Abstract
Background: Low levels of physical fitness are associated with low physical and mental health. The aims of this study were to assess the health-related physical fitness of children with intellectual disability (ID), and study the association of physical activity and motor development with physical fitness.
Methods: One hundred and twenty-eight children with moderate to severe ID (83 boys; age 2–18 years) visiting specialised day programme centres engaged in field-based physical fitness tests (body composition, muscular strength, muscular endurance, and cardiorespiratory fitness). Scores were compared to reference values, and with linear regression analysis the association between the fitness outcomes and physical activity and motor development was studied.
Results: High rates of overweight (23–25%) and obesity (10–15%) were found. A majority of the participants (71–91%) scored below reference values for muscular strength, endurance, and cardiorespiratory fitness tests. Physical activity and motor development were positively associated with scores on several fitness test (β = 0.27–0.44; p < 0.05).
Conclusions: Children with moderate to severe ID visiting specialised day programme centres have strikingly low physical fitness levels. Policies and interventions to increase the physical fitness for this specific group of children are urgently needed, in which increasing physical activity and motor skills are expected to be effective components.
Strikingly low levels of physical fitness were seen in children and adolescents with moderate to severe intellectual disabilities.
This vulnerable group is in need of appropriate interventions to increase their physical fitness levels.
Increasing the physical activity is a potential component in these interventions.
Improving motor development will most likely lead to improved physical fitness as well.
Implications for rehabilitation
Introduction
Low levels of health-related physical fitness have been found in children and adolescents with intellectual disability (ID) [Citation1–5]. These low levels are alarming since children and adolescents with ID already start off with more health problems than typically developing (TD) children [Citation6] and poor physical fitness is a risk factor for cardiovascular diseases, diabetes mellitus, and poor mental health [Citation7–10]. Several longitudinal studies show that risk factors of cardiovascular diseases, like hypercholesterolemia, hypertension, and overweight transfer from childhood to adulthood [Citation11,Citation12]. Furthermore, physical fitness is important to perform activities of daily living and low levels of strength and endurance will limit independence in adulthood [Citation13,Citation14].
Such studies on physical fitness in children and adolescents with ID have mainly been conducted in children with mild to moderate ID. Children and adolescents with more severe levels of ID were usually not well-represented in those studies [Citation15], which is understandable since evaluating these children poses some challenges, like limited understanding of the task. Furthermore, persons with ID experience more musculoskeletal problems than the general population; cerebral palsy, congenital deviation of feet and hip, hypotonia, and scoliosis are more likely to occur [Citation16–18]. These conditions have an effect on the physical ability to perform tasks, but also on the potential to become physically active and fit, and develop motor skills. Other conditions like epilepsy [Citation17], respiratory problems [Citation19], and sensorimotor dysfunction [Citation20] can potentially limit these possibilities as well. In clinical practice, caregivers and parents often attribute the low levels of physical fitness, activity and motor skills to the cognitive and physical disabilities of the child or adolescent, and thereby underestimate the potential these youngsters have. Previous research has shown that improving the physical fitness, activity, and motor skills in children and adolescents with ID is possible [Citation21–25]. In the authors’ experience, current care and support focus mainly on activities of daily living skills, like getting dressed and eating independently, while there is hardly any focus on improving physical fitness.
Since more severe levels of ID are related to a higher risk of chronic health conditions, this lack of focus on physical fitness in children with more severe levels of ID is even more striking [Citation17,Citation26]. Therefore, more information is needed on the physical fitness and its correlates, in this group of vulnerable children and adolescents. This information is relevant to prioritise the focus on physical fitness, and to identify child characteristics that are associated with low levels of physical fitness, to be able to target interventions to the most vulnerable groups in this population. Characteristics of interest are sex, age, having Down syndrome (DS), level of ID, physical activity levels, and motor development.
In TD children, boys have higher scores on physical fitness tests than girls, and older children have higher scores than younger children [Citation27]. In children and adolescents with ID, these sex and age-effects are seen, but evidence is not that distinct [Citation1,Citation3,Citation28,Citation29]. Having DS and having more severe levels of ID are ID-specific child characteristics associated with low physical fitness [Citation4,Citation30,Citation31]. These above-mentioned child characteristics are non-modifiable in order to improve the physical fitness.
Children’s physical activity and motor development are parameters that can be influenced and that are positively associated with physical fitness [Citation32–36]. Previous studies have shown that children and adolescents with ID have lower physical activity levels [Citation37–40] and lower age-related motor competence [Citation41] than TD peers. However, little research has been conducted on the contribution of physical activity and motor development to physical fitness in children and adolescents with ID [Citation39]. The few studies that have been undertaken included participants with mild to moderate ID. Results on the relationship between physical fitness and activity were inconclusive: two studies found an association between moderate and/or vigorous physical activity and muscular and/or cardiorespiratory fitness [Citation42,Citation43] and one did not find a significant relationship [Citation44]. Physical fitness and motor competence were related in youth with ID in two studies [Citation45,Citation46], but again, no information is available on this relationship for children with more severe ID. Furthermore, none of these studies included physical fitness, physical activity, and motor development in the same analysis to study the complex interaction between these characteristics.
Taken together, knowledge on physical fitness levels in children with moderate to severe ID, and the relationship with physical activity and motor development, will help researchers and clinical professionals to better target interventions to increase physical fitness in this specific and vulnerable population. Moreover, more insight in the physical fitness levels and its correlates can motivate policy and decision makers to prioritise these themes in care and school settings. Therefore, the aims of this study were to assess the health-related physical fitness of children with moderate to severe ID visiting specialised day programme centres, and to study the association of physical activity and motor development with physical fitness. Low physical fitness levels in this population are hypothesised, and physical fitness is hypothesised to be associated with physical activity and motor development.
Methods
Participants
Participants were recruited for this cross-sectional study in the seven children’s day programme facilities of a service provider for people with disabilities in the Netherlands. These day programme centres are specialised to support children that are unable to go to a mainstream or special school, due to their severe developmental delay or additional medical or behavioural comorbidity.
Children were invited to participate in the study if they had an age of 2–18 years with a moderate or severe level of ID, and sufficient motor capacities to walk independently. The level of ID was evaluated by the behavioural therapist or psychologist of the child by reviewing existing testing results from the Bayley Scale of Infant and Toddler Development, Third Edition (BSID-III; [Citation47]), the Snijders-Oomen Nonverbal Intelligence Test [Citation48], or comparable tests. Children with test-results corresponding an IQ of 20–40 (severe ID) or 40–55 (moderate ID) were selected. Parents or legal representatives of children who met the inclusion criteria received an invitation letter with information about the study, and were invited to sign the informed consent form. If informed consent was provided, parents or legal representatives completed the Physical Activity Readiness Questionnaire (PAR-Q) [Citation49] to determine if the participant could participate safely in the study. If there were any concerns, the physician was consulted for advice. Children were not invited if their behavioural therapist, psychologist, physician, or nurse practitioner advised against participation in the study because of an expected negative impact on behaviour or physical health of the child. Before testing started, the participant was asked to participate in the study. In case of any verbal or non-verbal resistance before or during the testing, the procedure was stopped immediately. This is according the Dutch code of conduct for “minors” and “mentally disabled” [Citation50,Citation51].
Ethical approval was obtained (MEC-2013-491) from the Ethics Committee of the Erasmus Medical Center. The study adheres to the Declaration of Helsinki for research involving human subjects [Citation52].
Measurements
Physical fitness tests
This study focused on the health-related physical fitness components according to the subdivision of the American College of Sports Medicine (ACSM) [Citation53]: body composition, muscular strength, muscular endurance, and cardiorespiratory fitness. Flexibility is another component, however, the relationship between flexibility and health has not been confirmed in children [Citation54,Citation55] and, therefore, this component was not included in this study.
Appropriate tests for children with a moderate to severe ID were selected based on three steps. In short, first a literature review on the known psychometric properties of field-based physical fitness tests in children with ID was performed [Citation15]. Second, the tests included in the review with proper psychometric properties were discussed with a focus group of physical therapists. The physical therapists discussed the feasibility of the tests (functionality, cognitive, and motor demands), and face validity. Based on the outcome of the discussion, one or more suitable test per physical fitness component was selected for the pilot study. The pilot study was step three, in which selected tests were studied on feasibility and reliability. This was done in a sample of 39 children with moderate to severe ID, age 2–18 years [Citation56]. Short-term (during one session) and long-term (2–4 weeks in between) test–retest reliability were studied. Tests with sufficient reliability (intraclass correlation > 0.7) were selected for this study: body mass index (BMI), waist circumference, overarm throwing, stair climbing, and modified 6-min walk test (6MWT).
Body composition
BMI was calculated as body weight in kg divided by height in meters squared. BMI-for-age-Z scores (zBMI) were calculated according to the WHO Growth references [Citation57,Citation58]. Based on these Z-scores, weight status was determined. Participants were classified as underweight when zBMI was < 2 SD. Participants at age 0–5 years with BMI > 2 SD were classified as overweight, > 3 SD as obese. For older children (6–18 years), >1 SD was classified as overweight and >2 SD as obese [Citation59]. High test–retest reliability results for BMI were found in children with moderate to severe ID (ICC > 0.99) [Citation56].
Waist circumference provides a measure of abdominal adiposity [Citation60]. It was measured halfway between the iliac crest and tenth rib, directly on the skin, using a flexible measuring tape accurate at the 0.1 cm level (Seca 201, Hamburg, Germany). High test–retest reliability results were found in this population (ICC > 0.99) [Citation56]. The waist circumferences values were compared to age and sex-matched Dutch reference values, in which the +1.3 SD was used as cut-off for overweight, and +2.3 SD was used as cut-off for obesity [Citation61].
Muscular strength
The muscular strength test was selected from the Functional Strength Measurements (FSM), developed for TD children of 4–10 years old [Citation62]. Only one muscular strength test of the FSM, the overarm throwing task, had sufficient test–retest reliability in children with moderate to severe ID (ICC = 0.76) [Citation56] and was selected for this study. In children with mild ID, the overarm throwing test had moderate convergent validity with handheld dynamometry [Citation63]. In this test, the participant stands behind a line and raises a bag of 2, 3, or 4 kg (dependent on the age) behind the head and throws the bag as far as possible. The distance from the line to the distal side of the bag is measured in cm. The actual test consists of three attempts, and the final score is the best score of these three attempts. Some participants needed extra guidance to perform this task correctly. In these cases, the test instructors physically or verbally guided the participants to starting position behind the line, and handed over the bag above their heads.
The muscular strength outcomes were compared to the reference values of 616 Dutch TD children, available for age 4–10 years [Citation64]. The 5th and 95th percentile were used as cut-off values.
Muscular endurance
For this component another test of the FSM [Citation62] was used: the stair climbing test. The participant walks the stairs as fast as possible up and down (three steps up and three down), turns and repeats this as many times as possible in 30 s. The amount of steps in 30 s is the score. The test consists of three attempts, and the final score is the best score of these three attempts. If the participant had difficulties with turning, the test instructor softly guided the turn.
In children with mild ID, the stair climbing test had moderate convergent validity with handheld dynamometry [Citation63]. A pilot study indicated good test–retest reliability in children with moderate to severe ID (ICC = 0.92) [Citation56]. However, it also indicated a significant improvement between the test and re-test; therefore, the children performed the test twice. The best score of the two trials was the final score. The muscular endurance outcomes were compared to the reference values of 616 Dutch TD children of 4–10 years [Citation64]. The 5th and 95th percentile were used as cut-off values.
Cardiorespiratory fitness
The 6MWT is a test of functional capacity, and is recommended by the ACSM to use as field-based test for cardiorespiratory fitness in several populations with low fitness levels [Citation53]. The 6MWT was found to be a valid and reliable test in adolescents with overweight or obesity and mild-to-moderate ID [Citation65]. The test was modified to make it more feasible for children with moderate to severe ID [Citation56]. During the modified 6MWT the participants walk as many meters as possible in 6 min over a 20-m track, holding a loose hand of the instructor. The heart rate was continuously monitored (Polar RS400, Polar Electro Oy, Kempele, Finland). Peak heart rate was calculated afterwards. The modified 6MWT outcomes were compared to the reference values of 328 TD British children, age 4–11 years. Tenth and 90th percentiles were used as cut-off values [Citation66]. The scores were also compared to an equation which predicts normal scores [Citation67]: distance = 11.89 × age (year) + 486.1. This equation was based on 496 Swiss children age 5–16 years.
Physical activity
Participants were asked to wear of triaxial accelerometers (Actigraph GT3x+) on the right hip, for eight consecutive days. Physical activity was expressed by steps per day. Data ware sampled with a frequency of 30 Hz, and data was derived with 15 s epochs [Citation68,Citation69]. Non-wear time was defined as ≥20 min of consecutive zeros, with no allowance of epochs with counts above zero [Citation70]. Non-wear time was excluded from analysis. Data with at least 4 d of recording with a daily minimum of eight registered hours were included in the analysis [Citation71]. In this selection procedure, no distinction was made between week days or weekend days, as no significant differences were found between the physical activity on week days or weekend days (data not shown).
Motor development
The gross motor subscale of the BSID-III [Citation47] was completed by physical therapists to give insight into the gross motor development of the participants. The BSID is designed to measure the developmental status of young children up to 42 months, but it can also be used to assess the development of individuals with severe delays, such as children and adolescents with ID [Citation72]. Based on clinical experience with children and adolescents with moderate to severe ID and with motor testing, and the experience of consulted physical therapist in the field, the BSID-III was chosen. A score of 42–43 on the gross motor scale corresponds to the motor development of a TD child aged 12 months, a score of 57–24 months, 64 points to 36 months, and the maximum score (67–72 points) to 42 months [Citation47].
Adaptive behaviour
The relative age corresponding the adaptive behaviour was used as a continuous indicator of the level of ID, since ID is a disability characterised by significant limitations both in intellectual functioning and in adaptive behaviour [Citation73]. Adaptive behaviour was assessed by the Dutch version of the Vineland Adaptive Behavioral Scale [Citation74,Citation75]. In this scale, three types of skills are covered: conceptual, social, and practical skills. The scale was filled in by the caregiver of the child and scored and converted to relative age score by the concerned behavioural therapist or physiologist.
Other child characteristics
Information on autism spectrum disorder and challenging behaviour was provided by the behavioural therapist or psychologist of the participants. Information on age and DS was extracted from the medical file, information for socioeconomic status, and origin (Dutch or non-Dutch) was provided by the parents. Socioeconomic status was based on the highest education of the parents: primary and secondary school, and lower or intermediate vocational school were classified as “low socioeconomic status, higher vocational school or university were classified as high socioeconomic status”. Children were considered as having a non-Dutch origin when at least one of their parents was born outside the Netherlands [Citation76].
Procedure
The physical fitness tests were performed in a gymnasium at each of the seven-day programme facilities during daytime, by one participant at a time. The tests were performed in a fixed order within the test session: body composition, modified 6MWT, stair climbing (1st trial), overarm throwing, and stair climbing (2nd trial). In this sequence, the load on, respectively, the upper and lower extremities were taken into account and familiarisation with the tester and the test environment by starting with relatively easy tests as body composition and the modified 6MWT. Resting between tests was allowed. The instructors explained the tests and demonstrated how to perform it correctly. For the more difficult muscular strength and muscular endurance tests, the participants could practice up to five times. When they performed it correctly during this practice phase, the actual test started. During all tests, the instructor encouraged the participants to perform maximally. No standardised encouragement was used since every child had their own preferences and communication style. The test instructors judged if the participant understood the instruction performed the test with maximal effort, and according to protocol. When the performance was not meeting these requirements, the reason of drop-out was noted and no score was written down. The gross motor scale of the BSID-III was performed at another occasion, within a month of the fitness testing. All instructors (physical therapist or human movement scientist) had many years of experience with testing procedures and working with children with moderate to severe ID.
Analysis
Descriptive statistics were used to describe the participant characteristics. Group differences between the total group and group per test were determined using Pearson’s Chi-square tests for dichotomous data, and independent t-tests for interval or ratio data, to investigate selective drop out.
The outcome on the several physical fitness tests were displayed by use of descriptive statistics. In order to compare the outcomes to the reference values, scatter plots were made, with the reference values plotted in the graphs. The percentages of participants that scored worse than the given age-related reference values were calculated. For the participants that fell outside the reference values due to their age, the reference value of the nearest age group was used.
To investigate the association of physical activity and motor development with the physical fitness scores, multiple linear regression analyses were performed. Each physical fitness test was a dependent variable. The following independent variables were entered in one block: sex, age, adaptive behaviour (as continuous indicator of level of ID), the BSID score (motor development), and steps per day (physical activity). Because of the small number of participants with both valid accelerometer data and a score on either the overarm throwing or stair climbing test, steps per day was not entered in the regression analysis for these two fitness tests. Assumptions of multicollinearity and homoscedasticity were checked before conducting the analysis [Citation77].
The data were analysed by use of SPSS version 24 (IBM statistics, Armonk, NY), Actilife 6 (Actigraph) and Excel (Microsoft 2016), and alpha level was set at 5%.
Results
Participants
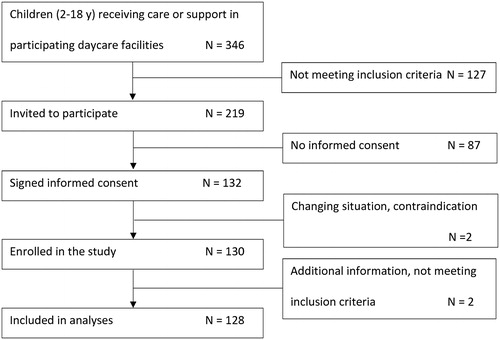
After inviting 219 children and adolescents to participate in the study, a total of 128 children with a moderate or severe ID were included. The flow diagram of the inclusion process can be found in .
In , the characteristics of the participants are described. The total sample consisted of 83 boys and 45 girls, with an average age of 9.6 ± 4.1 years (range 2–18). More than half of the participants had a severe ID (n = 73, 57%), with an average adaptive behaviour corresponding to the age of 1.4 ± 0.4 years. The children with a moderate ID (n = 54, 43%) had an adaptive behaviour corresponding to 2.7 ± 1.9 years. In total, 44 children had been diagnosed with autism spectrum disorder, 30 with DS. The included children were significantly younger than the non-included children (9.6 ± 4.1 vs. 10.5 ± 3.7 years; t(217) = 2.221; p = 0.03), but no difference between groups was found with regard to sex (χ2(1) = 0.056; p = 0.81).
Table 1. Participants’ characteristics for the total group.
The included children performed at least one physical fitness test according to protocol, 46 participants had scores on all five fitness tests. The main reasons for drop out were challenging behaviour, cognitive issues, and motor development issues. This was comparable to the drop out that was encountered in the pilot study [Citation56]. Sample size per test ranged from 59 for overarm throwing to 118 for BMI (). Because of the variable sample size per test, participant characteristics differed per test. However, only for overarm throwing and stair climbing significant differences compared to the total sample were found; the children that correctly performed the overarm throwing test consisted of relatively more children with moderate ID (64%; χ2(1) = 7.7; p < 0.01), had more developed adaptive behaviour (2.6 ± 1.8 years; t(156) = −2.67; p = 0.01) and a better motor development (63.6 ± 5.9; t(167) = −3.51; p < 0.01). For stair climbing, the children also had better motor development than the total group (63.6 ± 5.5; t(175) = −3.38; p < 0.01). The participants’ characteristics per test can be found in the Supplementary Table S1.
Table 2. Average score on the physical fitness tests and percentage participants scoring worse than reference values.
Sixty-eight participants had enough valid accelerometer data to be included in the analysis. For the other participants, data transfer problems occurred (n = 15), not enough valid data was on the accelerometer (n = 31), or the accelerometer got lost (n = 1). For 58 of the 68 children, at least one weekend day was included. Characteristics of the participants with physical activity data were not significantly different from those of the non-participants [Citation78].
Physical fitness levels
For body composition, BMI and waist circumference was correctly assessed in, respectively, 118 and 116 children. Average BMI was 19.3 ± 4.4 kg/m2, average zBMI 0.82 ± 1.21 (). Based on these zBMI scores, 3% of the children were classified as having underweight, 25% as having overweight, and 15% as having obesity (). The average waist circumference was 65.4 ± 15.1 cm (). Twenty-seven children (23%) were labelled as overweight, and 12 children (10%) were labelled as obese. Graphs of the scores compared to the reference values can be found in .
Figure 2. Scatterplots of the individual scores on the physical fitness test, with reference values plotted in the graphs. A. zBMI. B. Waist circumference – males. C. Waist circumference – females. D. Overarm throwing. E. Stair climbing. F. Modified 6MWT.
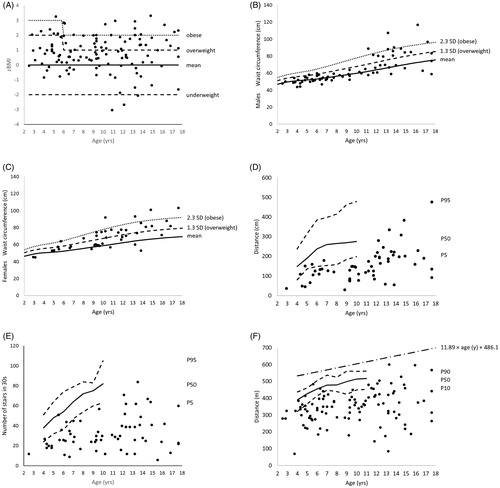
The muscular strength test was performed by 59 participants according to protocol. Average throwing distance was 155 ± 84 cm (, ). Compared to the reference values, 42 participants (71%) scored below the P5 cut-off values.
The muscular endurance test was correctly completed by 63 participants. Their maximum score of the two trials on the stair climbing test was on average 32 ± 17 steps in 30 s (). The majority of the participants achieved the maximum score in the second trial (n = 39, 62%), 13% (n = 8) in first trial, and 25% (n = 16) had the same score in both trials. Compared to the reference values, 57 participants (91%) scored below the P5 cut-off values.
The modified 6MWT, as indicator of cardiorespiratory fitness, was correctly performed by 102 children. They walked an average distance of 349 ± 98 m in 6 min (), with an average HRpeak of 142 ± 17 beats·min−1 (n = 79). Compared to the reference values of Lammers et al. [Citation66], 77 participants (75%) scored below the P10 cut-off values. None of the children made enough distance to reach the predicted distance by Ulrich et al. [Citation67].
In the Supplementary Table S2, separated scores for boys and girls on the physical fitness tests can be found.
Associations with physical fitness
Motor development was positively associated with overarm throwing (β = 0.27, p = 0.02), stair climbing (β = 0.44, p < 0.001), and the modified 6MWT (β = 0.34, p = 0.02). Increasing number of steps per day was only associated with an increasing score on the modified 6MWT (β = 0.33, p < 0.01) ().
Table 3. Association of fitness outcomes and predictor variables assessed by a multiple linear regression analysis.
Discussion
This study indicates that children with moderate to severe ID visiting specialised day programme centres have very low levels of health-related physical fitness. The relationship of the modifiable factors physical activity and motor development with cardiorespiratory fitness and muscular strength and endurance indicate a potential way to improve physical fitness in this population.
The current findings of low physical fitness levels in this specific group of children compared to TD children are similar to previous findings in children and adolescents with less severe levels of ID. For example, Dutch children aged 8–11 years with borderline to mild ID scored significantly lower on the handgrip, standing broad jump, sit-ups and 20 m shuttle run tests compared to TD peers [Citation1]. Comparable results were seen for adolescents with mild to moderate ID [Citation3], adolescents with DS [Citation2], and children with borderline to mild ID [Citation4]. High overweight rates were seen before as well [Citation3,Citation5]. The current rates of overweight and obesity are much higher than those of TD Dutch children: 40 vs. 13–15% [Citation79].
A positive association was found between physical activity and cardiorespiratory fitness, suggesting that cardiorespiratory fitness of youth with moderate to severe ID might be improved with increasing the amount of physical activity. These results are in agreement with intervention studies in youth with ID and TD youth which indicated positive effects of physical activity, like exercise, on several physical fitness outcomes [Citation23,Citation80–84].
The current results show an association between physical fitness and motor development, for the components muscular strength, muscular endurance, and cardiorespiratory fitness. This is in agreement with the findings in TD children that high levels of motor skills are related to high levels of physical fitness [Citation85–87]. The current results are comparable to two Asian studies in samples of over 400 children and adolescents with mild to moderate ID [Citation45,Citation46]. Both studies found statistically significant correlations between motor skills and muscular strength, muscular endurance, and CR fitness (r = 0.19–0.52; p < 0.05).
In this study, body composition was not related to physical activity and motor development. This is in line with previous studies in youth with ID [Citation42,Citation43,Citation45,Citation46,Citation88]. However, in TD children, an association between body composition and physical activity and motor development is seen [Citation89–91]. This difference could be explained by the body composition measures used. The studies in TD children used body fat measures, like skinfold thickness [Citation89–91]. In the studies with participants with ID BMI and waist circumference was measured which are anthropometric measures that are surrogate measures of body fatness. These measures cannot discriminate between fat mass and fat-free mass. Another explanation could be the study population. In youth with ID, other factors might be more strongly related to body composition. Factors associated with overweight and obesity in people with ID are nutritional habits, psychotropic medication, and altered metabolic rate [Citation92]. However, physical activity interventions did result in weight loss in children and adolescents with ID [Citation93,Citation94], which suggest that a relationship between physical activity and body composition does exist.
The physical fitness tests used in this study were tested on feasibility and reliability in a pilot study of 37 participants [Citation56]. Even though high drop-out rates were seen for the muscular strength and endurance tests both in this study and in the pilot study, the test–retest reliability was sufficient for group analysis (ICC > 0.75). Further research is required to find appropriate tests for the children and adolescents with moderate to severe ID, who were not able to perform the selected tests. Especially the children with a more severe level of ID, and children with less motor abilities, were less able the perform the muscular strength and muscular endurance tests. For these components more research is needed on tests which demand little cognitive and motor competence.
Implications
Even though children and adolescents with ID have to deal with musculoskeletal problems and other physical challenges [Citation16–18], improvements in physical fitness, physical activity, and motor skills are possible [Citation21,Citation22,Citation95–101]. For example, motor skill training sessions of 10–15 min, 3–5 times a week, can results in significant improvements in motor functioning in persons with severe to profound ID [Citation22].
In the Netherlands, the specialised day programme centres are not obligated to organise physical education, in contrast to regular primary schools. The children and adolescents with ID are physically active during day activities, but do not have physical education sessions supervised by skilled professionals. Considering the low physical fitness levels, associated with physical activity and motor development, found in this study, and the vulnerable population, the government and care organisations should make regular physical education supervised by skilled professionals a central standard for specialised day programme centres.
Limitations
The group participants consisted of 128 children and adolescents with moderate to severe ID. However, the sample size per test ranged from 59 to 118 children. Drop-out in the different tests has caused a bias in the muscular strength and muscular endurance tests, in which children with lower adaptive behaviour and less motor development were less likely to perform the tests correctly.
For physical activity steps per day was chosen as outcome measure. This measure reflects mainly the vertical axis activity, and can, therefore, be seen as participants’ walking behaviour. This measure was chosen because walking is likely to be the primary activity persons with ID engage in [Citation102,Citation103]. However, choosing one outcome measure for physical activity is a limitation of the study. Steps per day give no information on the amount of minutes and intensity of physical activity in which the participants engaged in.
The BSID test was used to indicate motor development was originally developed for TD children up to 42 months. Potentially, this could have caused a ceiling effect, since the participants in this study were between the 2 and 18 years old. However, the scores were evenly distributed (range 42–72 points), with only one participant reaching the maximum score (data not shown).
Due to the small sample sizes per test, this study was only powered to control for a few child characteristics in the linear regression analysis. The variables that were controlled for were sex, age, and adaptive behaviour (as indicator of level of ID). This was based on previous studies in TD children and children with ID [Citation1,Citation30]. Preferably, future studies with larger sample size should control for DS, social economic status, and origin as well, since previous research has shown that these variables were also associated with physical fitness [Citation104–106]. With regards to the influence of DS, previous research has shown that persons with DS have lower physical fitness values than persons with other causes of ID [Citation31]. Certain characteristics or comorbidities of DS can explain these differences. One of the explanations of these low fitness values is the altered autonomic function [Citation107]. Since 23% of the current sample had DS, this might have negatively influenced the outcomes. However, univariate analyses indicated that the participants with DS did not score significantly lower than the participants with other causes of ID (data not shown).
The reference values that were used had limitation as well. Only for body composition, standardised values for age were calculated. For the other fitness components, only norm-referenced cut-off scores per age were available, and only for a small age-bandwidth. To compare the scores of the participants that fell outside the bandwidth, the reference values of nearest age group were used, but these reference values most likely underestimate the actual 95th percentile. Moreover, it is likely that a sex difference will appear during puberty on these components [108] and the reference values that were used, were not sex-specific.
Due to the cross-sectional design of the study, no comment can be made on the direction of the relationship between physical fitness, physical activity, and motor development. In the general population, these relationships are suggested to be bidirectional and dynamic [Citation85].
Conclusions
Children with moderate to severe ID visiting specialised day programme centres have high rates of overweight and obesity, and low levels of muscular strength, muscular endurance, and cardiorespiratory fitness. Policies and interventions to increase the physical fitness for this specific group of children are urgently needed, in which increasing motor skills and physical activity should have a central place.
Supplemental Materials
Download PDF (211.7 KB)Acknowledgements
We would like to thank the children, adolescents and their parents and professional caregivers for participating in this study. Furthermore, we would like to thank the physical therapists of Reinaerde for helping with the data collection.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Hartman E, Smith J, Westendorp M, et al. Development of physical fitness in children with intellectual disabilities. J Intellect Disabil Res. 2015;59:439–449.
- Izquierdo-Gomez R, Martinez-Gomez D, Tejero-Gonzalez CM, et al. Are poor physical fitness and obesity two features of the adolescent with Down syndrome? Nutr Hosp. 2013;28:1348–1351.
- Salaun L, Berthouze-Aranda SE. Physical fitness and fatness in adolescents with intellectual disabilities. J Appl Res Intellect Disabil. 2012;25:231–239.
- Golubovic S, Maksimovic J, Golubovic B, et al. Effects of exercise on physical fitness in children with intellectual disability. Res Dev Disabil. 2012;33:608–614.
- Slevin E, Truesdale-Kennedy M, McConkey R, et al. Obesity and overweight in intellectual and non-intellectually disabled children. J Intellect Disabil Res. 2014;58:211–220.
- Oeseburg B, Dijkstra GJ, Groothoff JW, et al. Prevalence of chronic health conditions in children with intellectual disability: a systematic literature review. Intellect Dev Disabil. 2011;49:59–85.
- Ortega FB, Ruiz JR, Castillo MJ, et al. Physical fitness in childhood and adolescence: a powerful marker of health. Int J Obes. 2008;32:1–11.
- Hurtig-Wennlof A, Ruiz JR, Harro M, et al. Cardiorespiratory fitness relates more strongly than physical activity to cardiovascular disease risk factors in healthy children and adolescents: the European youth heart study. Eur J Cardiovasc Prevent Rehabil. 2007;14:575–581.
- Ortega FB, Tresaco B, Ruiz JR, et al. Cardiorespiratory fitness and sedentary activities are associated with adiposity in adolescents. Obesity (Silver Spring). 2007;15:1589–1599.
- Anderssen SA, Cooper AR, Riddoch C, et al. Low cardiorespiratory fitness is a strong predictor for clustering of cardiovascular disease risk factors in children independent of country, age and sex. Eur J Cardiovasc Prevent Rehabil. 2007;14:526–531.
- Raitakari OT, Juonala M, Kahonen M, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the cardiovascular risk in young Finns study. JAMA. 2003;290:2277–2283.
- Andersen LB, Hasselstrom H, Gronfeldt V, et al. The relationship between physical fitness and clustered risk, and tracking of clustered risk from adolescence to young adulthood: eight years follow-up in the Danish youth and sport study. Int J Behav Nutr Phys Act. 2004;1:6.
- Hilgenkamp TIM, van Wijck R, Evenhuis HM. (Instrumental) activities of daily living in older adults with intellectual disabilities. Res Dev Disabil. 2011;32:1977–1987.
- Oppewal A, Hilgenkamp TIM, van Wijck R, et al. Physical fitness is predictive for a decline in daily functioning in older adults with intellectual disabilities: results of the HA-ID study. Res Dev Disabil. 2014;35:2299–2315.
- Wouters M, Evenhuis HM, Hilgenkamp TIM. Systematic review of field-based physical fitness tests for children and adolescents with intellectual disabilities. Res Dev Disabil. 2017;61:77–94.
- Vonken MTH, Maaskant MA, van den Akker M. Prevalentie en risicogroepen voor aandoeningen van het bewegingsapparaat bij mensen met een verstandelijke beperking. NTZ. 2006;2:98–110.
- Schrojenstein Lantman-de Valk HMJ, Akker M, Maaskant MA, et al. Prevalence and incidence of health problems in people with intellectual disability. J Intellect Disabil Res. 2007;41(Pt 1):42–51.
- Bilo RAC, Voorhoeve HWA. Kind in ontwikkeling. Een handreiking bij de observatie van jonge kinderen. 7th ed. Houten, Netherlands: Bohn Stafleu van Loghum; 2007.
- Seddon PC, Khan Y. Respiratory problems in children with neurological impairment. Arch Dis Childhood. 2003;88:75–78.
- Wuang YP, Wang CC, Huang MH, et al. Profiles and cognitive predictors of motor functions among early school-age children with mild intellectual disabilities. J Intellect Disabil Res. 2008;52:1048–1060.
- Hocking J, McNeil J, Campbell J. Physical therapy interventions for gross motor skills in people with an intellectual disability aged 6 years and over: a systematic review. Int J Evid Based Healthc. 2016;14:166–174.
- Houwen S, van der Putten A, Vlaskamp C. A systematic review of the effects of motor interventions to improve motor, cognitive, and/or social functioning in people with severe or profound intellectual disabilities. Res Dev Disabil. 2014;35:2093–2116.
- Dodd KJ, Shields N. A systematic review of the outcomes of cardiovascular exercise programs for people with Down syndrome. Arch Phys Med Rehabil. 2005;86:2051–2058.
- Frey GC, Temple VA, Stanish HI. Interventions to promote physical activity for youth with intellectual disabilities. Salud Publica Mex. 2017;59:437–445.
- Shin IS, Park EY. Meta-analysis of the effect of exercise programs for individuals with intellectual disabilities. Res Dev Disabil. 2012;33:1937–1947.
- Moss S, Goldberg D, Patel P, et al. Physical morbidity in older people with moderate, severe and profound mental handicap, and its relation to psychiatric morbidity. Soc Psychiatry Psychiatr Epidemiol. 1993;28:32–39.
- Welk GJ, De Saint-Maurice Maduro PF, Laurson KR, et al. Field evaluation of the new FITNESSGRAM(R) criterion-referenced standards. Am J Prevent Med. 2011;41:S131–S142.
- Lin JD, Yen CF, Li CW, et al. Patterns of obesity among children and adolescents with intellectual disabilities in Taiwan. J Appl Res Int Dis. 2005;18:123–129.
- Mercer VS, Lewis CL. Hip abductor and knee extensor muscle strength of children with and without Down syndrome. Pediatr Phys Ther. 2001;13:18–26.
- Skowronski W, Horvat M, Nocera J, et al. Eurofit special: European fitness battery score variation among individuals with intellectual disabilities. Adapt Phys Activ Q. 2009;26:54–67.
- Pitetti KH, Baynard T, Agiovlasitis S. Children and adolescents with Down syndrome, physical fitness and physical activity. J Sport Health Sci. 2013;2:47–57.
- Malina RM. Physical activity and fitness: pathways from childhood to adulthood. Am J Hum Biol. 2001;13:162–172.
- Hands B, Larkin D, Parker H, et al. The relationship among physical activity, motor competence and health-related fitness in 14-year-old adolescents. Scand J Med Sci Sports. 2009;19:655–663.
- Kristensen PL, Moeller NC, Korsholm L, et al. The association between aerobic fitness and physical activity in children and adolescents: the European youth heart study. Eur J Appl Physiol. 2010;110:267–275.
- Burgi F, Meyer U, Granacher U, et al. Relationship of physical activity with motor skills, aerobic fitness and body fat in preschool children: a cross-sectional and longitudinal study (Ballabeina). Int J Obes. 2011;35:937–944.
- Cattuzzo MT, Dos Santos Henrique R, Re AH, et al. Motor competence and health related physical fitness in youth: a systematic review. J Sci Med Sport. 2016;19:123–129.
- Einarsson IT, Johannsson E, Daly D, et al. Physical activity during school and after school among youth with and without intellectual disability. Res Dev Disabil. 2016;56:60–70.
- Einarsson IT, Olafsson A, Hinriksdottir G, et al. Differences in physical activity among youth with and without intellectual disability. Med Sci Sports Exerc. 2015;47:411–418.
- Frey GC, Stanish HI, Temple VA. Physical activity of youth with intellectual disability: review and research agenda. Adapt Phys Activ Q. 2008;25:95–117.
- Hinckson EA, Curtis A. Measuring physical activity in children and youth living with intellectual disabilities: a systematic review. Res Dev Disabil. 2013;34:72–86.
- Hartman E, Houwen S, Scherder E, et al. On the relationship between motor performance and executive functioning in children with intellectual disabilities. J Intellect Disabil Res. 2010;54:468–477.
- Izquierdo-Gomez R, Martinez-Gomez D, Villagra A, et al. Associations of physical activity with fatness and fitness in adolescents with Down syndrome: the UP&DOWN study. Res Dev Disabil. 2015;36:428–436.
- Matute-Llorente A, Gonzalez-Aguero A, Gomez-Cabello A, et al. Physical activity and cardiorespiratory fitness in adolescents with Down syndrome. Nutr Hosp. 2013;28:1151–1155.
- Shields N, Hussey J, Murphy J, et al. An exploratory study of the association between physical activity, cardiovascular fitness and body size in children with Down syndrome. Dev Neurorehabil. 2017;20:92–98.
- Frey GC, Chow B. Relationship between BMI, physical fitness, and motor skills in youth with mild intellectual disabilities. Int J Obes. 2006;30:861–867.
- Foley JT, Harvey S, Chun HJ, et al. The relationships among fundamental motor skills, health-related physical fitness, and body fatness in South Korean adolescents with mental retardation. Res Q Exerc Sport. 2008;79:149–157.
- Bayley NB. Scales of infant and toddler development. 3rd ed. San Antonio (TX): Pearson Education, Inc; 2006.
- Tellegen PJ, Winkel M, Wijnberg-Williams BJ, et al. Snijders-oomen nonverbal intelligence test, SON -R 2½-7, manual & research report. Lisse, the Netherlands: Swets & Zeitlinger; 1998.
- Thomas S, Reading J, Shephard RJ. Revision of the physical activity readiness questionnaire (PAR-Q). Can J Sport Sci. 1992;17:338–345.
- CCMO. Code of conduct mentally disabled. 2002 [cited 2018 Oct 1]. Available from: http://www.ccmo.nl/attachments/files/code-of-conduct-mental-disabled.pdf
- CCMO. Code of conduct minors. 2002 [cited 2018 Oct 1]. Available from: http://www.ccmo.nl/attachments/files/code-of-conduct-minors.pdf
- World Medical Association. Declaration of Helsinki - ethical principles for medical research involving human subjects Helsinki. 2013. [cited 2018 Dec 12]. Available from: https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/doh-oct2013-jama-2/
- American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 10th ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2017.
- Ganley KJ, Paterno MV, Miles C, et al. Health-related fitness in children and adolescents. Pediatr Phys Ther. 2011;23:208–220.
- Ruiz JR, Castro-Pinero J, Artero EG, et al. Predictive validity of health-related fitness in youth: a systematic review. Br J Sports Med. 2009;43:909–923.
- Wouters M, van der Zanden AM, Evenhuis HM, et al. Feasibility and reliability of tests measuring health-related physical fitness in children with moderate to severe levels of intellectual disability. Am J Intellect Dev Disabil. 2017;122:422–438.
- de Onis M, Onyango A, Borgi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:661–668.
- WHO Multicentre Growth Reference Study Group. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization; 2006.
- de Onis M, Lobstein T. Defining obesity risk status in the general childhood population: which cut-offs should we use? Int J Pediatr Obes. 2010;5:458–460.
- Taylor RW, Jones IE, Williams SM, et al. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19 y. Am J Clin Nutr. 2000;72:490–495.
- Fredriks AM, van Buuren S, Fekkes M, et al. Are age references for waist circumference, hip circumference and waist-hip ratio in Dutch children useful in clinical practice? Eur J Pediatr. 2005;164:216–222.
- Aertssen WF, Ferguson GD, Smits-Engelsman BC. Reliability and structural and construct validity of the functional strength measurement in children aged 4 to 10 years. Phys Ther. 2016;96:888–897.
- Aertssen WFM, Steenbergen B, Smits-Engelsman BCM. The validity and reliability of the functional strength measurement (FSM) in children with intellectual disabilities. J Intellect Disabil Res. 2018;62:719–729.
- Smits-Engelsman BCM, Verhoef-Aertssen WFM. Functional Strength Measurement(FSM): Manual. Meteren, the Netherlands: FSM Production; 2012.
- Elmahgoub SS, Van de Velde A, Peersman W, et al. Reproducibility, validity and predictors of six-minute walk test in overweight and obese adolescents with intellectual disability. Disabil Rehabil. 2012;34:846–851.
- Lammers AE, Hislop AA, Flynn Y, et al. The 6 minute walk test: normal values for children of 4–11 years of age. Arch Dis Childhood. 2008;93:464–468.
- Ulrich S, Hildenbrand FF, Treder U, et al. Reference values for the 6 minute walk test in healthy children and adolescents in Switzerland. BMC Pulm Med. 2013;13:49.
- Reilly JJ, Penpraze V, Hislop J, et al. Objective measurement of physical activity and sedentary behaviour: review with new data. Arch Dis Child. 2008;93:614–619.
- Cliff DP, Reilly JJ, Okely AD. Methodological considerations in using accelerometers to assess habitual physical activity in children aged 0–5 years. J Sci Med Sport. 2009;12:557–567.
- Esliger DW, Copeland JL, Barnes JD, et al. Standardizing and optimizing the use of accelerometer data for fee-living physical activity monitoring. J Phys Act Health. 2005;2:366.
- Rich C, Geraci M, Griffiths L, et al. Quality control methods in accelerometer data processing: defining minimum wear time. PLoS ONE. 2013;8:e67206.
- Pearson Education. Technical report. Using the Bayley scales of infant and toddler development. 3rd ed. to assess individuals with severe delays. London: Pearson Education; 2008.
- Schalock RL, Borthwick-Duffy SA, Buntinx WHE, et al. Intellectual disability: definition, classification, and systems of supports. 11th ed. Washington (DC): American Association on Intellectual and Developmental Disabilities; 2010.
- de Bildt AA, Kraijer DW. Vineland-Z, sociale redzaamheidsschaal voor kinderen en jeugdigen met een verstandelijke beperking, handleiding [Vineland-Z, social independence scale for children and adolescents with an intellectual disability, manual]. Leiden, Netherlands: PITS B.V.; 2003.
- Sparrow SS, Balla DA, Cicchetti DV. Vineland adaptive behavior scales. Circle Pines (MN): American Guidance Service; 1984.
- Centraal Bureau voor de Statistiek. Standaarddefinitie allochtonen [Standard definition immigrants]. Voorburg, the Netherlands: Centraal Bureau voor de Statistiek: 2000.
- Field A. Discovering Statistics using SPSS. 2nd ed. London: Sage Publications Ltd; 2005.
- Wouters M, Evenhuis HM, Hilgenkamp TIM. Physical activity levels of children and adolescents with moderate to severe intellectual disability. J Appl Res Intellect Disabil. 2018;32:131–142.
- Schonbeck Y, Talma H, van Dommelen P, et al. Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PLoS One. 2011;6:e27608.
- Casey AF, Rasmussen R. Reduction measures and percent body fat in individuals with intellectual disabilities: a scoping review. Disabil Health J. 2013;6:2–7.
- Gonzalez-Aguero A, Vicente-Rodriguez G, Moreno LA, et al. Health-related physical fitness in children and adolescents with Down syndrome and response to training. Scand J Med Sci Sports. 2010;20:716–724.
- Calders P, Elmahgoub S, Cambier D. Physical and metabolic fitness of children and adolescents with intellectual disability - how to rehabilitate? In: Tan PU, editor. Latest findings in intellectual and developmental disabilities research. London: InTech; 2012.
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7:40.
- Collins K, Staples K. The role of physical activity in improving physical fitness in children with intellectual and developmental disabilities. Res Dev Disabil. 2017;69:49–60.
- Stodden DF, Gao Z, Goodway JD, et al. Dynamic relationships between motor skill competence and health-related fitness in youth. Pediatr Exerc Sci. 2014;26:231–241.
- Stodden DF, Langendorfer SJ, Roberton MA. The association between motor skill competence and physical fitness in young adults. Res Q Exerc Sport. 2009;80:223–229.
- Wrotniak BH, Epstein LH, Dorn JM, et al. The relationship between motor proficiency and physical activity in children. Pediatrics. 2006;118:e1758–e1765.
- Esposito PE, MacDonald M, Hornyak JE, et al. Physical activity patterns of youth with Down syndrome. Intellect Dev Disabil. 2012;50:109–119.
- Andersen LB, Harro M, Sardinha LB, et al. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study). Lancet. 2006;368:299–304.
- Twisk JW, Van Mechelen W, Kemper HC, et al. The relation between “long-term exposure” to lifestyle during youth and young adulthood and risk factors for cardiovascular disease at adult age. J Adolesc Health. 1997;20:309–319.
- Ortega FB, Ruiz JR, Hurtig-Wennlof A, et al. Cardiovascular fitness modifies the associations between physical activity and abdominal adiposity in children and adolescents: the European Youth Heart Study. Br J Sports Med. 2010;44:256–262.
- Must A, Curtin C, Hubbard K, et al. Obesity prevention for children with developmental disabilities. Curr Obes Rep. 2014;3:156–170.
- Ordonez FJ, Rosety M, Rosety-Rodriguez M. Influence of 12 week exercise training on fat mass percentage in adolescents with Down syndrome. Med Sci Monit. 2006;12:CR416–CR419.
- Elmahgoub SM, Lambers S, Stegen S, et al. The influence of combined exercise training on indices of obesity, physical fitness and lipid profile in overweight and obese adolescents with mental retardation. Eur J Pediatr. 2009;168:1327–1333.
- Giagazoglou P, Kokaridas D, Sidiropoulou M, et al. Effects of a trampoline exercise intervention on motor performance and balance ability of children with intellectual disabilities. Res Dev Disabil. 2013;34:2701–2707.
- Fotiadou EG, Neofotistou KH, Giagazoglou PF, et al. The effect of a psychomotor education program on the static balance of children with intellectual disability. J Strength Cond Res. 2017;31:1702–1708.
- Lee K, Lee M, Song C. Balance training improves postural balance, gait, and functional strength in adolescents with intellectual disabilities: single-blinded, randomized clinical trial. Disabil Health J. 2016;9:416–422.
- Lotan M, Isakov E, Kessel S, et al. Physical fitness and functional ability of children with intellectual disability: effects of a short-term daily treadmill intervention. ScientificWorldJournal. 2004;4:449–457.
- Lotan M, Isakov E, Merrick J. Improving functional skills and physical fitness in children with Rett syndrome. J Intellect Disabil Res. 2004;48:730–735.
- Shin JY, Nhan NV, Lee SB, et al. The effects of a home-based intervention for young children with intellectual disabilities in Vietnam. J Intellect Disabil Res. 2009;53:339–352.
- Bishop JC, Pangelinan M. Motor skills intervention research of children with disabilities. Res Dev Disabil. 2018;74:14–30.
- Lin JD, Lin PY, Lin LP, et al. Physical activity and its determinants among adolescents with intellectual disabilities. Res Dev Disabil. 2010;31:263–269.
- Draheim CC, Williams DP, McCubbin JA. Prevalence of physical inactivity and recommended physical activity in community-based adults with mental retardation. Ment Retard. 2002;40:436–444.
- Pitetti KH, Fernhall B. Comparing run performance of adolescents with mental retardation, with and without Down syndrome. Adapt Phys Act Q. 2004;21:219–228.
- McMurray RG, Harrell JS, Deng S, et al. The influence of physical activity, socioeconomic status, and ethnicity on the weight status of adolescents. Obes Res. 2000;8:130–139.
- Labree LJ, van de Mheen H, Rutten FF, et al. Differences in overweight and obesity among children from migrant and native origin: a systematic review of the European literature. Obes Rev. 2011;12:e535–e547.
- Fernhall B, Mendonca GV, Baynard T. Reduced work capacity in individuals with Down syndrome a consequence of autonomic dysfunction? Exerc Sport Sci Rev. 2013;41:138–147.
- Wilmore JH, Costill DL, Kenney WL. Physiology of sport and exercise. 4th ed. Champaign (IL): Human Kinetics Publishers; 2008.