Abstract
Objective: To observe upper limb activity patterns of people with stroke during sub-acute rehabilitation to inform the development of treatment strategies for upper limb rehabilitation. Design: Observational study of upper limb activity. Methods: Twenty participants admitted for sub-acute rehabilitation following stroke were observed during a week day for 1 minute every 10 min between 7 am and 7 pm. Upper limb activity was recorded and categorized into five types of movement. Results: Participants used either one or both upper limbs for 45.8% of the observation time. The affected arm moved 26.4% of the time, with most movement occurring in conjunction with the unaffected arm (18.9% of the time) and only 7.5% of the time being movement of the affected arm by itself. The largest proportion of upper limb activity was observed during mealtimes. Conclusions: Recognition of the need to improve upper limb outcomes after stroke has not yet translated into changes in the amount of upper limb activity undertaken during sub-acute rehabilitation. Opportunities to rehabilitate the hemiplegic upper limb are not fully realized. The dominance of bilateral movement in the early stages after stroke may provide scope for interventions that maximize this aspect of motor control.
Despite advances in rehabilitation, time spent in upper limb activity following stroke is very low, particularly in the affected arm.
Most movement of the affected arm occurs in conjunction with the unaffected arm.
There is an urgent need to redress this low level of movement, given the importance of upper limb recovery to quality of life for people following stroke.
IMPLICATIONS FOR REHABILITATION
Introduction
Despite advances in understanding of upper limb recovery after stroke, 80% of stroke survivors still present with reduced upper limb function which impacts independence, quality of life, and mood [Citation1]. The extent of upper limb recovery in the acute stage post-stroke plays a vital role in determining discharge destination, independence, and return to life roles [Citation2].
Maximizing recovery is an ongoing challenge for stroke rehabilitation providers, with research demonstrating a window of 3–4 weeks for optimum neural repair, compensation, and neural plasticity [Citation3]. Higher dose of upper limb therapy in this sub-acute stage is associated with improved functional outcomes [Citation4,Citation5]. However, providers prioritize early discharge with rehabilitation provision focused on independent and safe mobility in order to meet the high demand for inpatient beds [Citation6]. This coupled with the individual’s goal to prioritize mobility means that upper limb rehabilitation receives less attention [Citation7]. Notwithstanding the need to enhance mobility and ensure safety, this focus is likely to impact on post-stroke outcomes [Citation8].
Failure to meet the challenge of early upper limb rehabilitation has been documented. Using observational techniques, Bernhardt et al. found very low levels of upper limb activity during waking hours, with no movement for 67% of the day [Citation9]. Other observational studies consistently record no upper limb activity for up to 80% of the day [Citation9–12]. In the past decade, rehabilitation strategies such as exercise groups, enriched environments, and interactive video games have been developed to promote upper limb activity. Similarly, clinicians now have more evidence to support the provision of task-specific, intensive, high-dose upper limb rehabilitation to promote upper limb recovery [Citation13,Citation14]. However, the impact of recent knowledge on the amount of upper limb rehabilitation offered in the acute stages is unknown. The most recent study by Bernhardt et al. [Citation15] is now more than a decade ago, and practice may have improved to incorporate a stronger focus on upper limb rehabilitation. This observational study aims to describe the amount and type of upper limb activity over 12 h in people after stroke residing in a sub-acute rehabilitation setting. We categorized movement into five groups to identify the proportion of time in which the affected and non-affected limbs move independently and together. We also examined the effect of mealtimes on amount of upper limb movement.
Methods
Participants
All people with stroke admitted to the rehabilitation service between August 2015 and Jan 2016 were considered for inclusion in the study. Participants were included if they had a confirmed diagnosis of stroke according to standard diagnostic criteria [Citation16], presented with upper limb deficit as a result of their stroke; were declared medically stable and fit for rehabilitation by a medical consultant; and provided informed written consent. Participants were excluded if they had cognitive, behavioural or communication impairments that in the opinion of the research team (RM, DT, NS) limited their ability to provide consent and participate in the research; were within three days of planned discharge from inpatient rehabilitation; and/or reported shoulder pain.
Potential participants were identified and referred to the research team by the rehabilitation ward therapist. They were then informed about the study, and screened according to the inclusion and exclusion criteria. Eligible participants provided written informed consent and identified a mutually agreeable day for data collection. Each participant was observed over a single weekday. Movements were manually recorded by a trained observer on an upper limb taxonomy for 1 min every 10 min from 07:00 h to 19:00 h. Each minute of observation was broken into 6, 10-second blocks using a silent interval timer.
Each participant was followed discretely by the observer around the rehabilitation ward, therapy areas, and hospital facilities where feasible for the duration of the observation period. The observer positioned themselves inconspicuously, out of the field of view of the participant. When patients were not able to be directly observed (i.e., due to curtains being drawn or whilst in showers and toilets) activity was recorded after conferring with the participant, staff or family members as appropriate. In circumstances where the activity could not be estimated, such as during four randomly scheduled observer breaks, activity was coded as unobserved. Approval for the study was obtained from Health and Disability Ethics Committee, New Zealand (approval number 16/NTA/74).
Development of the upper limb taxonomy
The upper limb taxonomy and observation protocol were developed from work by Bernhardt et al. [Citation10]. To fully explore upper limb movement each 10 s epoch within the observed minute was coded into one of five categories: (1) unilateral affected upper limb movement (AU), (2) unilateral unaffected upper limb movement (UU), (3) bimanual movement (BiM) where movement of both upper limbs was observed to achieve a common task or purpose, (4) bilateral limb movement (BiL) where movement of both upper limbs was observed to achieve independent or unrelated tasks, and (5) no movement (No).
Observer training
Prior to data collection, all observers (n = 5) undertook five hours training with the upper limb taxonomy using video recordings of people with stroke. After training observers were tested against each other until inter- and intra-rater agreement was higher than 90% across 20 observations.
Measures
Demographic, clinical, and medical information was gathered from the medical record of consenting participant by their rehabilitation ward therapist. Data included; age, sex, ethnicity, date of stroke, type of stroke, side of body most affected, dominant hand prior to stroke, date of admission to the rehabilitation ward, estimated date of discharge, comorbidities, and medications.
Data analysis
Coded data were entered into a Microsoft Excel spreadsheet (Microsoft Corporation, Redmond, WA, USA). Type of movement was defined based on the five movement categories previously described. Total limb activity was collated based on all observations in which the limb had moved. For example, affected limb activity included AU + BiM + BiL categories, and unaffected limb activity included UU + BiM + BiL. Descriptive analysis was used to examine total amount of limb activity and type of movement.
Estimation of the variation of upper limb activity was computed using generalized linear mixed models (GLMM) with a logistic link function. Six such models were derived, one for each binary dependent variable: total affected limb activity, AU only, total unaffected limb activity, UU only, any upper limb activity (AU, UU, BiM, or BiL), and BiM and BiL combined. A smooth model was fitted to the data by fitting a natural spline that used one degree of freedom per hour as a clinically meaningful timeframe. To account for correlated repeated measures, each model included hierarchical random effects per participant and per hour within participant. The correlation structure was chosen using Akaike Information Criterion (AIC) from a collection of structures that included longer and shorter time spans and splines of varying flexibility. Time periods of high or low activity were derived from a fitted curve where the top and bottom 20% of values occurred (thresholding). The effect of meal times was tested by adding a single fixed effect term to the above model to estimate the effect as an odds ratio. The statistics package lme4 was used to analyze data [Citation17].
Results
Participant characteristics
A total of 21 people consented to participate in the study. One participant was unexpectedly discharged early and did not start data collection. The participants’ median age was 82 years and the median number of days since stroke was 13.5. The proportions of participants with left- and right-sided hemiparesis were similar, and for nine participants (45%) the affected limb was also their dominant upper limb. No participant had hemorrhagic stroke. The average length of stay for a patient was 18.3 days ().
Table 1. Participant characteristics.
Rehabilitation environment
The rehabilitation service receives referrals for older adults following medical, orthopedic, and neurological events. Facilities include two wards, a rehabilitation gym, outdoor spaces, and purpose-built activity of daily living training spaces such as a kitchen and bathroom, all on one level linked by corridors. The two wards include 12 × four-bed, 5 × two-bed, and 6 × single-bed rooms along with communal lounge and dining areas. Ten beds are specifically designated for people with stroke. The service provides interdisciplinary rehabilitation with staff to patient ratios of: nurses 1:5 in the morning and 1:6 in the afternoon, physiotherapists 1:9 and occupational therapists 1:10, social workers 1:26, and rehabilitation assistants 1:18. Speech language therapy is available on referral. Therapists work a 5-day week between the hours of 07:30 and 16:00 or 08:00 and 16:30. Scheduled meal times occur from 08:00 to 08:30, 12:00 to 13:00, and 17:00 to 17:30, and visiting hours are 08:00–20:00.
Observational data
A total of 8143 observations of movement within 10-s time intervals were recorded across the 20 participants (median = 408, IQR = 399–406), representing data completeness of 94.4%. Data loss was predominantly due to the participant being away from the service for appointments or being involved in private personal hygiene activities.
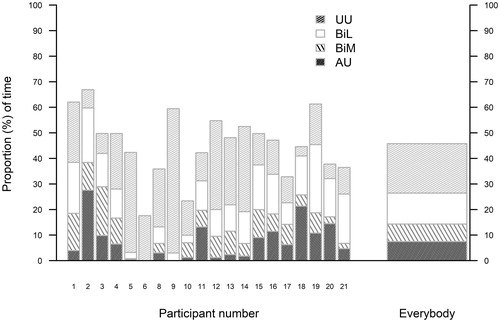
The affected arm moved 26.4% of the time, with most movement occurring in conjunction with the unaffected arm (18.9% of the time) and only 7.5% of the time being movement of the affected arm by itself (). The unaffected arm moved 38.3% of the time with half this movement (19.3% of the time) being movement of the unaffected arm by itself. Participants used either one or both upper limbs for 45.8% of the observation time.
Activity levels across the day
shows movement across the 12-h period illustrating variation in upper limb activity. Odds ratios for the effect of meal times on upper limb activity were not statistically significant ().
Figure 2. Spline analysis of UL activity with 95% confidence bands. Time periods containing the top 20% and bottom 20% of activity are lightly shaded. (UU: unaffected upper limb movement; BiL: Bilateral movement; BiM: bimaual movement; AU: affected upper limb movement)
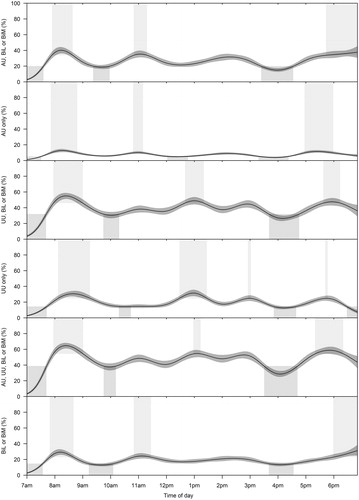
Table 2. Effect of meal time on three mutually-exclusive upper limb movement categories.
Using the threshold of 20%, peak activity was identified in the morning between 08:06 and 08:38, and in the early evening for all movement types. Peak movement was also seen in AU, but not UU mid-morning between 10:48 and 11:09. There was a peak of activity between 12:40 and 13:20 for UU and UU, BiL, or BiM but not for analysis of AU or AU, BiL, or BiM. Troughs of activity were seen in all movement types in the early morning 07:00–07:30 and late afternoon 15:40–16:22. Times reported above are the timeframes when thresholds overlapped for the specified conditions.
Discussion
To our knowledge, this study is the first observational study to exclusively focus on movement of the upper limbs during inpatient rehabilitation following stroke. Our findings indicate that 10 years on from the pioneering observational study by Bernhardt et al. [Citation9] the affected upper limb moves very little during a typical rehabilitation day and that for large portions of the day people with stroke do not engage in any activity of the upper limbs. For over half the observed day they did not engage in activity of either upper limb. The amount of upper limb activity was slightly higher than the study by Bernhardt et al. [Citation9]. Our data collection protocol differed from the Bernhardt et al.’s [Citation9] study in that we had 6 epochs of observation in each minute compared to just one, thus increasing the richness of the data. A further important difference was the timing of the research and the hours of observation. This study was carried out later post-stroke (on average 13.5 days vs. 5.6 days) and included a longer observation window (7 am–7 pm vs. 8 am–5 pm), encapsulating the morning and evening meals, and self-care activities. Other differences were that our focus was on upper limb movement rather than both upper and lower limb activity, and we documented all activities during that minute (not just the highest ranked movement). Whilst other studies have reported lower levels of upper limb activity using behavioural mapping techniques, these studies are limited by small sample sizes [Citation12,Citation18], limited classification of upper limb activity [Citation12,Citation18,Citation19], and failure to fully report the results of UL observation [Citation12].
In healthy adults, the ratio of activity between the non-dominant and dominant upper limbs during everyday activity is approximately 0.95 [Citation20–23]. In this study, irrespective of dominance, the ratio of activity between affected and unaffected upper limb was 0.69, which is higher than previous reports in people with sub-acute stroke of 0.24 [Citation18], 0.54 [Citation9], and 0.55 [Citation20]. For people with stroke living in the community, ratios of 0.45 [Citation22] and 0.65 [Citation23] have been reported. Comparisons of ratios are problematic because of methodological differences, including time since stroke, the extent of UL disability, and the amount of rehabilitation received. However it is clear that the ratio of affected to unaffected UL use is reduced following stroke and that being in an inpatient rehabilitation setting does not appear to promote use of the affected UL.
This study illustrates the opportunities to promote affected upper limb activity. Whilst there was very limited movement in the affected upper limb across the day, movement was more likely to occur in that limb during mealtimes when the unaffected arm was also moving. Upper limb activity was higher during the evening meal period compared to lunch time. As we did not collect specific data regarding the exact timing of meals for individual participants, this may reflect the nature of the task, where finger foods are more likely to be served at lunch, or it may be due to the more flexible scheduling of this meal. Collectively these findings suggest that eating may promote increased activity in the affected upper limb. Whether this reflects the opportunity to do something meaningful and rewarding with the upper limbs or is simply a function of the task itself is unclear. Movement in the affected upper limb was also increased in a window during the mid-morning, it is not clear whether this reflects morning tea or is a therapeutic influence where patients are more likely to be engaged in face-to-face rehabilitation at this time.
A number of implications for staff and carers involved in sub-acute, post-stroke rehabilitation arise from the results of this study. First, the benefit of building on functional movement strategies to increase the time spent in upper limb movement. Because most movement of the hemiplegic upper limb is done in concert with the unaffected limb, there may be benefit in focussing on bilateral or bimanual tasks in therapy time. Timing is also important. Given the relatively low periods of activity in the mid-morning and mid-afternoon, it is highly relevant to provide opportunities for exercise and activity targeted during these times. The paucity of time spent with a therapist is well documented and a challenge for upper limb recovery. Most patients participate directly in therapy sessions for less than an hour a day, with an average of 4–11 min allocated to upper limb rehabilitation [Citation9,Citation15]. This indicates the need for programmes that encourage independent exercise and activity outside direct therapy hours. Technology may advance this goal, through provision of enriched rehabilitation environments such as computerized games, virtual reality programmes, and robotic devices. Technology may also drive changes in the measurement of activity. Through the use of body-worn sensors, the amount and type of upper limb movement can be recorded continuously, independent of observers [Citation24,Citation25]. Monitoring such as this would inform therapists and promote the development of personalized methods of increasing daily activity levels.
A key strength to this study is that we observed almost all 1 minute observation blocks of a 12 h day and in contrast to some earlier reports, we annotated all movement. Other strengths include our sample size which was comparable to earlier work. We undertook preliminary training with the observers to ensure data accuracy, and we modelled the data to enable a clear and nuanced interpretation of the effect of variation on upper limb movement. Limitations to the study include a lack of data regarding specific therapy time and ward activities, particularly in light of the finding that upper limb movements around mealtimes may offer a therapeutic window. Other limitations include the lack of measure of spasticity and the exclusion of people with shoulder pain. Due to the nature of the study, participants were aware that they were being observed and this may have influenced their behaviour.
In conclusion, time spent in upper limb activity following stroke is very low and comparable to reports published over a decade ago [Citation9]. There is an urgent need to address this failing, given the importance of upper limb recovery to quality of life for people following stroke.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Morris JH, van Wijck F, Joice S, et al. Predicting health related quality of life 6 months after stroke: the role of anxiety and upper limb dysfunction. Disabil Rehabil. 2013;35:291–299.
- Veerbeek JM, Kwakkel G, van Wegen EEH, et al. Early prediction of outcome of activities of daily living after stroke: a systematic review. Stroke. 2011;42:1482–1488.
- Buma F, Kwakkel G, Ramsey N. Understanding upper limb recovery after stroke. Restor Neurol Neurosci. 2013;31:707–722.
- Han C, Wang Q, Meng PP, et al. Effects of intensity of arm training on hemiplegic upper extremity motor recovery in stroke patients: a randomized controlled trial. Clin Rehabil. 2013;27:75–81.
- Kwakkel G, van Peppen R, Wagenaar RC, et al. Effects of augmented exercise therapy time after stroke: a meta-analysis. Stroke. 2004;35:2529–2539.
- De Wit L, Putman K, Lincoln N, et al. Stroke rehabilitation in Europe: what do physiotherapists and occupational therapists actually do? Stroke. 2006;37:1483–1489.
- Hayward KS, Brauer SG. Dose of arm activity training during acute and subacute rehabilitation post stroke: a systematic review of the literature. Clin Rehabil. 2015;29:1234–1243.
- Poltawski L, Allison R, Briscoe S, et al. Assessing the impact of upper limb disability following stroke: a qualitative enquiry using internet-based personal accounts of stroke survivors. Disabil Rehabil. 2016;38:945–951.
- Bernhardt J, Chan J, Nicola I, et al. Little therapy, little physical activity: rehabilitation within the first 14 days of organized stroke unit care. Acta Derm Venereol. 2007;39:43–48.
- Bernhardt J, Dewey H, Thrift A, et al. Inactive and alone: physical activity within the first 14 days of acute stroke unit care. Stroke. 2004;35:1005–1009.
- Janssen H, Ada L, Bernhardt J, et al. Physical, cognitive and social activity levels of stroke patients undergoing rehabilitation within a mixed rehabilitation unit. Clin Rehabil. 2014;28:91–101.
- Thompson R, McKinstry W. How do rehabilitation patients spend their days? An investigation into the effect of a group therapy programme on time use. NZJP. 2009;37:122–126.
- Wolf SL, Kwakkel G, Bayley M, et al. Best practice for arm recovery post stroke: an international application. Physiotherapy. 2016;102:1–4.
- Ward NS, Kelly K, Brander F. The future of stroke rehabilitation: upper limb recovery. ACNR. 2015;15:6–7.
- Bernhardt J, Chitravas N, Meslo IL, et al. Not all stroke units are the same: a comparison of physical activity patterns in Melbourne, Australia, and Trondheim, Norway. Stroke. 2008;39:2059–2065.
- Stroke Foundation of New Zealand Guidelines Group. Clinical guidelines for stroke management. Wellington, New Zealand: Stroke Foundation of New Zealand; 2010.
- Bates D, Maechler M, Bolker B, et al. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48.
- King A, McCluskey A, Schurr K. The time use and activity levels of inpatients in a co-located acute and rehabilitation stroke unit: an observational study. Top Stroke Rehabil. 2011;18:654–665.
- Esmonde T, McGinley J, Wittwer J, et al. Stroke rehabilitation: patient activity during non-therapy time. Aust J Physiother. 1997;43:43–51.
- Lang CE, Wagner JM, Edwards DF, et al. Upper extremity use in people with hemiparesis in the first few weeks after stroke. J Neurol Phys Ther. 2007;31:56–63.
- Bailey RR, Lang CE. Upper-limb activity in adults: referent values using accelerometry. J Rehabil Res Dev. 2013;50:1213–1222.
- Michielsen ME, Selles RW, Stam HJ, et al. Quantifying nonuse in chronic stroke patients: a study into paretic, nonparetic, and bimanual upper-limb use in daily life. Arch Phys Med Rehabil. 2012;93:1975–1981.
- Bailey RR, Klaesner JW, Lang CE. Quantifying real-world upper-limb activity in nondisabled adults and adults with chronic stroke. Neurorehabil Neural Repair. 2015;29:969–978.
- Doman CA, Waddell KJ, Bailey RR, et al. Changes in upper-extremity functional capacity and daily performance during outpatient occupational therapy for people with stroke. Am J Occup Ther. 2016;70:7003290040p1–700329004p11.
- van der Pas SC, Verbunt JA, Breukelaar DE, et al. Assessment of arm activity using triaxial accelerometry in patients with a stroke. Arch Phys Med Rehabil. 2011;92:1437–1442.