding of the first interview and supplemented (if needed) during the coding of every following interview. Themes were derived from the final coding framework after all interviews were coded. This was based on sorting all codes into potential themes and collating all the relevant data extracts within the identified themes, as described by Braun and Clarke (Citation2006). After reaching this initial set of themes, all data and themes were reviewed again to check that no important information was left uncategorized, and themes were adjusted accordingly. A coding example is displayed in . Quotations were selected based on the representativeness of the corresponding theme.
Table 1. Coding example in theme: It affects all aspects of living.
Results
Participant characteristics are reported in . Participants had an average age of 49.6, (SD = 10.7 years) and were mostly women (78.9%). Stroke was the most common acquired brain injury type in this group (57.9%). Most participants were in the chronic phase after ABI. Time since injury was on average 10.6 years (ranging between 2 months and 38 years). None of the participants reported having a neurodevelopmental or psychotic disorder that has been linked to SHS, such as ADHD, ASD or schizophrenia (Baum et al., Citation2015; Ghanizadeh, Citation2011; Zhou et al., Citation2020). Other diagnoses that were reported by participants are displayed in .
Table 2. Participant characteristics.
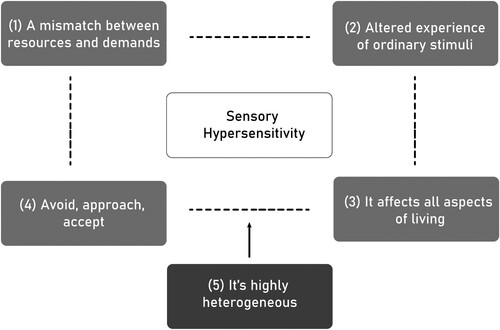
The interview data revealed a great variety in the behavioural manifestation, severity, and duration of the SHS symptoms. The negative impact of SHS on daily living was consistently reported by all participants. Participants also described feeling tired after the interview but generally, everyone expressed gratitude towards the research team for being able to tell their story and create more awareness for SHS after ABI. Overall, five main themes were identified: (1) A mismatch between resources and demands, (2) Altered experience of ordinary stimuli, (3) It affects all aspects of living, (4) Avoid, approach, accept, (5) It's highly heterogeneous (). These titles were chosen to provide a comprehensive view of the content of all themes. Simultaneously, the themes describe the chronological order of the triggers, experiences, consequences, and variety of situations of SHS.
A mismatch between resources and demands
Figure 1. Five main themes of SHS after ABI.
The first theme encapsulates what participants named as triggers for a worsening of their SHS and things that lead to a feeling of being overwhelmed. These triggers included for example internal triggers such as stress, pain, time pressure, feeling like they have to do too many things at once, and external triggers such as being presented with too many stimuli at once (e.g., taking part in traffic), uncontrolled or unexpected stimuli. These triggers were rooted in a mismatch between someone's available resources and the resources demanded by a situation. For instance, someone has a certain level of resources for an activity; however, this activity takes up more energy or cognitive resources than expected, due to different circumstances or unforeseen events. This can lead to a worsening of their SHS symptoms and consequently a feeling of sensory overload.
‘If a situation changes all of a sudden, I find it really hard to deal with that. I can feel the sensory overload building up inside of me' – Man, 58
‘It's best for me when I am just in my home and doing my own thing. When I know what my plan for the day is and no unexpected events happen’ – Woman, 42
‘Things that I cannot control, like my kids, are way worse than things I can control. Because I know by now what is good for me and what is not. So I can take this into account. However, I cannot account for external and unexpected things' – Man, 49
Changes in a situation often result in unexpected stimuli, e.g., something someone did not account for. This can be difficult to deal with spontaneously, as it requires extra energy and cognition. Hence, loss of control as well as fatigue were also identified as triggers for SHS.
‘At home people are taking my needs into account. But as soon as I go out, my villain, the noise, is there and I have no control over it’ – Woman, 51
‘Last year, one of my friends turned 30, and she gave a party at her house. I had never been before, so I was unsure of all the noise I would hear and what we were going to do and stuff. I knew that I had to find a way to be able to leave and find a quiet place, so we booked a hotel in the area’ – Woman, 37
‘I get nauseous, a flu-like feeling. My whole body gets tired because I have to constantly ‘defend’ myself against the noise and the vibrations. This does not work automatically for me anymore, and it is a downward spiral. This makes me very tired, which then makes me more sensitive’ – Woman, 54
| 2. | Altered experience of ordinary stimuli | ||||
For the current study, we provided a basic description of SHS, in order to recruit the intended participants, which referred to a heightened sensitivity to incoming sensory information across one or more sensory modalities. However, we also asked participants to share their own understanding and what SHS meant to them.
‘This can be a variety of things. It can be noise, it can be sunshine. If you for example see a row of trees with the sun shining on them, and you bike past it, you see this change between light and shadow. That can already be too much for me. It can also be an image, for example, in certain shops they have a large screen behind the counter. That can also be too much, and my legs could collapse. However, it could also be cold or warmth, or the feeling of a tag in my clothes’ – Woman, 55
‘SHS is for me that I cannot handle light, noise and other things anymore. And I get a headache, become nauseous, tired and irritated’ – Woman, 27
‘For me personally, it is that at a certain moment, it feels like everything is coming at me; the noises, lights or even something I want to read. Then I think, “I can better stop reading because I cannot take it in properly”. But yeah, it is mostly the noises and hustle around me. That's the main thing’ – Woman, 53
‘When a lot of stuff happens around me, or when there is too much noise around me, I get tired. Then I cannot think clearly anymore, and I do not know the answers any more to the easiest questions’ – Male, 61
‘Images move too quickly on the tv. Fighting scenes, racing cars, games, I can't watch any of that without regularly turning my head away’ – Woman, 42
‘I notice that there are a lot of noises. I used to like walking in the woods, however now I have to carefully move my legs so that I do not hear all the leaves. And I cannot do any of this without my noise-cancelling headphones’ – Woman, 55
‘It is also my registration of where I am in a room. For example, when I sit on a chair and someone pushes against the backrest, this feels very intense to me’ – Woman, 46
‘Also emotions of other people, I feel them way more intense’ – Woman, 46
‘For example in Amsterdam, it's really difficult for me, even if you don't see it from the outside. But you know, the trams, the people, it's so busy, and then the traffic during the day, then my SHS is an eight or nine on a scale from one to ten’ – Woman, 54
Participants reported that their SHS occurred after their brain injury, and that they experience it as a clear change compared to before their injury.
‘I used to be a teacher, and I handled 30 teenagers a day. Occasionally I was bothered by the noise, however, that was a very different feeling from how I feel now’ – Woman, 37
‘Before my injury, I did not know SHS, and afterwards, I was like: “What is this? I cannot do this. I have to go home and be in a quiet environment”’ – Woman, 51
| 3. | It affects all aspects of living | ||||
Participants reported that SHS had consequences on several aspects of their daily living, including physical, cognitive, psychological, and social effects. In the physical domain, it was reported that SHS can lead (among others) to feelings of nausea, headaches, pain, fatigue, and dizziness. Participants also reported trembling, hot flushes, and losing muscle strength during or after situations of sensory overload.
‘During my pregnancies, I was never nauseous, and now, I’m nauseous all day’ – Woman, 55
‘In a moment of high SHS (..), I get a headache. It is like pressure on my eyes, very uncomfortable. I cannot function properly anymore at a moment like that’ – Woman, 52
On a cognitive level, participants reported decreased mental flexibility, slower information processing, less attention, worsened memory, and occasionally feeling like they had lost consciousness in moments of high SHS.
Researcher: ‘How do you usually feel in those moments of heightened SHS that you described before?’ Woman, 26: ‘(…) It feels like a blockade in my head. Everything goes into it, however, I can't put into words what I want to say, and it's almost like I am trapped in my own head’
‘The biggest problem in those moments is that I can't think clearly anymore. For instance, I just cannot remember the easiest name of a friend or acquaintance. In moments where I hear a lot around me, my thinking capacity gets reduced to zero’ – Man, 61
Psychologically, feelings of anxiety, frustration, and panic were reported to be experienced in response to SHS.
Researcher: ‘How do you usually feel in those moments of heightened SHS that you described before?’ Woman, 46: ‘I just feel really bad, because there will be a lot of emotions coming out that I don’t want to have’
Researcher: ‘Do you experience physical complaints due to SHS?’ Woman, 64: (…), and I can also get annoyed or experience some level of panic’
Lastly, SHS seems to have a major effect on an individual's social life and societal roles. Participants reported being unable to continue with their job and having trouble being the partner, parent, friend, or colleague they used to be, both on an emotional and on a practical level. For instance, practically, they are unable to fulfil certain tasks they used to do in their family life, and simultaneously they need a lot more help and support from their partner than they can provide in return, due to their symptoms. Participants also mentioned the difficulties that SHS creates for their social behaviour. Other people do not seem to understand what they are going through, which can lead to feelings of helplessness and loneliness. This included family members and friends, but also healthcare workers and professionals.
‘Due to my SHS complaints, I cannot do my work anymore, because I cannot look at a screen for an extended period of time’ – Woman, 52
‘People don't see what happens afterwards. They say “but you seem fine and able to do it”, however, they don't see the costs afterward. And I also can't always explain why I feel a certain way’ – Woman, 46
| 4. | Avoid, approach, accept | ||||
When asked what participants do to deal with their SHS, answers were centred on three approaches, i.e., avoiding, approaching, or accepting their symptoms. Sometimes participants reported that a combination was found most helpful, or the best method depended on the situation (flexible coping). For avoidance, which included avoiding situations that potentially trigger SHS planning was usually the most important tool for participants to ensure this avoidance. By planning all activities carefully, a level of control could be exercised to strive for a satisfying balance between rest and effort. This was linked to the difficulties arising from a loss of control as mentioned under “A mismatch between resources and demands”. Avoidance also included the use of aids such as sunglasses and noise-cancelling headphones.
‘I try to avoid sensory overload as much as possible. I don't go to busy parties anymore, even though I like them’ – Man, 58
‘I always plan what I do, when and with whom’ – Woman, 42
‘I have to make sure I go to my bedroom, blinds down and everything dark’ – Woman, 52
Sometimes, participants reported a level of approaching their symptoms by means of training rather than avoiding them. This, for instance, included gradually exposing themselves to sensory rich situations, such as a supermarket. Participants also reported looking for a distraction rather than resting in situations of SHS, for example through exercising, crafting, or doing a little task (e.g., a game).
‘Together with my therapist, I trained to be able to go to the supermarket. We build this gradually. First, I went without needing anything, and so on. Now I am able to go there by myself’ – Woman, 52
‘I would play a game on my computer, without noise though, but just to have a bit of distraction. That is really important, so that you don't stay in your head about how bad it was. You have to be able to let it go for a while’ – Woman, 65
The third method included practicing positive thoughts and accepting the SHS as it comes rather than avoiding the situation or actively practicing exposure. Participants reported experiencing positive effects of exercising mindfulness, breathing exercises, and meditation. This also included focusing on positive things and trying to let things go and accept that things have changed.
‘I don't give up hope, improvement is possible. I’m not my previous self anymore, so I see it more as a 2.0 version’ – Woman, 46
‘I’m trying to teach myself to let things go’ – Woman, 51
| 5. | It's highly heterogeneous | ||||
During the interviews, it was observed that there is a lot of variety among participants. For instance, there were differences between participants in how they experienced SHS, its intensity, and its implications.
‘When it's really bad, it can last for 30 minutes’ – Woman, 46
‘When I reach my limit, it stays like that for days’ – Woman, 27
‘It's constantly there in the background’ – Woman, 55
Coping strategies were reported as effective by some participants, but ineffective by others (e.g., breathing exercises or resting in bed).
‘When I feel sensory overwhelmed, I don't need to sit down or sleep or anything like that. That doesn't work for me. I need to keep myself occupied, do something with my hands for example’ – Woman, 26
However, there was also variety among participants depending on the context or the encountered sensory modality. Participants found their SHS to be unpredictable, even after years of experiencing it. Some also reported noticing an improvement over time whereas others did not.
‘It's very situation-dependent. Sometimes it works if I just take a moment to myself and shut myself off from my surroundings. And other times this doesn't work at all’ – Woman, 42
‘In the beginning, after my injury, it was really bad. I could not do or handle anything. But in the last four years, I have built up a lot again’ – Woman, 46
‘I assume this will be like this for the rest of my life. I also do not see any improvements’ – Woman, 64
Even within a person, within a modality, the same stimulus would not always evoke the same response but could differ based on the triggers and context.
For example, one woman (age 26), said “Sometimes every noise is too much, it feels like a pinball machine in my head”, but also reported “When I’m driving, I turn the music really loud, so that it blocks the rest of the noise outside”.
Discussion
The current study aimed to explore the triggers that lead to sensory hypersensitivity (SHS) in individuals with ABI and to examine what strategies individuals use to cope with these symptoms. After a series of semi-structured interviews, five main themes about experiences of SHS were identified using inductive thematic analysis; (1) A mismatch between resources and demands, (2) Altered experience of ordinary stimuli, (3) It affects all aspects of living, (4) Avoid, approach, accept, and (5) It's highly heterogeneous. These themes describe the chronological process where certain triggers elicit SHS, as they create a mismatch between someone's available resources and the resources demanded by the context/sensory environment (1). This SHS is described as “an altered experience of stimuli” of various (combinations of) modalities (2), which affects physical, cognitive, psychological, and social aspects of daily living (3). Following, individuals cope with these symptoms using three approaches: “avoid, approach, and accept” (4). However, there was a great heterogeneity between and within participants in the manifestation of SHS (5).
The themes we found regarding SHS symptoms (Theme 2) and the effects it has on daily living (Theme 3) were similar to what has been described before. For instance, the hypersensitivity to a variety of stimuli after ABI was recently described by Thielen et al. (Citation2022, Citation2023) and Alwawi et al. (Citation2020). Similarly, the implications for daily living such as physical and psychological discomfort (Theme 3), as described in the current study, have also been reported for noise and light sensitivity after TBI (Callahan & Lim, Citation2018; Landon et al., Citation2012). Based on these similarities, we can assume that the current study investigates the same symptomatology as other research within this field. This provides a base for valid implications grounded in the two main aims of this study.
Firstly, we aimed to identify the triggers for SHS after ABI, as this could provide us with potential factors to target with interventions. Theme 1 (A mismatch between resources and demands) encompasses this information, and included internal triggers such as stress, pain, and time pressure, and external triggers such as multisensory environments and uncontrolled and unexpected stimuli. These triggers were reported to be related to an increased experience of SHS, suggesting SHS to be context-dependent. Following, the identified mismatch consisted of an imbalance of available resources of an individual and resources demanded by the sensory environment. The available resources seem to consist of a set of biopsychosocial factors, which can vary per individual (such as genetic, behavioural or cultural). In the current study group, the biopsychosocial resources could be affected due to the ABI (e.g., physical, cognitive, and psychological effects due to the injury, and social resources for support to deal with the other effect). However, the mismatch can also occur in the general population, when the situation is more demanding than the resources available for it, leading to feelings of SHS and being overwhelmed. This is in accordance with other studies that have shown SHS in the general population, and can also be applied to other clinical populations (Ahadi & Basharpoor, Citation2010; Ben-Sasson et al., Citation2019; Marzolla et al., Citation2023a; Pfeiffer et al., Citation2015).
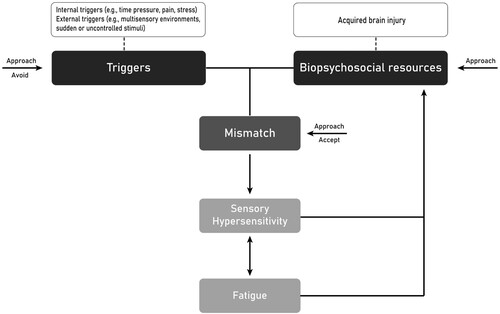
On the basis of these lived experiences of SHS, we propose a model for triggers of SHS in ABI patients (). This model is based on the statements of participants within the current study, who report having fewer resources since their injury (e.g., their mental battery feels lower or more easily exhausted than before their injury). This decrease in resources, in combination with certain triggers, can lead to the abovementioned mismatch between resources and demands, which can lead to heightened SHS in certain contexts. Experiencing SHS can further affect the available resources, creating a closed loop. Additionally, in our model, we propose a bidirectional relationship between SHS and fatigue (). Fatigue is a commonly reported symptom after acquired brain injury, which has been found to co-occur with SHS after ABI (Cantor et al., Citation2014; Chandran et al., Citation2020; Colle et al., Citation2006; Rauchman et al., Citation2023; Shepherd et al., Citation2019). The (causal) relation between fatigue and SHS in the ABI population remains unclear. However, within the current study, all participants reported fatigue before it was asked as part of the interview protocol, either as a trigger or a consequence of SHS. Participants also mentioned that rest and relaxation can help to cope with symptoms. This creates a feedback loop between SHS and fatigue, which has also been reported in other TBI patients (Landon et al., Citation2012).
Figure 2. Proposed model that describes the triggers and maintenance of SHS symptoms after ABI.
Note. The boxes containing triggers and acquired brain injury could be replaced by individualized factors such as other triggers, or circumstances that impact an individual’s biopsychosocial resources.
Next to fatigue, the level of control and predictability of stimuli plays a role in the mismatch (e.g., sudden stimuli such as unaccounted noise). During the interviews, individuals described having great difficulties with stimuli they did not account for. Exerting control has been found a key component to regaining quality of life in other studies with TBI patients (Jumisko et al., Citation2009; Landon et al., Citation2012). Besides, the preference in sensory hypersensitive individuals for predictable and controllable stimuli can be neurologically explained by existing hypotheses stating that there is less sensory neural activity when processing expected relative to unexpected information and that less certain expectations about the sensory world may lead to feelings of being overwhelmed. Within these hypotheses, it is assumed that higher neural activity in response to sensory stimuli leads to higher subjective sensory sensitivity (Ward, Citation2019). The need for control also provides a possible explanation for the inconsistencies concerning why the same stimuli sometimes lead to an unpleasant response in individuals with SHS and sometimes not (Theme 5). This suggests that SHS, in these cases, may not be instigated per se by the stimulus itself, but more by the context in which this stimulus is presented. This context can consist of the level of control over the stimulus, but also other triggers such as level of stress at the time when the stimulus is presented.
The proposed model, which functions as a closed loop, aims to explain the maintenance of SHS symptoms after ABI. This poses the question of how to break out of this, which relates to the second aim of this study, i.e., to explore how individuals who experience SHS after ABI deal with their complaints. Within Theme 4, three common strategies to cope with SHS were described; Avoid, approach, accept. Within the model, we propose that these coping strategies are ways to reduce the mismatch, to subsequently reduce SHS. For instance, avoidance could be seen as a way of eliminating some of the encountered context and its triggers, thereby reducing the chance of a mismatch. This is represented in with an arrow “Avoid” that points at “Triggers”. However, even though avoidance can sometimes be useful when protecting one's boundaries and not asking too much of oneself, it can possibly maintain the loop of SHS symptoms. The fear-avoidance model, a psychological model that states that negative appraisal of bodily sensation and its consequences can lead to fear, avoidance of related activities, and hypervigilance toward these bodily sensations (Leeuw et al., Citation2007), has been suggested to explain persistent symptoms after TBI (Wijenberg et al., Citation2017). Specifically, the relation between noise sensitivity and psychological distress may be affected by fear-avoidance behaviour in a mild TBI sample (Faulkner et al., Citation2021). This relates to the “Anxiety hypothesis” for noise sensitivity as proposed by Shepherd et al. (Citation2015). This hypothesis states that anxiety-related over-arousal leads to hypervigilance towards noise. Potentially, these concepts could be applied to SHS, where avoidance behaviours can provide temporary relief from symptoms, however over time they could play a role in the maintenance of these symptoms and the (anxiety-induced) hypervigilance towards them and towards bodily sensations in general.
The second coping style, approaching the symptoms, shows similarities with graded exposure, i.e., confrontation with the avoided or feared situation in real life, through imagination or role play (Furnham et al., Citation2013). Graded exposure to avoided stimuli and situations has been reported beneficial in individuals with ABI before (Waldron et al., Citation2013). For example, Dundon et al. (Citation2015) have also shown that selective attention deficits in TBI patients can be ameliorated by means of graded exposure to noise. The participants within the current study who reported gradually exposing themselves reported being successful by being able to manage and complete the avoided activity again (e.g., going to a supermarket), thereby increasing their levels of participation. Within the proposed model, we assume that the “approach” style could be a way of supplementing the biopsychosocial resources, or acting on the presence of triggers (via training or graded exposure). This is represented in , with arrows labelled “Approach” pointing at “Triggers” and “Biopsychosocial resources”.
Furthermore, as approach coping also included distraction from experienced symptoms, by means of e.g., exercising, it could also act directly on reducing the mismatch (, “Approach” pointing at “Mismatch”). Distraction, similar to the “acceptance” coping style, could be used to shift the hyperfocus on bodily sensations and stimuli. This resembles principles used in Acceptance and Commitment Therapy (ACT), such as improving functionality rather than focussing on symptom reduction, which have been suggested to be applicable to psychological implications following ABI (Kangas & McDonald, Citation2011). We propose that the mismatch between resources and demands contains an objective and a subjective component. The objective component is related to what is demanded in a sensory environment to function properly and respond adequately. The subjective component, however, is related to one's own expectations. Acceptance is proposed to reduce this subjective part of the mismatch, by accepting, if not embracing, the situation as it is. Therefore, this could ultimately lead to a decreased experience of SHS (, “Acceptance” pointing at “Mismatch”).
Other models for example in the ADHD literature tap into comparable elements as described in the current paper. For instance, various individual, environmental, and psychological factors are suggested to be associated with ADHD symptoms (e.g., Yadav et al., Citation2021), which share similarities with the triggers and biopsychosocial resources suggested in the current model (e.g., exposure to stress). Furthermore, the Triple-Pathway Model by Sonuga-Barke et al. (Citation2010) states that neuro-psychological heterogeneity in ADHD can be explained by dissociable cognitive, motivational, and temporal processing deficits that affect ADHD-related behaviour in some individuals, but not others. Our proposed model taps into this temporal processing aspect by including time pressure as one of the identified triggers. Cognitive and motivational domains are incorporated into the biopsychosocial resources, defined in our model. However, these studies generally do not focus specifically on symptoms of hypersensitivity. In the sensory processing literature, models suggest e.g., a role of heightened reactivity in one or more stress response systems (Biological Sensitivity to Context (Boyce & Ellis, Citation2005)), or of deeper information processing and emotional reactivity (Sensory Processing Sensitivity (Homberg et al., Citation2016)) to be underlying sensory processing sensitivity. The current model incorporates these mechanisms (biopsychosocial resources) and adds a situational/context component to it to explain momentary symptoms of SHS (triggers). Nonetheless, the question remains whether mechanisms suggested for ADHD and trait sensory processing sensitivity can be applied to an ABI population where these symptoms arose after their injury, and more research is needed to investigate the validity of the current model in other populations.
It is important to note that our study also indicated high inter-individual differences in SHS expression. As such, the triggers described here, may not be applicable for all individuals with SHS after ABI, and there may be other triggers that have not been identified yet. This high heterogeneity also implies that there might not be one solution or a one-size-fits-all treatment, but that the interplay of contributing triggers and resources should be (clinically) investigated for each individual separately.
Limitations and future research
This study contains some limitations. Firstly, the diagnosis of ABI relied solely on self-report, as we did not have access to medical documents. Besides, individuals with ABI were assessed as one group, as there was no reason to suggest differences between ABI groups at this stage, allowing us to gain an explorative and general perspective of SHS after ABI. However, future research should investigate whether injury characteristics such as injury severity, time since injury, injury location, and underlying injury mechanisms (e.g., TBI versus stroke) contribute to the development and experience of SHS, especially related to biopsychosocial resources and relevant triggers. Relatedly, a sample size of 19 participants with varying ABI conditions may limit the representativeness of the current results. Furthermore, SHS is assessed on a subjective level, as this was in accordance with the design of the study, i.e., assessing the experience of SHS. However, future studies could explore how and whether these subjective experiences could be objectified, as this might relate to underlying mechanisms and the identification of subgroups. Future studies should also evaluate the validity of the proposed model, e.g., by experimentally manipulating the triggers and measuring the SHS symptoms in response. By using interviews that required either an onsite visit or an online video call, there might be individuals with SHS who were unable to take part in this study, as this would take up too much of their energy. Therefore, the current results might not be representative of individuals on the high end of SHS after ABI. Lastly, some of the questions asked in the interview may have been too leading and not open-ended enough (e.g., providing a supermarket as an example setting for potential heightened SHS). Future research should avoid using this type of question.
Conclusion
The current qualitative study aimed to identify triggers and coping strategies for sensory hypersensitivity towards incoming sensory information after ABI. Five themes could be identified including (1) A mismatch between resources and demands, (2) Altered experience of ordinary stimuli, (3) It affects all aspects of living, (4) Avoid, approach, accept, (5) It's highly heterogeneous. Following, we proposed a model that describes the triggers and maintenance of subjective SHS after ABI, stating that SHS results from a mismatch between contexts (i.e., triggers) that demand more biopsychosocial resources from an individual than currently available. This mismatch can lead to SHS, which affects, and is affected by fatigue. Coping strategies can act on various stages of this model, aiming to reduce the mismatch and consequently the experienced SHS. Due to the heterogeneity of this group, interventions should identify and target the unique combination of triggers, context, and resources for each individual.
Triggers_coping_sensory_hypersensitivity_ABI_supplementary_1_interview_protocol.docx
Download MS Word (25.7 KB)Acknowledgements
The authors would like to thank Katrijn Schruers for her help throughout this project. Furthermore, our gratitude goes towards all participants who used their precious energy to take part in this study and support this research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Ahadi, B., & Basharpoor, S. (2010). Relationship between sensory processing sensitivity, personality dimensions and mental health. Journal of Applied Sciences, 10(7), 570–574. https://doi.org/10.3923/jas.2010.570.574
- Alwawi, D. A. A., Dean, E., Heldstab, A., Lawson, L. M., Peltzer, J., & Dunn, W. (2020). A qualitative study of stroke survivors’ experience of sensory changes. Canadian Journal of Occupational Therapy, 87(4), 298–306. https://doi.org/10.1177/0008417420941975
- Baum, S. H., Stevenson, R. A., & Wallace, M. T. (2015). Behavioral, perceptual, and neural alterations in sensory and multisensory function in autism spectrum disorder. Progress in Neurobiology, 134, 140–160. https://doi.org/10.1016/j.pneurobio.2015.09.007
- Ben-Sasson, A., Gal, E., Fluss, R., Katz-Zetler, N., & Cermak, S. A. (2019). Update of a meta-analysis of sensory symptoms in ASD: A new decade of research. Journal of Autism and Developmental Disorders, 49(12), 4974–4996. https://doi.org/10.1007/s10803-019-04180-0
- Boyce, W. T., & Ellis, B. J. (2005). Biological sensitivity to context: I. An evolutionary–developmental theory of the origins and functions of stress reactivity. Development and Psychopathology, 17(2), 271–301. https://doi.org/10.1017/S0954579405050145
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Brown, C. E., & Dunn, W. (2002). Adolescent/adult sensory profile. Pearson.
- Callahan, M. L., & Lim, M. M. (2018). Sensory sensitivity in TBI: Implications for chronic disability. Current Neurology and Neuroscience Reports, 18(9), 56. https://doi.org/10.1007/s11910-018-0867-x
- Cantor, J. B., Ashman, T., Bushnik, T., Cai, X., Farrell-Carnahan, L., Gumber, S., Hart, T., Rosenthal, J., & Dijkers, M. P. (2014). Systematic review of interventions for fatigue after traumatic brain injury: A NIDRR traumatic brain injury model systems study. The Journal of Head Trauma Rehabilitation, 29(6), 490–497. https://doi.org/10.1097/HTR.0000000000000102
- Carlsson, G., Möller, A., & Blomstrand, C. (2004). A qualitative study of the consequences of'hidden dysfunctions’ one year after a mild stroke in persons<75 years. Disability and Rehabilitation, 26(23), 1373–1380. https://doi.org/10.1080/09638280400000211
- Chandran, A., Elmi, A., Young, H., & DiPietro, L. (2020). Determinants of concussion diagnosis, symptomology, and resolution time in US high school soccer players. Research in Sports Medicine, 28(1), 42–54. https://doi.org/10.1080/15438627.2019.1590834
- Colle, F., Bonan, I., Leman, M. G., Bradai, N., & Yelnik, A. (2006). Fatigue after stroke. Annales de Réadaptation et de Médecine Physique, 49(6), 272–364. https://doi.org/10.1016/j.annrmp.2006.04.009
- Costa-López, B., Ferrer-Cascales, R., Ruiz-Robledillo, N., Albaladejo-Blázquez, N., & Baryła-Matejczuk, M. (2021). Relationship between sensory processing and quality of life: A systematic review. Journal of Clinical Medicine, 10(17), 3961. https://doi.org/10.3390/jcm10173961
- Dundon, N. M., Dockree, S. P., Buckley, V., Merriman, N., Carton, M., Clarke, S., Roche, R. A., Lalor, E. C., Robertson, I. H., & Dockree, P. M. (2015). Impaired auditory selective attention ameliorated by cognitive training with graded exposure to noise in patients with traumatic brain injury. Neuropsychologia, 75, 74–87. https://doi.org/10.1016/j.neuropsychologia.2015.05.012
- Faulkner, J. W., Snell, D. L., Shepherd, D., & Theadom, A. (2021). Turning away from sound: The role of fear avoidance in noise sensitivity following mild traumatic brain injury. Journal of Psychosomatic Research, 151, 110664. https://doi.org/10.1016/j.jpsychores.2021.110664
- Furnham, A., Wilson, E., Chapman, A., & Persuad, R. (2013). Treatment hurts: Lay theories of graded exposure in the treatment of four anxiety disorders. European Journal of Psychotherapy & Counselling, 15(3), 253–273. https://doi.org/10.1080/13642537.2013.810657
- Ghanizadeh, A. (2011). Sensory processing problems in children with ADHD, a systematic review. Psychiatry Investigation, 8(2), 89. https://doi.org/10.4306/pi.2011.8.2.89
- Greven, C. U., Lionetti, F., Booth, C., Aron, E. N., Fox, E., Schendan, H. E., Pluess, M., Bruining, H., Acevedo, B., & Bijttebier, P. (2019). Sensory processing sensitivity in the context of environmental sensitivity: A critical review and development of research agenda. Neuroscience & Biobehavioral Reviews, 98, 287–305. https://doi.org/10.1016/j.neubiorev.2019.01.009
- Homberg, J. R., Schubert, D., Asan, E., & Aron, E. N. (2016). Sensory processing sensitivity and serotonin gene variance: Insights into mechanisms shaping environmental sensitivity. Neuroscience & Biobehavioral Reviews, 71, 472–483. https://doi.org/10.1016/j.neubiorev.2016.09.029
- Jean, E., & Deborah, M. B. (2007). Acquired brain injury: An integrative neuro-rehabilitation.
- Jumisko, E., Lexell, J., & Söderberg, S. (2009). The meaning of feeling well in people with moderate or severe traumatic brain injury. Journal of Clinical Nursing, 18(16), 2273–2281. https://doi.org/10.1111/j.1365-2702.2008.02738.x
- Kangas, M., & McDonald, S. (2011). Is it time to act? The potential of acceptance and commitment therapy for psychological problems following acquired brain injury. Neuropsychological Rehabilitation, 21(2), 250–276. https://doi.org/10.1080/09602011.2010.540920
- King, N., Crawford, S., Wenden, F., Moss, N., & Wade, D. (1995). The rivermead post concussion symptoms questionnaire: A measure of symptoms commonly experienced after head injury and its reliability. Journal of Neurology, 242(9), 587–592. https://doi.org/10.1007/BF00868811
- Knoll, R. M., Lubner, R. J., Brodsky, J. R., Wong, K., Jung, D. H., Remenschneider, A. K., Herman, S. D., & Kozin, E. D. (2020). Auditory quality-of-life measures in patients with traumatic brain injury and normal pure tone audiometry. Otolaryngology–Head and Neck Surgery, 163(6), 1250–1254. https://doi.org/10.1177/0194599820933886
- Landon, J., Shepherd, D., Stuart, S., Theadom, A., & Freundlich, S. (2012). Hearing every footstep: Noise sensitivity in individuals following traumatic brain injury. Neuropsychological Rehabilitation, 22(3), 391–407. https://doi.org/10.1080/09602011.2011.652496
- Leeuw, M., Goossens, M. E. J. B., Linton, S. J., Crombez, G., Boersma, K., & Vlaeyen, J. W. S. (2007). The fear-avoidance model of musculoskeletal pain: Current state of scientific evidence. Journal of Behavioral Medicine, 30(1), 77–94. https://doi.org/10.1007/s10865-006-9085-0
- Marzolla, M. C., Hurks, P., Borghans, L., & van Heugten, C. (2023a). Hypersensitivity to noise and light: A multifactorial framework of attention, personality, and mood [Manuscript submitted for publication].
- Marzolla, M. C., Wijenberg, M., Stapert, S., Hurks, P., Schepers, J., & van Heugten, C. (2023b). Hypersensitivity to noise and light over 1 year after mild traumatic brain injury: A longitudinal study on self-reported hypersensitivity and its influence on long-term anxiety. Depression, and Quality of Life. Journal of Head Trauma Rehabilitation, 30(3), 259–267. https://doi.org/10.1097/HTR.0000000000000813
- Ochi, R., Saito, S., Hiromitsu, K., Shigemune, Y., Shinoura, N., Yamada, R., & Midorikawa, A. (2022). Sensory hypo- and hypersensitivity in patients with brain tumors. Brain Injury, 36(8), 1053–1058. https://doi.org/10.1080/02699052.2022.2110943
- Pfeiffer, B., Daly, B. P., Nicholls, E. G., & Gullo, D. F. (2015). Assessing sensory processing problems in children with and without attention deficit hyperactivity disorder. Physical & Occupational Therapy in Pediatrics, 35(1), 1–12. https://doi.org/10.3109/01942638.2014.904471
- Rabinowitz, A. R., & Fisher, A. J. (2020). Person-Specific methods for characterizing the course and temporal dynamics of concussion symptomatology: A pilot study. Scientific Reports, 10(1), 1–9. https://doi.org/10.1038/s41598-019-57220-1
- Rauchman, S. H., Zubair, A., Jacob, B., Rauchman, D., Pinkhasov, A., Placantonakis, D. G., & Reiss, A. B. (2023). Traumatic brain injury: Mechanisms, manifestations, and visual sequelae. Frontiers in Neuroscience, 17, 1090672. https://doi.org/10.3389/fnins.2023.1090672
- Sandelowski, M. (2000). Whatever happened to qualitative description? Research in Nursing & Health, 23(4), 334–340. https://doi.org/10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G
- Scheydt, S., Müller Staub, M., Frauenfelder, F., Nielsen, G. H., Behrens, J., & Needham, I. (2017). Sensory overload: A concept analysis. International Journal of Mental Health Nursing, 26(2), 110–120. https://doi.org/10.1111/inm.12303
- Shepherd, D., Heinonen-Guzejev, M., Heikkilä, K., Dirks, K. N., Hautus, M. J., Welch, D., & McBride, D. (2015). The negative affect hypothesis of noise sensitivity. International Journal of Environmental Research and Public Health, 12(5), 5284–5303. https://doi.org/10.3390/ijerph120505284
- Shepherd, D., Landon, J., Kalloor, M., Barker-Collo, S., Starkey, N., Jones, K., Ameratunga, S., & Theadom, A. (2020). The association between health-related quality of life and noise or light sensitivity in survivors of a mild traumatic brain injury. Quality of Life Research, 29(3), 665–672. https://doi.org/10.1007/s11136-019-02346-y
- Shepherd, D., Landon, J., Kalloor, M., & Theadom, A. (2019). Clinical correlates of noise sensitivity in patients with acute TBI. Brain Injury, 33(8), 1050–1058. https://doi.org/10.1080/02699052.2019.1606443
- Sonuga-Barke, E., Bitsakou, P., & Thompson, M. (2010). Beyond the dual pathway model: Evidence for the dissociation of timing, inhibitory, and delay-related impairments in attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 49(4), 345–355. https://doi.org/10.1016/j.jaac.2009.12.018
- Thielen, H., Huenges Wajer, I. M., Tuts, N., Welkenhuyzen, L., Lafosse, C., & Gillebert, C. R. (2023). The multi-modal evaluation of sensory sensitivity (MESSY): Assessing a commonly missed symptom of acquired brain injury. The Clinical Neuropsychologist, 1–35. Advance online publication. https://doi.org/10.1080/13854046.2023.2219024
- Thielen, H., Tuts, N., Welkenhuyzen, L., Huenges Wajer, I. M., Lafosse, C., & Gillebert, C. R. (2022). Sensory sensitivity after acquired brain injury: A systematic review. Journal of Neuropsychology, 17(1), 1–31. https://doi.org/10.1111/jnp.12284
- Truong, J. Q., Ciuffreda, K. J., Han, M. E., & Suchoff, I. B. (2014). Photosensitivity in mild traumatic brain injury (mTBI): a retrospective analysis. Brain Injury, 28(10), 1283–1287. https://doi.org/10.3109/02699052.2014.915989
- Waldron, B., Casserly, L. M., & O'Sullivan, C. (2013). Cognitive behavioural therapy for depression and anxiety in adults with acquired brain injury. What works for whom? Neuropsychological Rehabilitation, 23(1), 64–101. https://doi.org/10.1080/09602011.2012.724196
- Ward, J. (2019). Individual differences in sensory sensitivity: A synthesizing framework and evidence from normal variation and developmental conditions. Cognitive Neuroscience, 10(3), 139–157. https://doi.org/10.1080/17588928.2018.1557131
- Wijenberg, M. L. M., Stapert, S. Z., Verbunt, J. A., Ponsford, J. L., & Van Heugten, C. M. (2017). Does the fear avoidance model explain persistent symptoms after traumatic brain injury? Brain Injury, 31(12), 1597–1604. https://doi.org/10.1080/02699052.2017.1366551
- Yadav, S. K., Bhat, A. A., Hashem, S., Nisar, S., Kamal, M., Syed, N., Temanni, M.-R., Gupta, R. K., Kamran, S., Azeem, M. W., Srivastava, A. K., Bagga, P., Chawla, S., Reddy, R., Frenneaux, M. P., Fakhro, K., & Haris, M. (2021). Genetic variations influence brain changes in patients with attention-deficit hyperactivity disorder. Translational Psychiatry, 11(1), 349. https://doi.org/10.1038/s41398-021-01473-w
- Zhou, H.-y., Yang, H.-x., Cui, X.-l., Shi, L.-j., Gong, J.-b., Lui, S. S., Cheung, E. F., Watanabe, K., & Chan, R. C. (2020). Self-reported sensory responsiveness patterns in typically-developing and early-onset schizophrenia adolescents: Its relationship with schizotypal and autistic traits. Journal of Psychiatric Research, 131, 255–262. https://doi.org/10.1016/j.jpsychires.2020.10.002

